Published online Dec 21, 2014. doi: 10.3748/wjg.v20.i47.17970
Revised: September 25, 2014
Accepted: October 21, 2014
Published online: December 21, 2014
Processing time: 118 Days and 9.1 Hours
AIM: To evaluate whether postoperative radiotherapy is an alternative to neck lymph node surgery and if it provides a survival benefit for those receiving two-field, chest and abdomen, lymphadenectomy.
METHODS: A total of 530 cases with middle and lower thoracic esophageal carcinoma in our hospital from January 2008 to April 2009 were selected and analyzed, of which 219 cases received right chest, upper abdominal incision Ivor-Lewis surgery and simultaneously underwent mediastinal and abdominal two-field lymphadenectomy. If regional lymph node metastasis occurred within the recurrent laryngeal nerve, the patients would receive bilateral supraclavicular radiotherapy (DT = 5000cGy) to be adopted at postoperative 4-5 wk (Group A) or cervical lymphadenectomy at postoperative 3-4 wk (Group B). If there were no regional lymph node metastases within the recurrent laryngeal nerve, the patients only underwent two-field, chest and abdomen, lymphadenectomy (Group C).
RESULTS: In 219 cases who underwent two-field lymphadenectomy, 91 cases were diagnosed with regional lymph node metastasis within the recurrent laryngeal nerve. Of them, 48 cases received cervical radiotherapy, and 43 cases underwent staging lymphadenectomy; 128 patients were not given the follow-up treatment of cervical radiotherapy because there was no regional lymph node metastasis within the recurrent laryngeal nerve. Five-year survival rates in group A and B were 47% and 50%, respectively, with no statistical difference between them, and the rate in group C was 58%.
CONCLUSION: For patients with middle and lower thoracic esophageal carcinoma combined with lymph node metastasis within the recurrent laryngeal nerve, cervical radiotherapy can be a substitute for surgery and provide benefit.
Core tip: Three-field lymphadenectomy is currently a focus in esophageal surgery. According to the patterns of lymph node metastasis, understanding of the lymph node status in the middle and lower recurrent laryngeal nerve region may predict the status of cervical lymph nodes. In patients who have received thoracic and abdominal lymphadenectomy, if lymph node metastasis of recurrent laryngeal nerve is indicated it will be especially important to subsequently treat cervical lymph nodes. Additional cervical lymphadenectomy is always performed clinically in this case. In this article, we discuss whether cervical surgical procedures can be replaced by radiotherapy.
- Citation: Ren Y, Su C, Zhou Y, Zhao X, Yang CL, Liu YY. Effect of bilateral supraclavicular postoperative radiotherapy in middle and lower thoracic esophageal carcinoma. World J Gastroenterol 2014; 20(47): 17970-17975
- URL: https://www.wjgnet.com/1007-9327/full/v20/i47/17970.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i47.17970
Tumor cell metastasis via the lymphatic pathway is a major spread pathway of esophageal carcinoma. Many studies have demonstrated that esophageal carcinoma occurs more frequently at lymph nodes of the bilateral recurrent laryngeal nerve[1-3]. Especially for middle and lower thoracic esophageal carcinoma, once lymph node metastasis occurs in this region, it often indicates the presence of lymph node metastasis[4-7]. For those patients, three-field lymphadenectomy (including neck, chest, and abdominal lymph nodes) is often adopted. Three-field lymphadenectomy expands the scope of the operation, with benefits for the survival of patients[8-10]. However, it combines with an ensuing increase in surgical trauma and postoperative complications[11-17]. Cervical lymph node metastasis is not common[1], and not all patients will benefit from the three-field lymphadenectomy. On the other hand, surgery has its own limitations, and it can only reach the level of radical resection from the naked eye. Many studies have reported that patients who underwent three-field lymphadenectomy still have risks of recurrent cervical lymph node after surgery. Radiation therapy, as with surgery, can kill localized tumor cells, and has the advantage of being non-invasive compared with surgery. The question is whether or not we can adopt bilateral supraclavicular radiotherapy to replace lymphadenectomy, and achieve control effects on cervical lymph nodes. Based on this idea, we designed the supplemental treatment modality of cervical radiotherapy after two-field lymphadenectomy.
After preoperative examination, patients who had a definitive diagnosis of esophageal squamous cell carcinoma, with the location of the tumor in the middle and lower thoracic cavity, expected to achieve R0 resection at surgery, with no evidence of distant metastasis were included. Exclusion criteria: (1) the presence of preoperative palpation or ultrasound or positron emission tomography computed tomography (PET-CT) indicated that there were obvious cervical lymph nodes, highly suspicious transfers, or after pathological examination, cervical lymph node metastasis was confirmed (such patients need surgery before radiotherapy and chemotherapy); (2) preoperative diagnosis by CT or endoscopic ultrasound (EUS) of T4 (such patients tend to have lower rates of surgical resection, surgery is required before radiotherapy and chemotherapy); (3) patients with severe disease (severe cirrhosis, diabetes or heart and lung complications); and (4) patients with a history of previous gastric resection surgery (usually not as a substitute for the esophageal tube after surgery).
Patients with lower thoracic and cardia cancer, or confirmed adenocarcinoma through preoperative histological examination, were also excluded (such as specific pathological types, and if there was a possibility that accumulation at lower esophageal gastric region was present).
A total of 530 cases with middle and lower thoracic esophageal carcinoma in our hospital from January 2008 to April 2009 were selected and analyzed, of which 219 cases receiving right chest, upper abdominal incision Ivor-Lewis surgery, and simultaneously undergoing mediastinal and abdominal two-field lymphadenectomy, met the above criteria. Of 219 cases, 91 cases were diagnosed with regional lymph node metastasis within the recurrent laryngeal nerve. Among these, 48 cases received cervical radiotherapy at postoperative 4-5 wk (Group A), 43 cases underwent second cervical lymphadenectomy at postoperative 3 wk (Group B); 128 cases of postoperative recurrent laryngeal nerve pathology without lymph node metastasis received only two-field lymphadenectomy.
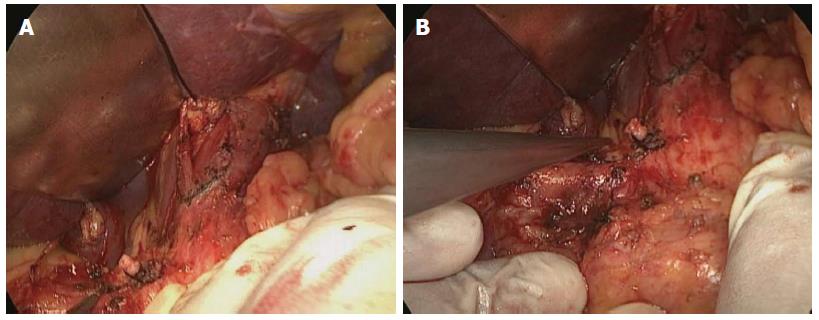
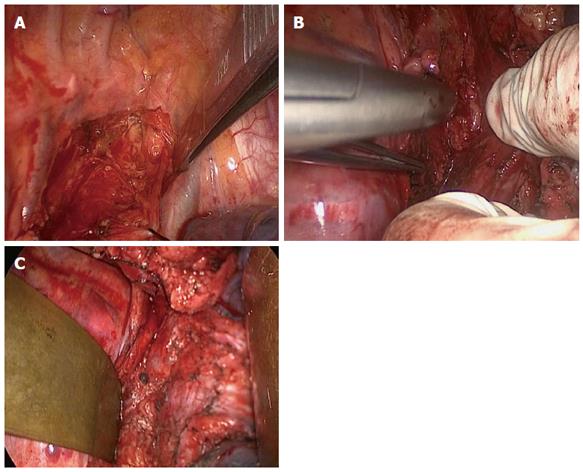
Abdominal surgical procedures: After abdominal incision, patients received abdominal surgery. Tissue was removed at a distance of ≥ 5 cm from the lower edge of the tumor, cardia and proximal stomach, where a gastric tube would be made. Simultaneously, abdominal lymph node resections were undergone (including the 16th set of pericardial lymph nodes, 17th set at drainage area of the left gastric artery, 18th set at the drainage area of common hepatic artery, 19th set at traveling area of splenic artery, 20th set of lymph nodes around the celiac artery) as shown in Figure 1.
Thoracic surgical procedures: Thoracic surgery was undergone through a posterolateral incision at the right side, dissociated almost from the entire thoracic esophagus; meanwhile, mediastinal lymph node regions were removed on the recurrent laryngeal nerve (2, 3, and 4 sets), as shown in Figure 2A and 2B, especially the cervicothoracic junction within the thoracic lymph entrance, and the middle and lower mediastinal lymph nodes (7, 8, 9, 10, and 16 sets), as shown in Figure 2C.
At the edge of the tumor lesions at ≥ 5 cm, the esophagus was cut, and a gastric tube was put into the thoracic cavity as a substitute. Through the esophageal bed, the stomach and top right pleural esophagus was anastomosed.
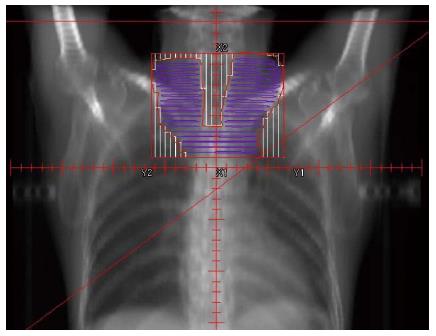
At postoperative 3-4 wk, the patients began to receive three-dimensional conformal radiotherapy at cervical and bilateral supraclavicular regions. Radiation fields included the bilateral supraclavicular region (upper boundary was the cricothyroid membrane level, lower boundary was the clavicular head level) as shown in Figure 3: 8 MV X-ray accelerator irradiation DT = 50GY/25 times, 2GY per time, 5 times/wk.
The data were analyzed using Mann Whitney’s U-test and Fisher’s exact test. Kaplan-Meir survival curves were used to analyze the subsistence data. The differences between groups were compared using log-rank test. P < 0.05 was considered to be statistically significant.
The characteristics of the three groups are shown in Table 1. The UICC TNM classification (the 7th edition) was used for staging. Significant differences in patient age, gender and tumor location were not observed.
| Parameters | Group A | Group B | Group C | P |
| (n = 48) | (n = 43) | (n = 128) | ||
| Age (yr) | 62.1 + 7.6 | 62.8 + 7.3 | 63.1 + 5.6 | |
| Sex | ||||
| Male | 47 | 43 | 125 | NS |
| Female | 1 | 0 | 3 | |
| Tumor location, n | ||||
| Middle thoracic | 30 | 27 | 73 | NS |
| Lower thoracic | 18 | 16 | 55 | |
| PT, n | ||||
| T1a | 4 | 3 | 9 | NS |
| T1b | 8 | 5 | 17 | |
| T2 | 18 | 17 | 48 | |
| T3 | 16 | 17 | 46 | |
| T4a | 2 | 1 | 8 | |
| PN, n | ||||
| N0 | 0 | 0 | 128 | |
| N1 | 23 | 19 | 0 | NS |
| N2 | 16 | 16 | 0 | |
| N3 | 9 | 8 | 0 | |
| PG, n | ||||
| G1 | 31 | 28 | 61 | NS |
| G2 | 15 | 13 | 59 | |
| G3 | 2 | 2 | 8 |
Postoperative complications occurred in 4 cases (4/48, 8.3%) in group A, and in 8 cases (8/43, 18.6%) in group B; 1 patient in group B died due to postoperative respiratory failure during hospitalization (Table 2).
| Complications | Group A | Group B | P |
| Anastomotic leak | 1 | 1 | NS |
| Recurrent laryngeal nerve palsy | 1 | 2 | NS |
| Respiratory failure | 0 | 1 | NS |
| Chylothorax | 1 | 2 | NS |
| Wound infection | 1 | 2 | NS |
| Hospital death | 0 | 1 | NS |
During the follow-up period, 60 cases had tumor recurrence or metastasis, among which were 18 cases of group A, 19 cases of group B and 23 cases of group C (Table 3). Two cases of group C had cervical lymph node metastasis. Lymph node metastasis was the most common in groups A and B; hematogenous metastasis was more common in group C (Table 3).
| Parameters | Group A | Group B | Group C |
| Cervical lymph nodes | 1 | 1 | 2 |
| Upper mediastinum (regional lymph nodes) | 2 | 1 | 2 |
| Middle and lower mediastinal lymph nodes | 6 | 7 | 2 |
| Abdominal lymph nodes | 6 | 5 | 3 |
| Hematogenous metastasis | 3 | 5 | 14 |
| Total | 18 | 19 | 23 |
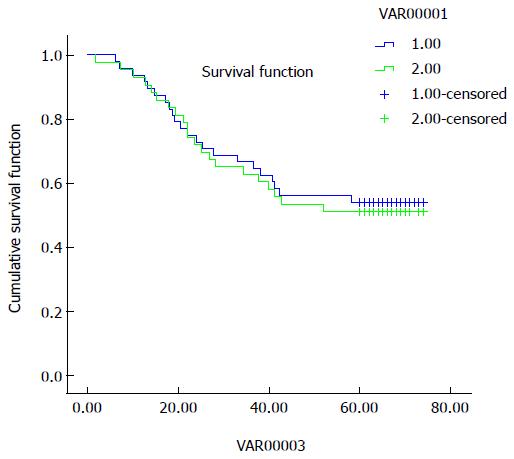
Cause-specific survival curves for groups A and B are shown in Figure 4. The 5-year survival rates of groups A and B were not significantly different, at 47% and 50%, respectively.
Surgery is the main treatment of esophageal carcinoma. As complete a removal of lymph node metastasis as possible is needed to ensure surgical efficacy. According to the characteristics of lymphatic drainage of esophageal carcinoma[18], bilateral cervical, chest and abdominal mediastinal may be the transferred areas; in theory, the removal of all nodes at the above-mentioned three regions (called three-field lymphadenectomy) can achieve maximum efficacy. Among the many clinical reports, the survival period of patients receiving three-field lymphadenectomy are generally higher than that of patients receiving mediastinal and abdominal lymphadenectomy[8-10]. However, three-field extended lymphadenectomy increases trauma and perioperative complications in patients[12-16]. Our study also found that patients who received three-field lymphadenectomy appeared to have a higher incidence of recurrent laryngeal nerve palsy and anastomotic leak compared with those who received two-field lymphadenectomy. Thus, it is controversial whether all patients should consistently receive three-field lymphadenectomy.
Some studies suggest that analyzing from the anatomy, regional lymph nodes of recurrent laryngeal nerve are a part of cervical lymph nodes. Thus, in the order of lymphatic drainage[19], lymph at the submucous layer of the esophagus is firstly drained to the recurrent laryngeal nerve, then to the neck[20,21]; regional lymph nodes of the recurrent laryngeal nerve are considered as the neck sentinel lymph nodes. In clinical practice, both Noguchi et al[22] and Noguchi[22] did pathological examinations of recurrent laryngeal nerve lymph nodes for patients who underwent IVOR-Lewis, and chose positive patients with recurrent laryngeal nerve lymph node metastasis to receive stepwise or contemporaneous neck lymph node dissection, while those without lymph node metastasis in this area received only two-field lymphadenectomy. There was no significant difference in clinical survival rate over the same period for lymphadenectomy patients. Li et al[23] found that, especially for patients with middle and lower thoracic esophageal carcinoma, the recurrent laryngeal nerve region might suggest lymph node status; therefore it is recommended to select the appropriate patients with cervical lymphadenectomy. Many studies support the idea that not all patients with esophageal carcinoma have lymph node metastasis present, and patients without lymph node metastasis cannot benefit from a three-field lymphadenectomy[1]. From this perspective, we did not give two-field lymphadenectomy for 128 patients without regional lymph node metastasis, and postoperative 5-year survival rate was 58%; therapeutic effect was achieved on an equal with similar literature. We believe that from the primary tumor resection perspective, Ivor-Lewis surgery can guarantee the thoroughness of middle and lower thoracic esophageal carcinoma resection. If three-field lymphadenectomy is not selected, it will make some patients have too much normal esophagus cut, stomach esophageal anastomosis will be forced at the neck, which only increases the pressure on surgery; it may bring more complications and affected the postoperative quality of life in patients.
In our study, only 91 cases with postoperative recurrent laryngeal nerve lymph nodes from 219 patients received two-field lymphadenectomy; these were considered to need follow-up treatment on cervical lymph nodes. The similarities of radiotherapy and surgery are that both of them can kill local tumor cells, but radiotherapy has the comparative advantage over surgery in that it is relatively non-invasive, and can reduce the patients’ psychological and physical adverse effects. Thus, for patients receiving two-field lymphadenectomy, can radiation therapy be used to replace the operation when there is the possibility of cervical lymph node metastasis? Based on this idea, we had 91 cases of two-field lymphadenectomy, of whom 48 patients were treated with postoperative cervical radiotherapy and 43 cases were given cervical lymphadenectomy. The results showed there was no significant difference in cervical lymph node recurrence rate between the two groups, while the 5-year survival rate was not significantly different in comparison. In other words, with this model, it can still achieve the efficacy of lymph node dissection without additional surgery. Postoperative cervical radiotherapy can reduce the pressure on doctors, reduce surgical trauma to patients, avoid neck incision, and be more easily accepted mentally.
In conclusion, for middle and lower thoracic esophageal carcinoma patients, postoperative radiotherapy after bilateral supraclavicular lymph node surgery can avoid cervical lymph node surgery, and the clinical efficacy is the same as with three-field lymphadenectomy.
A surgical procedure is the main method for treatment of esophageal cancer, and usually includes three aspects: tumor resection, lymph node resection and digestive tract reconstruction. Regarding lymph node resection, the scope and eradication are key factors influencing the surgical efficiency and also the focus of clinical research. Due to the special anatomic and lymphatic draining characteristics, neck, chest and abdomen are possible locations of metastasis. Theoretically, resections of all the possible lymph nodes may maximize the eradication, which however causes increased trauma during surgery. Currently, resections of thoracic and abdominal lymph nodes are the consensus of scholars dedicated to esophageal surgery. Thus, how to choose the appropriate patients for cervical lymphadenectomy and whether some surgical procedures can be replaced by non-surgical methods are investigated in this study.
Physicians have obtained favorable clinical outcomes in diagnosis of cervical lymph node metastasis by palpation and cervical ultrasound. Latest studies have found that according to the patterns of lymph node metastasis, lymph nodes in the recurrent laryngeal nerve region may serve as the outpost of cervical lymph nodes. Based on this, selective three-field lymphadenectomy may be performed to obtain better therapeutic efficacy.
In this study, the authors did not use techniques such as ultrasound, computed tomography, etc. to predict the lymph node status, but predicted cervical lymph node status according to the patterns of lymph node metastasis and pathological status of lymph nodes in the recurrent laryngeal nerve region. Based on this, selective subsequent treatment was performed, which avoided false positive results and micro-metastasis of technical methods. The obvious difference from previous studies is that they replaced traditional surgery with radiotherapy, which reduced the injuries of patients while relieving the mental pressure of both physicians and patients.
This study proved that it is feasible to selectively perform cervical lymphadenectomy according to the patterns of lymph node metastasis and the pathological status in the thoracic recurrent laryngeal nerve region. Therefore, surgical procedures might be replaced by regional radiotherapy. Furthermore, the regional recurrence rate and the 5-year survival rate were not significantly different from surgical procedures. Additionally, radiotherapy produces lighter injuries than surgery. Therefore, it is more easily accepted by patients and widely used clinically.
Three-field lymphadenectomy: this is a surgical procedure with additional cervical lymph node resection based on two-field lymphadenectomy (thoracic and abdominal field). The scope of cervical lymphadenectomy involves bilateral supraclavicular lymph nodes, cervical para-esophageal lymph nodes and anterior cervical lymph nodes.
The manuscript is very well written. For the patients with middle and lower thoracic esophageal carcinoma, once the regional lymph node metastasis occurs within the recurrent laryngeal nerve, it often indicates the presence of lymph node metastasis, which requires three-field lymphadenectomy. A total of 530 cases with middle and lower thoracic esophageal carcinoma are included. The results suggest that for patients with middle and lower thoracic esophageal carcinoma complicated with lymph node metastasis within the recurrent laryngeal nerve, cervical radiotherapy can substitute surgery and provide benefits.
P- Reviewer: Heba AA S- Editor: Yu J L- Editor: A E- Editor: Liu XM
| 1. | Nishihira T, Hirayama K, Mori S. A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg. 1998;175:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 187] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Fujita H, Kakegawa T, Yamana H, Shima I, Tanaka H, Ikeda S, Nogami S, Toh Y. Lymph node metastasis and recurrence in patients with a carcinoma of the thoracic esophagus who underwent three-field dissection. World J Surg. 1994;18:266-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Mizutani M, Murakami G, Nawata S, Hitrai I, Kimura W. Anatomy of right recurrent nerve node: why does early metastasis of esophageal cancer occur in it? Surg Radiol Anat. 2006;28:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Shiozaki H, Yano M, Tsujinaka T, Inoue M, Tamura S, Doki Y, Yasuda T, Fujiwara Y, Monden M. Lymph node metastasis along the recurrent nerve chain is an indication for cervical lymph node dissection in thoracic esophageal cancer. Dis Esophagus. 2001;14:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 82] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Araujo J, Bories E, Caillol F, Pesenti C, Guiramand J, Poizat FF, Monges G, Ries P, Raoul JL, Delpero JR. Distant lymph node metastases in gastroesophageal junction adenocarcinoma: impact of endoscopic ultrasound-guided fine-needle aspiration. Endosc Ultrasound. 2013;2:148-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Tabira Y, Yasunaga M, Tanaka M, Nakano K, Sakaguchi T, Nagamoto N, Ogi S, Kitamura N. Recurrent nerve nodal involvement is associated with cervical nodal metastasis in thoracic esophageal carcinoma. J Am Coll Surg. 2000;191:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Ueda Y, Shiozaki A, Itoi H, Okamoto K, Fujiwara H, Ichikawa D, Kikuchi S, Fuji N, Itoh T, Ochiai T. Intraoperative pathological investigation of recurrent nerve nodal metastasis can guide the decision whether to perform cervical lymph node dissection in thoracic esophageal cancer. Oncol Rep. 2006;16:1061-1066. [PubMed] |
| 8. | Tachibana M, Kinugasa S, Yoshimura H, Shibakita M, Tonomoto Y, Dhar DK, Nagasue N. Clinical outcomes of extended esophagectomy with three-field lymph node dissection for esophageal squamous cell carcinoma. Am J Surg. 2005;189:98-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 131] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Natsugoe S, Matsumoto M, Okumura H, Uchikado Y, Setoyama T, Sasaki K, Sakurai T, Omoto I, Owaki T, Shinchi H. Clinical course and outcome after esophagectomy with three-field lymphadenectomy in esophageal cancer. Langenbecks Arch Surg. 2010;395:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Fang WT, Chen WH. Current trends in extended lymph node dissection for esophageal carcinoma. Asian Cardiovasc Thorac Ann. 2009;17:208-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Butt MO, Luck NH, Hassan SM, Abbas Z, Mubarak M. Acute esophageal necrosis in a patient with end-stage renal disease on hemodialysis. J Translat Intern Med. 2014;2:143-145. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Shim YM, Kim HK, Kim K. Comparison of survival and recurrence pattern between two-field and three-field lymph node dissections for upper thoracic esophageal squamous cell carcinoma. J Thorac Oncol. 2010;5:707-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Isono K, Ochiai T, Okuyama K, Onoda S. The treatment of lymph node metastasis from esophageal cancer by extensive lymphadenectomy. Jpn J Surg. 1990;20:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Jamieson GG, Lamb PJ, Thompson SK. The role of lymphadenectomy in esophageal cancer. Ann Surg. 2009;250:206-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Isono K, Sato H, Nakayama K. Results of a nationwide study on the three-field lymph node dissection of esophageal cancer. Oncology. 1991;48:411-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 349] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 16. | Nishimaki T, Suzuki T, Suzuki S, Kuwabara S, Hatakeyama K. Outcomes of extended radical esophagectomy for thoracic esophageal cancer. J Am Coll Surg. 1998;186:306-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 111] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Rigatelli G, dell’Avvocata F, Magro B, Panin S. Atrial septal defects in the adult: Management, transcatheter and surgical therapeutic options and outcomes. J Translat Intern Med. 2014;2:111-118. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Assef M, Rossini L, Rossini L, Araki O, Nakao F, Silva J, Duenas W, Gagliardi D, Fabricio V. Relevance of endoscopic ultrasound in the management of esophagus cancer therapy. Endosc Ultrasound. 2014;3:S15-S16. |
| 19. | Sato T, Iizuka T. Color atlas of surgical anatomy for esophageal cancer. Tokyo: Springer-Verlag 1992; 25-90. |
| 20. | Akiyama H, Tsurumaru M, Udagawa H, Kajiyama Y. Systemic lymph node dissection for esophageal cancer-effective or not? Dis Esophagus. 1994;7:2-12. |
| 21. | Watanabe H. The problems of cervico-thoraco abdominal (3-field) lymphadenectomy for thoracic esophageal carcinoma. Ann Thorac Cardiovasc Surg. 1995;1:349-353. |
| 22. | Noguchi T, Wada S, Takeno S, Hashimoto T, Moriyama H, Uchida Y. Two-step three-field lymph node dissection is beneficial for thoracic esophageal carcinoma. Dis Esophagus. 2004;17:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Li H, Yang S, Zhang Y, Xiang J, Chen H. Thoracic recurrent laryngeal lymph node metastases predict cervical node metastases and benefit from three-field dissection in selected patients with thoracic esophageal squamous cell carcinoma. J Surg Oncol. 2012;105:548-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |