Published online Feb 28, 2014. doi: 10.3748/wjg.v20.i8.2079
Revised: October 25, 2013
Accepted: November 3, 2013
Published online: February 28, 2014
Processing time: 152 Days and 21.8 Hours
AIM: To validate whether the platelet count/spleen size ratio can be used to predict the presence of esophageal varices in Mexican patients with hepatic cirrhosis.
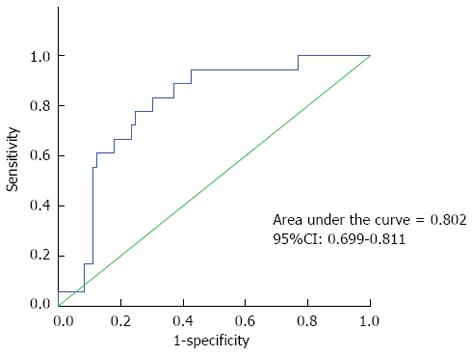
METHODS: This was an analytical cross-sectional study to validate the diagnostic test for hepatic cirrhosis and was performed between February 2010 and December 2011. Patients with a diagnosis of hepatic cirrhosis were included and stratified using their Child-Pugh score. Biochemical parameters were evaluated, and ultrasound was used to measure the longest diameter of the spleen. The platelet count/spleen diameter ratio was calculated and analyzed to determine whether it can predict the presence of esophageal varices. Upper gastrointestinal endoscopy was used as the gold standard. Sensitivity and specificity, positive and negative predictive values, and positive and negative likelihood ratios were determined, with the cutoff points determined by receiver-operating characteristic curves.
RESULTS: A total of 91 patients were included. The mean age was 53.75 ± 12 years; 50 (54.9%) were men, and 41 (45.0%) women. The etiology of cirrhosis included alcohol in 48 (52.7%), virally induced in 24 (26.3%), alcoholism plus hepatitis C virus in three (3.2%), cryptogenic in nine (9.8%), and primary biliary cirrhosis in seven (7.6%). Esophageal varices were present in 73 (80.2%) patients. Child-Pugh classification, 17 (18.6%) patients were classified as class A, 37 (40.6%) as class B, and 37 (40.6%) as class C. The platelet count/spleen diameter ratio to detect esophageal varices independent of the grade showed using a cutoff value of ≤ 884.3, had 84% sensitivity, 70% specificity, and positive and negative predictive values of 94% and 40%, respectively.
CONCLUSION: Our results suggest that the platelet count/spleen diameter ratio may be a useful tool for detecting esophageal varices in patients with hepatic cirrhosis.
Core tip: Using noninvasive parameters for high-risk esophageal varices may reduce the need for endoscopies. The ratio of platelet count/diameter of the spleen (PC/SD ratio) is the principal noninvasive predictor of esophageal varices for stratifying patients with cirrhosis. These parameters are easy to obtain, reproducible and noninvasive. In our study, the cutoff point for PC/SD ratio was lower than that reported in previous literature (< 884.3 and < 909, respectively), with a sensitivity of 84% and specificity of 70%. The differences are probably influenced by racial characteristics. The PC/SD ratio should be considered to identifying patients with esophageal varices.
- Citation: González-Ojeda A, Cervantes-Guevara G, Chávez-Sánchez M, Dávalos-Cobián C, Ornelas-Cázares S, Macías-Amezcua MD, Chávez-Tostado M, Ramírez-Campos KM, Ramírez-Arce ADR, Fuentes-Orozco C. Platelet count/spleen diameter ratio to predict esophageal varices in Mexican patients with hepatic cirrhosis. World J Gastroenterol 2014; 20(8): 2079-2084
- URL: https://www.wjgnet.com/1007-9327/full/v20/i8/2079.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i8.2079
Portal hypertension is the principal complication of hepatic cirrhosis[1]. More than 80% of patients with cirrhosis will develop esophageal varices at some point, and 30% of these patients will have at least one bleeding episode because of rupture of a varix[2]. Most first bleeding episodes happen during the first year after the detection of the varices, with a 5%-10% mortality attributed to the initial hemorrhage[3]. For this reason, identifying the presence of esophageal varices is a fundamental part of the diagnostic work-up in patients with cirrhosis, and it is also a prognostic marker of the illness. The first crucial preventive step is the identification of those patients with bleeding risk and selection for prophylactic treatment.
Today’s guidelines are clear that there are no substitute markers to determine the presence and size of esophageal varices, and endoscopy is still the only valid method to investigate varices[4]. However, access to endoscopy and other resources is limited in some countries. At any given time, a variable proportion of patients will not have varices, and the reported prevalence of esophageal varices is 24%-80%[5]. The use of noninvasive methods to predict the presence of esophageal varices would help restrict endoscopic studies to those with a high probability of having varices. Until a few years ago, little information was available on this subject; however, a recent consensus on the definitions, methodology, and therapeutic strategies in portal hypertension[6] recommended that all patients with cirrhosis should be assessed with endoscopy to verify the presence of varices.
Recent studies[7-11] have emphasized the use of noninvasive methods to identify patients with the intention of avoiding endoscopy in low-risk cases. The fact that distinct predictors of the presence of varices have been identified in different studies probably reflects differences between the study populations and spectrum of the disease and this makes it difficult to develop a widely applicable predictive model.
Giannini et al[12] proposed the use of the platelet count (PC)/spleen diameter (SD) ratio as a noninvasive tool for predicting the presence of varices. The use of the PC/SD ratio for the noninvasive assessment of varices seems to meet strict methodological criteria and is based on pathophysiological criteria. The diagnostic precision of this parameter was validated using endoscopic diagnosis in a follow-up of patients free of esophageal varices[13].
The preliminary results obtained by other authors have demonstrated that the diagnostic accuracy of the PC/SD ratio is maintained in patient subgroups with different hepatic disease etiologies and when applying different methodologies[14], suggesting the universality of the diagnostic method. However, no studies have confirmed the results of these earlier studies in the Mexican population. Previous studies were performed in Caucasian populations, and the ratio may differ between populations. Thus, different predictive values may be needed to indicate the presence of esophageal varices. The objective of our study was to validate the PC/SD ratio as a predictor of the presence and absence of esophageal varices in Mexican patients with chronic hepatopathy.
This study was an analytical cross-sectional validation study of a diagnostic test. Patients were included from the Department of Enteral and Parenteral Nutrition, Gastroenterology Service, Hospital Civil de Guadalajara “Fray Antonio Alcalde.” The inclusion criteria were a diagnosis of hepatic cirrhosis by histology or physical, biochemical, and imaging examinations compatible with the disease and treatment from February 1, 2010 to December 31, 2011.
Both men and women with a diagnosis of hepatic cirrhosis of any etiology were included. The exclusion criteria were hepatocellular carcinoma, use of medications for the primary prophylaxis of variceal bleeding, history of esophageal variceal bleeding, alcohol consumption within the admission and a history of ligation, sclerotherapy, and/or portal hypertension surgery.
Once the patients were included in the study, a complete medical history was taken, and biochemical parameters were measured. All patients were classified according to their Child-Pugh grading.
To calculate the PC/SD ratio, a blood count and PC was obtained using a CELL-DYN 3700 automated hematology analyzer (Abbott Laboratories, Abbott Park, IL, United States) Afterwards, the patient underwent an upper abdominal echographic examination using a GE Logiq P5 ultrasound system (General Electric Company, Fairfield CT, United States); the spleen’s longest diameter was measured in millimeters.
The PC/SD ratio was calculated by dividing the number of platelets/μL by the maximum bipolar diameter of the spleen in millimeters, estimated with abdominal ultrasound. Normal values in healthy mexican adults are: Maximum bipolar diameter of 115-130 mm and platelet count of 167000-431000/mm3[15].
Finally, the patient received a upper gastrointestinal endoscopy to determine the presence and grade of esophageal varices according to Westaby’s grading system. All endoscopies were performed using one endoscopy unit and an Olympus GIF-Q150 gastrointestinal videoscope (Olympus Corporation, Tokyo, Japan). The endoscopy and echography operators were blinded to the biochemical parameters. The interobserver variation coefficients for spleen measurements and presence of varices were evaluated in all the patients (1.4% and 1.2%, respectively).
The study was conducted according to the principles of the Declaration of Helsinki (1989) and the Mexican Health Guidelines. Full written informed consent was obtained from all patients before their inclusion in the study. The protocol was approved by the Local Research Committee of the Hospital Civil de Guadalajara “Fray Antonio Alcalde” (registry number, 138/09).
The results are expressed as frequencies, average percentages, and standard deviations. Student’s t test was used to compare the quantitative variables. The test validity was determined with sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive and negative likelihood ratios (LR+ and LR-) of the PC/SD ratio. The statistical analysis was performed using SPSS for Windows version 17.0 (SPSS Inc., Chicago, IL, United States).
A total of 91 patients with hepatic cirrhosis were included. Forty-one (45%) were women, and 50 (54.9%) were men. The average age was 53.75 ± 12 years. The most common hepatic cirrhosis etiology was alcoholism in 48 (52.7%) patients, followed by hepatitis C virus (HCV) in 24 (26.3%), no hepatitis B virus cirrhosis were included, alcoholism plus HCV in three (3.2%), cryptogenic in nine (9.8%), and primary biliary cirrhosis in seven (7.6%).
In the Child-Pugh classification, 17 (18.6%) patients were classified as class A, 37 (40.6%) as class B, and 37 (40.6%) as class C. During the endoscopic procedure, esophageal varices were detected in 73 patients (Table 1).
| Characteristics | Value |
| Patients (n) | 91 (100) |
| Age (yr) | 53.75 ± 12 |
| Cirrhosis etiology | |
| Alcoholism | 48 (52.7) |
| Viral hepatitis | 24 (26.3) |
| Viral hepatitis + alcoholism | 3 (3.2) |
| Other | 16 (17.5) |
| Grading of varices | |
| I | 21 (23) |
| II | 30 (32.9) |
| III | 22 (24.1) |
| Child–Pugh classification | |
| A | 17 (18.6) |
| B | 37 (40.6) |
| C | 37 (40.6) |
The average PC/SD ratios were 824.56 ± 412.27 and 1390 ± 905.49 (P = 0.018) for patients who showed evidence of esophageal varices during the endoscopy and in those who did not, respectively. The respective PCs were 117517 ± 50275/μL and 175788 ± 88448/μL (P = 0.014). The respective SD values were 148.16 ± 21.88 mm and 130.61 ± 14.41 mm (P = 0.002) (Table 2).
| EV present | EV absent | P value1 | |
| Platelets/μL | 117517 ± 50275 | 175788 ± 88448 | 0.014 |
| SD (average mm) | 148.16 ± 21.88 | 130.61 ± 14.41 | 0.002 |
| PC/SD ratio | 824.56 ± 412.27 | 1390 ± 905.49 | 0.018 |
The PC/SD ratio to detect esophageal varices independent of the grade showed that a value of 884 for the cutoff point had an 84% sensitivity, 70% specificity, 94% PPV, 40% NPV, 4.13 LR+, and 0.37 LR-. The exactitude was 0.72 (Table 3, Figure 1).
| EV present | EV absent | |
| Cutoff ratio of ≤ 884 vs > 884 | 73 | 18 |
| Sensitivity | 84% | |
| Specificity | 70% | |
| Positive predictive value | 94% | |
| Negative predictive value | 40% | |
| Positive likelihood ratio | 4.1 | |
| Negative likelihood ratio | 0.37 | |
According to Westby’s classification, 21 (23%) patients had grade I varices, 30 (32.9%) had grade II varices, and 22 (24.1%) had grade III varices. The intra- and interobserver variation coefficients for the spleen bipolar measurement were evaluated in all 91 patients using the kappa index (1.2 and 0.98, respectively).
There is an ever-growing demand for endoscopic studies, and the capacity to satisfy this demand is limited, especially in developing countries. It is difficult to provide endoscopy for the detection of esophageal varices every year or two in high-risk patients. Finding noninvasive parameters associated with high-risk esophageal varices may help reduce the need for endoscopy, and, above all, lower the cost. These parameters could be used to distinguish between high- and low-risk patients; the high-risk patients could then be followed up with endoscopic examinations.
The principal noninvasive predictor of esophageal varices may be the PC/SD ratio because it has high sensitivity and specificity in patients with hepatic cirrhosis. This ratio could represent an acceptable parameter of clinical relevance in patients with portal hypertension[12,13,16,17].
We tried to validate whether a simple score could predict the presence of esophageal varices in mexican patients with hepatic cirrhosis of any etiology. Large-scale assessment that takes into account the etiology of cirrhosis is needed to define the role of the PC/SD ratio and to compare the diagnostic exactitude of this ratio with that of other noninvasive parameters. At present, the available data do not support the substitution of another method for upper gastrointestinal endoscopy when identifying esophageal varices, but the PC/SD ratio may be helpful for stratifying patients with cirrhosis into different risk categories. This may be especially relevant to those whose general health conditions do not permit the use of an invasive study, but whose history suggests the possibility of esophageal varices, thus reducing the number of endoscopies.
A large number of patients undergo an endoscopic study to diagnose chronic hepatic illness, and there is a particular interest in finding noninvasive predictors of esophageal varices that could replace the need for scrutinizing endoscopies and thus lower the economic, medical, and social costs[1-12,14,18].
Particular groups of patients have been studied, for example, patients waiting for a liver transplant[18]. In some cases, there is no uniformity in the classification of the varices, or the statistical analysis has been inadequate, and most studies have a retrospective design. In the literature, a low PC and splenomegaly are the most studied noninvasive predictors of esophageal varices, and these parameters produce better results than do parameters such as serum bilirubin and albumin levels, Child-Pugh functional classification, and portal vein diameter[9-12,18-20].
In our study, the analysis of the noninvasive predictors was based on the maximum diameter of the spleen, measured in millimeters using abdominal ultrasound, and the PC. These two parameters were used to calculate the PC/SD ratio. A cutoff point of ≤ 884 produced a sensitivity and specificity of 84% and 70%, respectively.
These results are similar to those of a recent meta-analysis[21], that included 1275 patients and reported a sensitivity of 89% (95%CI: 87-92) and specificity of 74% (95%CI: 70-78). These parameters are easy to obtain, reproducible, and above all, noninvasive. Another advantage is that no additional expense is involved because these studies are performed routinely in patients with hepatic cirrhosis.
The cutoff point for the PC/SD ratio in our study was lower than that reported by Giannini et al[16] (< 884.3 and < 909, respectively). This difference is probably influenced by racial characteristics. The higher values in the study by Giannini et al[16] were obtained from studies of a principally Caucasian population; the patients were taller than in our population and therefore had larger internal organs. The patient population included in our study is representative of the population with hepatic cirrhosis who have signs of portal hypertension seen in clinical practice. The difference in PC/SD ratio between our study and previous studies indicate that it is important to determine a cutoff point for the PC/SD ratio in any specific population.
Thrombocytopenia can be caused by splenic sequestration or by a decrease in hepatic production of thrombopoietin caused by a failing liver and antibody platelet destruction[1-4,9-11,18]. Some authors who have evaluated noninvasive parameters in the diagnosis of esophageal varices have found that splenomegaly can have a high sensitivity but a low specificity, whereas thrombocytopenia shows the opposite, that is, a low sensitivity and intermediate specificity. In the study by Chalasani et al[22], the PC and splenomegaly independently predicted the presence of esophageal varices. In the study by Madhotra et al[8], 32% of the patients had a PC < 68000/μL without splenomegaly. These differences may reflect differences in the etiology of cirrhosis, action of immunological mediators, or reduction in thrombopoietin and not just splenic sequestration[4,11].
The positive predictive value (or the proportion of patients with a positive test result who have the disease) was 94%, but the negative predictor value (or the proportion of people with a negative test results who do not have the disease) was 40% as a reflection of our specificity (70%), the prevalence of esophageal varices in patients in cirrhosis and the different etiologies of the chronic liver diseases.
The use of the PC/SD ratio will help create a lower-cost and more effective method to identify esophageal varices in patients with portal hypertension. The ideal tool should have high sensitivity and specificity as close as possible to 100% to obtain an accurate profile a high-security profile and to avoid the need for endoscopy in patients without esophageal varices. The PC/SD ratio should be considered when identifying patients with a high risk of developing esophageal varices.
In conclusion, the PC/SD ratio cannot substitute for upper gastrointestinal endoscopy in the scrutiny of esophageal varices. However, this ratio can be a useful noninvasive method for identifying patients with esophageal varices and thereby may help reduce the number of unnecessary endoscopies.
Portal hypertension is the principal complication of hepatic cirrhosis. More than 80% of patients with cirrhosis will develop esophageal varices at some point, and 30% of these patients will have at least one bleeding episode because of rupture of a varix. Most first bleeding episodes happen during the first year after the detection of the varices, with a 5%-10% mortality attributed to the initial hemorrhage. For this reason, identifying the presence of esophageal varices is a fundamental part of the diagnostic work-up in patients with cirrhosis, and it is also a prognostic marker of the illness.
Recent studies have emphasized the use of noninvasive methods to identify patients with the intention of avoiding endoscopy in low-risk cases. The fact that distinct predictors of the presence of varices have been identified in different studies probably reflects differences between the study populations and spectrum of the disease and this makes it difficult to develop a widely applicable predictive model.
The cutoff point for platelet count/spleen diameter ratio (PC/SD) ratio was lower than that reported in previous literature (< 884.3 and < 909, respectively), with a sensitivity of 84% and specificity of 70%. The differences are probably influenced by racial characteristics. The PC/SD ratio should be considered to identifying patients with esophageal varices.
This is an interesting study in which whether ratio of platelet count to spleen diameter can be a predictive factor for existence of esophageal varices was examined in Mexican patients with hepatic cirrhosis. This paper validated the useful of platelet count/spleen diameter ratio and determined a cutoff value for the Mexican, which is a little smaller than the value found in the Caucasian population; suggest that this ratio may be racial specific.
P- Reviewers: Elena V, Jeng JH, Wei L S- Editor: Gou SX L- Editor: A E- Editor: Zhang DN
| 1. | Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D, Brouwer JT. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1013] [Cited by in RCA: 957] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 2. | Gentilini P, Laffi G, La Villa G, Romanelli RG, Buzzelli G, Casini-Raggi V, Melani L, Mazzanti R, Riccardi D, Pinzani M. Long course and prognostic factors of virus-induced cirrhosis of the liver. Am J Gastroenterol. 1997;92:66-72. [PubMed] |
| 3. | Rukhsana JF, Javed IF, Masood R, Hameed A, Farooq A, Sultan G. Outcome after injection sclerotherapy for esophageal variceal bleeding in patients with liver cirrhosis and COPD. J Postgrad Med Inst. 2005;19:76-80. |
| 4. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007;102:2086-2102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 257] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 5. | Pascal JP, Calès P, Desmorat H. Natural history of esophageal varices. Recent advances in the pathophysiology and treatment of portal hypertension. Serono Symposia review no. 22. 1989;127-142. |
| 6. | de Franchis R. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762-768. [PubMed] |
| 7. | Schepis F, Cammà C, Niceforo D, Magnano A, Pallio S, Cinquegrani M, D’amico G, Pasta L, Craxì A, Saitta A. Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection? Hepatology. 2001;33:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 176] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Madhotra R, Mulcahy HE, Willner I, Reuben A. Prediction of esophageal varices in patients with cirrhosis. J Clin Gastroenterol. 2002;34:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 144] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Zein CO, Lindor KD, Angulo P. Prevalence and predictors of esophageal varices in patients with primary sclerosing cholangitis. Hepatology. 2004;39:204-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Zaman A, Becker T, Lapidus J, Benner K. Risk factors for the presence of varices in cirrhotic patients without a history of variceal hemorrhage. Arch Intern Med. 2001;161:2564-2570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 107] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Riggio O, Angeloni S, Nicolini G, Merli M, Merkel C. Endoscopic screening for esophageal varices in cirrhotic patients. Hepatology. 2002;35:501-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Giannini E, Botta F, Borro P, Risso D, Romagnoli P, Fasoli A, Mele MR, Testa E, Mansi C, Savarino V. Platelet count/spleen diameter ratio: proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 2003;52:1200-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 299] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 13. | Giannini EG, Botta F, Borro P, Dulbecco P, Testa E, Mansi C, Savarino V, Testa R. Application of the platelet count/spleen diameter ratio to rule out the presence of oesophageal varices in patients with cirrhosis: a validation study based on follow-up. Dig Liver Dis. 2005;37:779-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Zimbwa TA, Blanshard C, Subramaniam A. Platelet count/spleen diameter ratio as a predictor of oesophageal varices in alcoholic cirrhosis. Gut. 2004;53:1055. [PubMed] |
| 15. | Díaz-Piedra P, Olay-Fuentes G, Hernández-Gómez R, Cervantes-Villagrana RD, Presno-Bernal JM, Alcántara-Gómez LE. Determinación de los intervalos de referencia de biometría hemática en población mexicana. Rev Latinoamer Patol Clin. 2012;59:243-250. |
| 16. | Giannini EG, Zaman A, Kreil A, Floreani A, Dulbecco P, Testa E, Sohaey R, Verhey P, Peck-Radosavljevic M, Mansi C. Platelet count/spleen diameter ratio for the noninvasive diagnosis of esophageal varices: results of a multicenter, prospective, validation study. Am J Gastroenterol. 2006;101:2511-2519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 172] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 17. | de Mattos AZ, de Mattos AA. Platelet count/spleen diameter ratio: can it replace endoscopy for the screening of esophageal varices in cirrhotic patients? Eur J Gastroenterol Hepatol. 2012;24:1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Feldman M, Friedman LS, Sleinsenger MH. Enfermedades gastrointestinales y hepáticas. En: Fisiopatología, diagnóstico y tratamiento. Panamericana, editor. 7ª edición 2002; 1579-1587. |
| 19. | Bressler B, Pinto R, El-Ashry D, Heathcote EJ. Which patients with primary biliary cirrhosis or primary sclerosing cholangitis should undergo endoscopic screening for oesophageal varices detection? Gut. 2005;54:407-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Sanyal AJ, Fontana RJ, Di Bisceglie AM, Everhart JE, Doherty MC, Everson GT, Donovan JA, Malet PF, Mehta S, Sheikh MY. The prevalence and risk factors associated with esophageal varices in subjects with hepatitis C and advanced fibrosis. Gastrointest Endosc. 2006;64:855-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 21. | Chawla S, Katz A, Attar BM, Gupta A, Sandhu DS, Agarwal R. Platelet count/spleen diameter ratio to predict the presence of esophageal varices in patients with cirrhosis: a systematic review. Eur J Gastroenterol Hepatol. 2012;24:431-436. [PubMed] |
| 22. | Chalasani N, Imperiale TF, Ismail A, Sood G, Carey M, Wilcox CM, Madichetty H, Kwo PY, Boyer TD. Predictors of large esophageal varices in patients with cirrhosis. Am J Gastroenterol. 1999;94:3285-3291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 145] [Article Influence: 5.6] [Reference Citation Analysis (0)] |