Published online Dec 28, 2014. doi: 10.3748/wjg.v20.i48.18477
Revised: June 13, 2014
Accepted: July 15, 2014
Published online: December 28, 2014
Processing time: 236 Days and 4.5 Hours
Jejunoileal diverticula are rare and generally asymptomatic. In the few cases of patients who develop complications such as diverticulitis, perforation, obstruction, and/or hemorrhage, conventional treatment consists of surgical resection. We describe a case of perforated jejunoileal diverticulum with localized abscess and highlight the merits of surgical vs medical management. The patient is a 77-year-old male who presented with sharp, constant abdominal pain just inferior to the umbilicus. Administration of intravenous antibiotics results in complete and long-term resolution of the patient’s symptoms. In this report, we establish a framework for safely treating perforated small bowel diverticulum without surgical exploration.
Core tip: Perforated jejunal diverticulum can be safely managed without surgical exploration in carefully selected patients.
- Citation: Levack MM, Madariaga ML, Kaafarani HM. Non-operative successful management of a perforated small bowel diverticulum. World J Gastroenterol 2014; 20(48): 18477-18479
- URL: https://www.wjgnet.com/1007-9327/full/v20/i48/18477.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i48.18477
Jejunoileal diverticula are rare. They are incidentally found in less than 0.5%-2.3% of small bowel contrast studies and less than 0.3%-4.5% of autopsy studies[1]. First described in 1794, they are thought to occur due to mucosal and submucosal herniation through weakened areas of the muscularis mucosa of the bowel, usually on the mesenteric border. Most small bowel diverticula are asymptomatic and can be observed without need for intervention. Six to ten percent of patients develop complications including diverticulitis, perforation, obstruction and/or hemorrhage. Conventional treatment for a perforated jejunoileal diverticulum consists of surgical resection of the involved segment with small bowel anastomosis. We describe here the case of a patient who presented with a perforated jejunal diverticulum and a peri-diverticular abscess, who was successfully treated non-operatively.
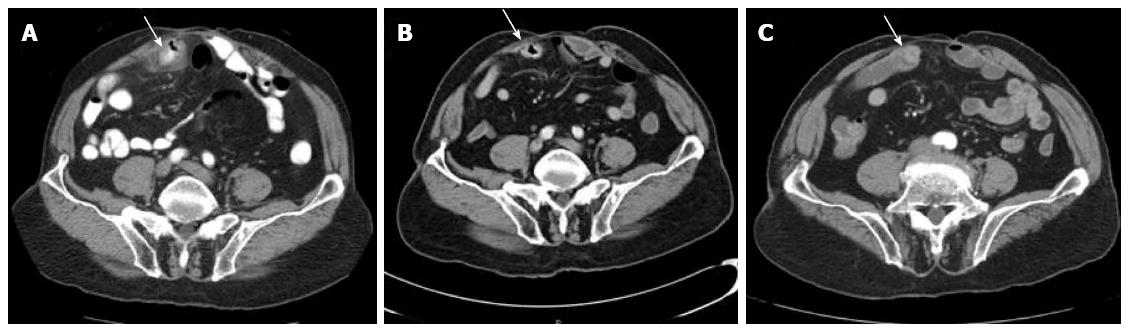
A 77-year-old male presented to the emergency room with a three day history of abdominal pain. The pain was sharp and constant in nature and localized just lateral and inferior to umbilicus. He endorsed that he continued to pass flatus and have normal bowel movements. His past medical history was pertinent for a remote surgical history of a gunshot wound to the abdomen requiring an exploratory laparotomy in 1968, the details of which were unknown by the patient. On review of systems, he denied diarrhea, vomiting, blood per rectum or signs of obstruction. On examination, his vital signs were stable, and he appeared alert, oriented and not in any acute distress. His abdomen had a well-healed midline laparotomy scar and was focally tender to palpation with guarding lateral to the scar in the right lower quadrant. There was no guarding or rebound tenderness. His laboratory studies showed a leukocytosis of 11.4 th/cmm with a neutrophilic predominance. Computed tomography (CT) demonstrated a focally thickened loop of small bowel in the anterior midabdomen with a small collection adjacent to the thickened small bowel measuring 2.8 cm × 1 cm. There was no evidence of obstruction and the thickened loop appeared most consistent with a perforated small bowel diverticulum (Figure 1A). He was started on broad spectrum antibiotic coverage utilizing IV Ampicillin, Ciprofloxacin and Flagyl and was hydrated with IV fluids and treated with bowel rest. The collection was deemed too small for percutanous drainage. His pain significantly improved over the next 3-4 d, and he was discharged on hospital day 5 on oral Ciprofloxacin and Flagyl for a 14 d total course of antibiotics. On follow up in clinic 1 wk later, his symptoms had completely resolved, and a repeat CT scan at that time revealed significantly decreased thickening of a focal loop of small bowel with near complete resolution of the adjacent inflammatory changes (Figure 1B). A CT enterography 6 wk later revealed a small bowel diverticulum with complete resolution of the inflammation (Figure 1C). At 1 year phone follow up, the patient remained asymptomatic and had no further episodes of pain.
Unlike colonic diverticula, the natural history of small bowel diverticula is not well studied, and most cases in the literature report on operative resection and re-anastomosis[2]. In a small series of 4 cases of complicated jejunal diverticulitis (two cases of gastrointestinal hemorrhage, one case of perforation and one case of enterolith obstruction), all patients underwent surgical resection with good postoperative outcomes[1]. In another retrospective review of 208 patients with small bowel diverticulosis, jejunal diverticula occurred in 18% of patients, but were associated with 46% of complications (e.g., bleeding, perforation, obstruction)[3].
Similar to our experience, 2 reported cases of perforated small bowel diverticulitis both initially managed medically with bowel rest and antibiotics have been described[4]. One patient later required surgical resection due to failure of medical therapy. Colvin et al[5] similarly described a case of localized peritonitis from a jejunal diverticulum which was successfully managed with bowel decompression and antibiotics. Novak et al[6] reported a series of 2 patients with small bowel perforations secondary to jejunal diverticula who were treated with a combination of antibiotics and percutaneous drainage.
We report here the successful non-operative management of a perforated jejunoileal diverticulum that presented with localized abdominal symptoms and signs. In our patient, intravenous antibiotics alone resulted in complete and long-term resolution of the patient’s symptoms, and are thus recommended as initial management for a perforated small bowel diverticulum with subsequent CT imaging follow-up.
In cases of diffuse peritonitis or pneumoperitoneum on imaging, the authors still recommend surgical exploration and resection.
77-year-old male with sharp, constant abdominal pain for 3 d. The patient had normal vital signs and his abdomen was tender to palpation in the lower quadrant.
Perforated small bowel diverticulitis with adjacent small abscess.
Common causes of abdominal pain in the right lower quadrant in a male patient are appendicitis, colonic diverticulitis, and hernia; most of these can be differentiated by appropriate imaging.
Complete blood count demonstrated mild leukocytosis (11.4 th/cmm) with neutrophilic predominance.
Computed tomography of the abdomen showed perforated small bowel diverticulum.
No pathological specimens were obtained in this case.
This patient was treated with IV antibiotics and temporary bowel rest.
Carefully selected patients with small bowel perforated diverticulitis can be successfully treated with IV antibiotics, bowel rest, and serial abdominal exams.
This is a case report of rare gastrointestinal diseases; perforated jejunal diverticulitis in a patient whose medical treated was successfully resolved without surgery. The authors admitted that an initial treatment with antibiotic is necessary, but surgical resection is acquired if peritonitis became a risk. Although the knowledge is not novel, a careful evaluation of the case is meaningful because it can be highly risk and the patient response is case per case dependent.
P- Reviewer: Du YQ, Leardkamolkarn V, Li SD, Uludag M S- Editor: Qi Y L- Editor: A E- Editor: Ma S
| 1. | Patel VA, Jefferis H, Spiegelberg B, Iqbal Q, Prabhudesai A, Harris S. Jejunal diverticulosis is not always a silent spectator: a report of 4 cases and review of the literature. World J Gastroenterol. 2008;14:5916-5919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Longo WE, Vernava AM. Clinical implications of jejunoileal diverticular disease. Dis Colon Rectum. 1992;35:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 93] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 3. | Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997;184:383-388. [PubMed] |
| 4. | Prost A La Denise J, Douard R, Berger A, Cugnenc PH. Small bowel diverticulosis complicated by perforated jejunal diverticula: conservative and/or surgical management? Hepatogastroenterology. 2008;55:1657-1659. [PubMed] |
| 5. | Colvin HS, Kuenfoo C, Rajab TK, Sayadatas T. Non-surgical management of recurrent perforation of a jejunal diverticulum following previous segmental bowel resection: a case report. J Med Case Rep. 2009;3:7318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Novak JS, Tobias J, Barkin JS. Nonsurgical management of acute jejunal diverticulitis: a review. Am J Gastroenterol. 1997;92:1929-1931. [PubMed] |