Published online Dec 28, 2014. doi: 10.3748/wjg.v20.i48.18439
Revised: June 19, 2014
Accepted: August 13, 2014
Published online: December 28, 2014
Processing time: 251 Days and 1.1 Hours
AIM: To study the relationship between resilience and quality of life (QOL) in patients with digestive cancer.
METHODS: The resilience of patients was measured prior to treatment, and their psychological distress, fatigue status, and treatment side effects were assessed 3 wk after. Their QOL was measured after their treatment ended. A relationship model of these variables was constructed using path analysis.
RESULTS: Resilience explained 33.2% of the variance in psychological distress, 16.1% of the variance in fatigue, and 1.23% of the variance in side effects. The relationship between resilience and QOL was statistically significant (β = 0.119, t = 4.499, P < 0.001) when psychological distress, fatigue, and side effects were absent from the regression model, whereas the adjusted regression coefficient of resilience was not statistically significant (t = 1.562, P > 0.05) when these variables were added. Psychological distress, together with fatigue and side effects, could explain 52.40% of the variance in QOL (P < 0.05). Physiological distress accounted for 28.94% of the total effect on QOL, fatigue accounted for 33.72%, side effects accounted for 22.53%, and resilience accounted for 14.80%.
CONCLUSION: Resilience is not an independent predictor of QOL in patients with digestive cancer, but it is a main factor influencing psychological distress and side effects.
Core tip: Resilience is an individual’s capacity to maintain their psychological and physical well-being in the face of adversity. Cancer is a disease causing severe psychological distress in patients. Exploring the association between resilience and quality of life (QOL) can help us understand the role of resilience in improving the QOL of cancer patients, as well as providing clinical staff with information on psychological intervention and psychological care programs for cancer patients. Our findings highlight the need to develop strategies that improve resilience in patients with digestive cancer.
- Citation: Tian J, Hong JS. Assessment of the relationship between resilience and quality of life in patients with digestive cancer. World J Gastroenterol 2014; 20(48): 18439-18444
- URL: https://www.wjgnet.com/1007-9327/full/v20/i48/18439.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i48.18439
Cancer is a disease that severely damages human physical and mental health. Its diagnosis significantly affects a patient’s emotional and psychological status[1], with the patient’s quality of life (QOL) often being affected considerably after surgery and chemotherapy/radiotherapy[2-4]. However, many studies have found that cancer patients with similar diseases and treatment status have significantly different QOLs[5,6]. Psychologists believe that resilience is the main factor that causes patients with similar situations to have different perceptions of their QOL[7,8].
Resilience is an individual’s capacity to maintain their psychological and physical well-being in the face of adversity[8]. In recent years, the role of resilience in the process of cancer treatment has been given increasing attention[9-14]. Studies have found that resilience can powerfully predict patients’ fatigue from treatment[12], good resilience can help patients reduce treatment-induced damage to bodily functions and shorten the time of bodily function recovery[13], and patients with good resilience are able to treat their disease correctly and maintain a relatively good psychological state, thereby resulting in a better QOL[11,12].
Although much research has shown that a relationship exists between QOL and resilience in cancer patients[11,14-16], limited information is available on the nature of this relationship and the degree of the influence of resilience on QOL. Exploring whether resilience is an independent predictor of QOL and estimating the degree of its impact on QOL can help us understand the role of resilience in improving the QOL of cancer patients, as well as provide clinical staff with information on psychological intervention and psychological care programs for cancer patients.
In this study, we used path analysis to detect the relationships of resilience, psychological distress, fatigue, and treatment side effects with QOL. We drew a path map to show the paths of the influences of resilience, psychological distress, fatigue, and side effects on QOL, and quantitatively estimated their direct and indirect effects on it. Our results may help explain whether strategies to improve resilience are important in promoting the QOL of cancer patients.
We selected patients with digestive tumors from Fujian Province for this study, as digestive cancer ranks as the leading cause of death in that area. The patients were recruited from five province-level hospitals in Fuzhou City during 2008-2011. The study sample was limited to patients whose tumors were located in the esophagus, stomach, or colorectum. The following eligibility criteria were used: (1) aged between 18 and 70 years; (2) literate; (3) lacking mental or psychological disease; and (4) with a known diagnosis of cancer.
All participants provided their written informed consent. The study was approved by the relevant institutional review boards for human research from Fujian Medical University.
The RS-14, a 14-item questionnaire proposed by Wagnild[17] with the score for each item ranging from 1 (not true) to 7 (true), was used to measure the resilience of the participants. Patients scored the items based on their personal circumstances. The total score of the scale ranges from 14 to 98, with a high total score indicating good resilience. The RS-14 has been used for measuring an individual’s degree of resilience in a wide variety of age groups[18], and its reliability and validity have been confirmed by many researchers[19]. In the present study, the Chinese version of this tool was found to have a reliability of 0.93.
The Hospital Anxiety and Depression Scale, a 14-item (7 for the anxiety subscale, 7 for the depression subscale) questionnaire, was used to evaluate the psychological distress of the participants[20]. The score for each item ranges from 0 to 3. Patients scored the items based on their current situation. The total score of the scale ranges from 0 to 42, with a high total score indicating severe psychological distress. The Chinese version of this scale has been confirmed to be suitable for Chinese patients[21]. In the current study, this version had a reliability of 0.92.
The 20-item Multidimensional Fatigue Inventory Scale, developed by a Dutch research group[22], was used for measuring the fatigue of the participants. The score for each item ranges from 1 (true) to 5 (not true). Patients scored the items based on their current situation. A high total score indicates severe fatigue. The Chinese version has been confirmed to be suitable for Chinese patients[23].
Treatment side effects in the participants were examined from seven aspects: gastrointestinal system, respiratory system, liver and kidney, heart, hair, skin, and nervous system. The severity of side effects in each of these aspects had five ordinal scales: none, mild, moderate, slightly severe, and severe, which were scored 1-5, respectively. The total score was the sum of the scores of the seven categories, with a high total score indicating severe side effects.
The European Organization for Research and Treatment of Cancer Core Questionnaire (Version 3.0) determined the QOL of cancer patients[24], and is a 30-item questionnaire that includes 28 items scored from 1 to 4 and 2 items scored from 1 to 7. The Chinese version of this questionnaire has been confirmed to be suitable for Chinese cancer patients[24]. In the current study, the sum of the scores for Items 1-5 and Items 8-19 describes the physical aspect of QOL (QOL-Physical), the sum of the scores for Items 20-25 describes the mental aspect of QOL (QOL-Mental), and the sum of the scores for Items 6, 7, 26, and 27 describes the social aspect of QOL (QOL-Social). All these scores were transformed into values in the range of 0-100. A high total score indicates good QOL.
Data on each patient were collected in three periods: before the first treatment cycle began (first period), the patient’s resilience was measured by trained graduate students from Fujian Medical University; in the third week of treatment (second period), the patient’s psychological distress, fatigue, and side effects were measured by trained nurses in the hospitals; and at the end of the first treatment cycle (third period), the patient’s QOL was measured by trained graduate students from Fujian Medical University.
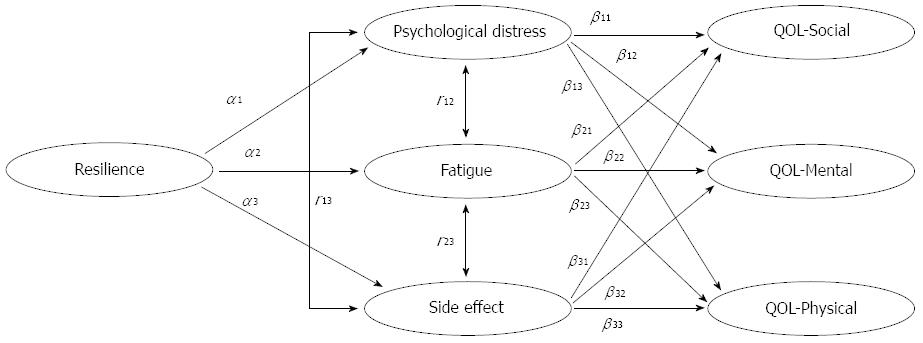
Low resilience affects mental health[25]. Poor mental health can increase side effects and fatigue[26] and, together with fatigue and side effects, influence the QOL of an individual[27,28]. Therefore, we assumed that the models shown below describe the relationships between resilience (x), psychological distress (y1), fatigue (y2), side effects (y3), QOL-Social (z1), QOL-Mental (z2), and QOL-Physical (z3):
y1 = a1 + α1x + e1
y2 = a2 + α2x + e2 (1)
y3 = a3 + α3x + e3
z1 = b1 + β11y1 + β21y2 + β31y3 + epsilon1
z2 = b2 + β12y1 + β22y2 + β32y3 + epsilon2 (2)
z3 = b3 + β13y1 + β23y2 + β33y3 + epsilon3
Models (1) and (2) are plotted as a path map (Figure 1). In the figure, r12, r23, and r13 represent correlation coefficients between psychological distress (y1), fatigue (y2), and side effects (y3).
The path coefficients shown in Figure 1 were estimated using path analysis. The degree of the effects of resilience on the three domains of QOL is equal to the sum of the products of the path coefficients in the path map as follows:
Effect (x→z1) = α1×β11 + α2×β21 + α3×β31
Effect (x→z2) = α1×β12 + α2×β22 + α3×β32 (3)
Effect (x→z3) = α1×β13 + α2×β23 + α3×β33
The coefficient βij in Model (2) expresses the direct effect of yi on zj (i, j = 1,2,3). The indirect effects of psychological distress (y1), fatigue (y2), and side effects (y3) on QOL-Social (z1), QOL-Mental (z2), and QOL-Physical (z3) can be calculated with the following formula:
Indirect effect (y1→zi) = r12×β2i + r13×β3i
Indirect effect (y2→zi) = r12×β1i + r23×β3i (4)
Indirect effect (y3→zi) = r23×β2i + r13×β1i
i = 1, 2, 3
Statistical analysis was performed using SAS (Version 9.0) for Windows (SAS Institute, Inc., Cary, NC).
In total, 970 participants, including 699 (72.06%) males and 271 (27.94%) females at an average age of 56.38 years (SD = 12.91), were included in this study. The percentage of participants with primary school, middle school, high school, and college education levels were 27.61%, 30.97%, 24.87%, and 16.54%, respectively. Among the 970 participants, 338 (34.84%) had esophageal cancer, 374 (38.56%) had gastric cancer, and 258 (26.60%) had colon cancer; in addition, 122 (12.56%), 343 (35.36%), 316 (32.58%), and 189 (19.48%) were in stages I-IV of their respective diseases. Moreover, 750 (77.32%) patients underwent surgery combined with chemotherapy, 85 (8.76%) underwent surgery combined with radiotherapy, and 135 (13.92%) underwent surgery combined with chemotherapy and radiotherapy. The average time of the first treatment cycle was 4 wk.
Two assumptions are depicted in the model shown in Figure 1. One assumption was that psychological distress, fatigue, and treatment side effects were the main factors influencing QOL. To verify the correctness of this assumption, we analyzed the relationships between QOL as the dependent variable and psychological distress, fatigue, and side effects as the independent variables using multiple linear regression. The results revealed an adjusted R2 value of 0.524 for the model, indicating that psychological distress, fatigue, and side effects collectively could explain 52.4% of the variance in QOL, thus confirming that our assumption was appropriate. The other assumption in the model was that resilience had no direct effect on QOL. To verify this, we set resilience as the independent variable and QOL as the dependent variable in the regression model. The results showed that the regression coefficient of resilience, adjusted for age, sex, disease stage, psychological distress, fatigue, and side effects, was not statistically significant (t = 1.562, P = 0.119), indicating that resilience had no direct effect on QOL. Based on the previously mentioned analysis, we concluded that the model shown in Figure 1 was appropriate.
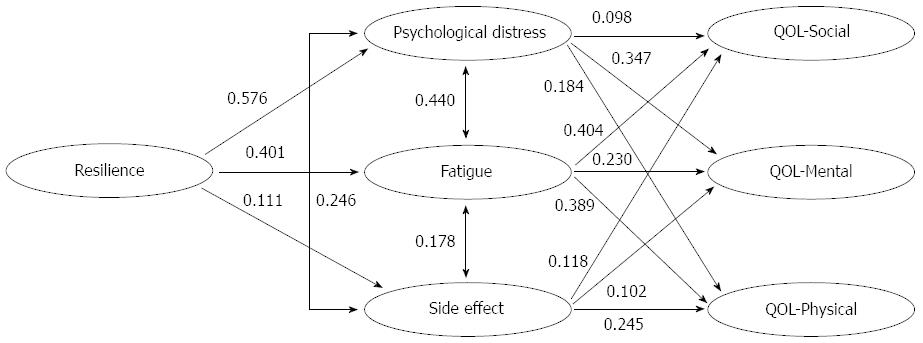
After adjusting for age, sex, and disease stage, the partial correlation coefficient between psychological distress and fatigue was r12 = 0.440 (P < 0.001), between psychological distress and side effects was r13 = 0.246 (P < 0.001), and between fatigue and side effects was r23 = 0.178 (P < 0.001).
The standardized coefficient for each path in the path map (Figure 1) was estimated, and the standardized coefficients adjusted for age, sex, and disease stage are shown in Table 1. The square of the standardized coefficient of resilience revealed that it could explain 33.2% of the variance in psychological distress and 16.1% of that in fatigue. These results suggest that resilience is an important factor that affects both psychological distress and fatigue.
| Dependent | Independent | Standardized coefficients | t | P value |
| Psychological distress | Resilience | -0.576 | -15.571 | < 0.001 |
| Fatigue | Resilience | -0.401 | -7.233 | < 0.001 |
| Side-effects | Resilience | -0.111 | -3.151 | 0.002 |
| QOL-Social | Psychological distress | -0.098 | -2.784 | 0.005 |
| Fatigue | -0.404 | -11.712 | < 0.001 | |
| Side-effects | -0.118 | -3.697 | < 0.001 | |
| QOL-Mental | Psychological distress | -0.347 | -10.149 | < 0.001 |
| Fatigue | -0.230 | -6.851 | < 0.001 | |
| Side-effects | -0.102 | -3.298 | 0.001 | |
| QOL-physical | Psychological distress | -0.184 | -5.748 | < 0.001 |
| Fatigue | -0.389 | -12.306 | < 0.001 | |
| Side-effects | -0.245 | -8.415 | < 0.001 |
The standardized coefficients in Table 1 were written into the path map (Figure 2). The direct and indirect effects of resilience, psychological distress, fatigue, and side effects on QOL were calculated according to Equations (3) and (4) (Table 2). Psychological distress and fatigue had greater effects on the three dimensions of QOL. The direct effects of fatigue were the largest for QOL-Social and QOL-Physical, the direct effect of psychological distress was the largest for QOL-Mental, and side effects mainly influenced by QOL-Physical.
| Factor | QOL-Social | QOL-Mental | QOL-Physical | ||||||
| Direct effect | Indirect effect | Total | Direct effect | Indirect effect | Total | Direct effect | Indirect effect | Total | |
| Psychological distress | 0.098 | 0.207 | 0.305 | 0.347 | 0.126 | 0.473 | 0.184 | 0.231 | 0.415 |
| Fatigue | 0.404 | 0.064 | 0.468 | 0.230 | 0.171 | 0.401 | 0.389 | 0.125 | 0.514 |
| Side-effects | 0.118 | 0.115 | 0.233 | 0.102 | 0.194 | 0.296 | 0.245 | 0.150 | 0.395 |
| Resilience | 0.000 | 0.160 | 0.160 | 0.000 | 0.235 | 0.235 | 0.000 | 0.212 | 0.212 |
By summing the direct effects on the three domains of QOL, we obtained the direct effects of psychological distress, fatigue, and side effects on QOL (data in the second column of Table 3). By summing the indirect effects on the three domains of QOL, we obtained the indirect effects of psychological distress, fatigue, side effects, and resilience on QOL (data in the third column of Table 3). The proportions of direct and indirect effects on QOL for psychological distress, fatigue, side effects, and resilience are shown in the fifth and sixth columns of Table 3. Fatigue, psychological distress, and side effects accounted for 48.32%, 29.71%, and 21.97%, respectively, of the total direct effect on QOL (fifth column of Table 3). Of the total effect on QOL, fatigue accounted for 33.72%, psychological distress accounted for 28.94%, side effects accounted for 22.53%, and resilience accounted for 14.80% (seventh column of Table 3). These results suggest that psychological distress and fatigue produced in the course of treatment are important factors influencing the QOL of patients. Although resilience has a lower proportion of the total effect on QOL, it has significant effects on fatigue and psychological distress.
| Factor | QOL | ||
| Direct effect | Indirect effect | Total | |
| Psychological distress | 0.629 (29.71) | 0.558 (28.13) | 1.187 (28.94) |
| Fatigue | 1.023 (48.32) | 0.360 (18.15) | 1.383 (33.72) |
| Side-effects | 0.465 (21.97) | 0.459 (23.14) | 0.924 (22.53) |
| Resilience | 0.000 (0.00) | 0.607 (30.59) | 0.607 (14.80) |
| Total | 2.117 (100.00) | 1.984 (100.00) | 4.101 (100.00) |
Resilience refers to an individual’s capacity to maintain their psychological and physical well-being in the face of adversity. Resilience can be viewed as a defense mechanism that enables one to thrive amid distress. Therefore, improving resilience may be an important target for disease treatment and prophylaxis[25]. Patients with cancer can show high levels of functioning in physical domains of QOL, but not in others, suggesting that an individual’s capacity to adjust and cope will influence their QOL. Individual differences in resilience cause patients to have different coping styles and adjustment capacities[5]. Therefore, it is necessary to introduce the concept of resilience into studies of the QOL of cancer patients.
QOL is an indicator of a patient’s social, psychological, and physiological status, as well as their well-being[1]. In theory, resilience affects the psychological aspect of QOL[10,12], and thus should have a direct effect on QOL. However, in this study, the regression coefficient of resilience (adjusted for age, sex, and disease stage) was statistically significant (β = 0.119, t = 4.499, P < 0.001) when psychological distress, fatigue, and treatment side effects were absent from the regression model; the reverse was true (t = 1.562, P > 0.05) when these variables were added. These results suggest that the effect of resilience on QOL may be passed on by psychological distress, fatigue, and side effects, and is therefore indirect. Further studies are necessary to confirm this conclusion.
In this study, we analyzed the patients in the following order: resilience → psychological distress, fatigue, and side effects → QOL; that is, resilience was plotted on the left part of the path map, which means that if patients with low resilience can be identified early and are given good social support as well as psychological care, then their psychological distress will likely decrease. This would prompt them to actively respond to treatment-induced fatigue and side effects, thereby improving their QOL.
In summary, the data obtained by our epidemiological survey showed that although resilience is not an independent predictor of QOL in patients with digestive cancer and accounted for only 14.80% of the total effect on QOL, it is a major influencing factor on psychological distress and side effects. In addition, psychological distress and fatigue are important factors that affect QOL, indicating that the role of resilience in improving QOL cannot be ignored. In studying the QOL of patients with cancer, we should focus on strategies that improve their resilience.
Resilience is an individual’s capacity to maintain their psychological and physical well-being in the face of adversity. Cancer is a disease causing severe psychological distress in patients. Exploring the association between resilience and quality of life (QOL) can help us understand the role of resilience in improving the QOL of cancer patients, as well as provide clinical staff with information on psychological intervention and psychological care programs for cancer patients.
In recent years, the role of resilience in the process of cancer treatment has been given increasing attention. Studies have found that resilience can powerfully predict patients’ fatigue during treatment, and good resilience can help patients reduce treatment-induced damage to bodily functions and shorten the time of bodily function recovery. The researchers suggested that patients with good resilience are able to treat their disease correctly and maintain a relatively good psychological state, thereby resulting in a better QOL.
Although much research has shown that a relationship exists between QOL and resilience in cancer patients, limited information is available on the nature of this relationship and the degree of the influence of resilience on QOL. This study showed the relationships between resilience, psychological distress, fatigue, and treatment side effects with QOL.
These results indicate that the role of resilience in improving QOL cannot be ignored. In studying the QOL of patients with cancer, the authors should focus on strategies that improve their resilience.
The paper examines a very important subject, namely the relationships between resilience and quality of life in digestive cancer patients. The subject is interesting and would be of equal interest for other cancers as well. Resilience, psychological distress, fatigue, and side effects were assessed for a large group of patients, and significant correlations were found and discussed in the paper. The findings are illustrated by figures and tables, and discussed in detail in the paper.
P- Reviewer: Kanda T, Tanase CP S- Editor: Ma YJ L- Editor: Rutherford A E- Editor: Wang CH
| 1. | Bottomley A. The cancer patient and quality of life. Oncologist. 2002;7:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 218] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 2. | Efficace F, Bottomley A, van Andel G. Health related quality of life in prostate carcinoma patients: a systematic review of randomized controlled trials. Cancer. 2003;97:377-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Andersen BL. Quality of life for women with gynecologic cancer. Curr Opin Obstet Gynecol. 1995;7:69-76. [PubMed] |
| 4. | Arora NK, Gustafson DH, Hawkins RP, McTavish F, Cella DF, Pingree S, Mendenhall JH, Mahvi DM. Impact of surgery and chemotherapy on the quality of life of younger women with breast carcinoma: a prospective study. Cancer. 2001;92:1288-1298. [PubMed] |
| 5. | Lawford J, Eiser C. Exploring links between the concepts of Quality of Life and resilience. Pediatr Rehabil. 2001;4:209-216. [PubMed] |
| 6. | Epping-Jordan JE, Compas BE, Osowiecki DM, Oppedisano G, Gerhardt C, Primo K, Krag DN. Psychological adjustment in breast cancer: processes of emotional distress. Health Psychol. 1999;18:315-326. [PubMed] |
| 7. | Yi JP, Vitaliano PP, Smith RE, Yi JC, Weinger K. The role of resilience on psychological adjustment and physical health in patients with diabetes. Br J Health Psychol. 2008;13:311-325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 138] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 8. | Richardson GE. The metatheory of resilience and resiliency. J Clin Psychol. 2002;58:307-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Pearman T. Quality of life and psychosocial adjustment in gynecologic cancer survivors. Health Qual Life Outcomes. 2003;1:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Bull AA, Meyerowitz BE, Hart S, Mosconi P, Apolone G, Liberati A. Quality of life in women with recurrent breast cancer. Breast Cancer Res Treat. 1999;54:47-57. [PubMed] |
| 11. | Wenzel LB, Donnelly JP, Fowler JM, Habbal R, Taylor TH, Aziz N, Cella D. Resilience, reflection, and residual stress in ovarian cancer survivorship: a gynecologic oncology group study. Psychooncology. 2002;11:142-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 182] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Strauss B, Brix C, Fischer S, Leppert K, Füller J, Roehrig B, Schleussner C, Wendt TG. The influence of resilience on fatigue in cancer patients undergoing radiation therapy (RT). J Cancer Res Clin Oncol. 2007;133:511-518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Hou WK, Law CC, Yin J, Fu YT. Resource loss, resource gain, and psychological resilience and dysfunction following cancer diagnosis: a growth mixture modeling approach. Health Psychol. 2010;29:484-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 14. | Costanzo ES, Ryff CD, Singer BH. Psychosocial adjustment among cancer survivors: findings from a national survey of health and well-being. Health Psychol. 2009;28:147-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 191] [Cited by in RCA: 165] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 15. | Yang HC, Thornton LM, Shapiro CL, Andersen BL. Surviving recurrence: psychological and quality-of-life recovery. Cancer. 2008;112:1178-1187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Antoni MH, Goodkin K. Host moderator variables in the promotion of cervical neoplasia--I. Personality facets. J Psychosom Res. 1988;32:327-338. [PubMed] |
| 17. | Wagnild GM. The Resilience Scale user’s guide for the US English version of the Resilience Scale and the 14-Item Reselience Scale (RS-14). Montana: The Resilience Center 2009; . |
| 18. | Ahern NR, Kiehl EM, Sole ML, Byers J. A review of instruments measuring resilience. Issues Compr Pediatr Nurs. 2006;29:103-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 283] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 19. | Nishi D, Uehara R, Kondo M, Matsuoka Y. Reliability and validity of the Japanese version of the Resilience Scale and its short version. BMC Res Notes. 2010;3:310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 20. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [PubMed] |
| 21. | Leung CM, Ho S, Kan CS, Hung CH, Chen CN. Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. A cross-cultural perspective. Int J Psychosom. 1993;40:29-34. [PubMed] |
| 22. | Smets EM, Garssen B, Bonke B, De Haes JC. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2188] [Cited by in RCA: 2436] [Article Influence: 81.2] [Reference Citation Analysis (0)] |
| 23. | Tian J, Hong JS. Validation of the Chinese version of Multidimensional Fatigue Inventory-20 in Chinese patients with cancer. Support Care Cancer. 2012;20:2379-2383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Zhen LC, Tian HR, Xie PZ. Medical Quality of survival Evaluation. Beijing: Junshi Yixue Kexue Press 2000; . |
| 25. | Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. 2010;30:479-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 587] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 26. | Tian J, Chen ZC, Hang LF. Effects of nutritional and psychological status in gastrointestinal cancer patients on tolerance of treatment. World J Gastroenterol. 2007;13:4136-4140. [PubMed] |
| 27. | Tian J, Chen ZC, Hang LF. The effects of psychological status of the patients with digestive system cancers on prognosis of the disease. Cancer Nurs. 2009;32:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Tian J, Chen ZC, Hang LF. Effects of nutritional and psychological status of the patients with advanced stomach cancer on physical performance status. Support Care Cancer. 2009;17:1263-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |