Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.17260
Revised: July 31, 2014
Accepted: September 12, 2014
Published online: December 7, 2014
Processing time: 177 Days and 16.4 Hours
Some laterally advanced cholangiocarcinomas behave as ductal spread or local invasion, and hepatopancreatoduodenectomy (HPD) may be performed for R0 resection. To date, there have been no reports of laparoscopic HPD (LHPD) in the English literature. We report the first case of LHPD for the resection of a Bismuth IIIa cholangiocarcinoma invading the duodenum. The patient underwent laparoscopic pancreaticoduodenectomy and right hemihepatectomy. Child’s approach was used for the reconstruction. The patient recovered well with bile leakage from the 2nd postoperative day and was discharged on the 16th postoperative day with a drainage tube in place which was removed 2 wk after discharge. Postoperative pathology revealed a well-differentiated cholangiocarcinoma and the margin of liver parenchyma, pancreas and stomach was negative for metastases. The results suggest that LHPD is a feasible and safe procedure when performed in highly specialized centers and in suitable patients with cholangiocarcinoma.
Core tip: This is the first report of laparoscopic hepatopancreatoduodenectomy (LHPD) for cholangiocarcinoma in the English literature. The patient was treated with laparoscopic pancreaticoduodenectomy and right hemihepatectomy. The successful outcome suggests that LHPD is a feasible and safe procedure when performed in highly specialized centers and in suitable patients with cholangiocarcinoma.
-
Citation: Zhang MZ, Xu XW, Mou YP, Yan JF, Zhu YP, Zhang RC, Zhou YC, Chen K, Jin WW, Matro E, Ajoodhea H. Resection of a cholangiocarcinoma
via laparoscopic hepatopancreato- duodenectomy: A case report. World J Gastroenterol 2014; 20(45): 17260-17264 - URL: https://www.wjgnet.com/1007-9327/full/v20/i45/17260.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.17260
Laparoscopic right hemihepatectomy and pancreaticoduodenectomy are among the most challenging abdominal surgical procedures[1,2]. To date, there are no reports of laparoscopic hepatopancreatoduodenectomy (LHPD) in the English literature. We hereby report the first case of LHPD in a patient with cholangiocarcinoma.
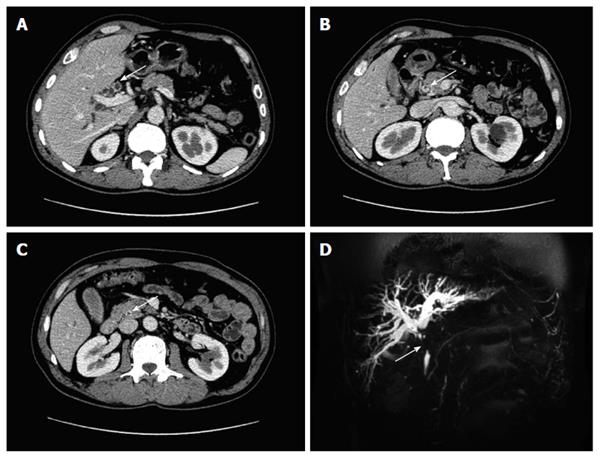
A 61-year-old man presented with the chief complaint of painless jaundice for 20 d. He denied any history of liver diseases or diabetes. No superficial lymph nodes were palpable on physical examination, but palpebral and bulbar conjunctivae demonstrated mild jaundice. The remaining physical examination was unremarkable. Routine laboratory tests were as follows: Liver function tests showed aspartate aminotransferase 103 U/L, alanine aminotransferase 248 U/L, alkaline phosphatase 422 U/L, gamma glutamyl transpeptidase 1165 U/L, total bilirubin 103.4 μmol/L, and direct bilirubin 67.4 μmol/L. Levels of tumor markers (carcinoembryonic antigen, alpha fetoprotein, and carbohydrate antigen 19-9) were within normal ranges. Enhanced computed tomography and magnetic resonance cholangiopancreatography scan revealed hepatic and upper common bile duct stenosis with intrahepatic bile duct dilatation (Figure 1). Extensive irregular thickening of the common bile duct wall was also noted. According to the medical history and the imaging findings, a preoperative diagnosis of cholangiocarcinoma was promptly established and laparoscopy was performed.
The patient was placed in the supine position with his head slightly elevated. The surgeon stood on the right side of the patient and the first assistant stood on the left. The second assistant holding the laparoscope stood on the right side, occasionally shifting to the left during the hepatectomy procedure. One initial 10-mm trocar was inserted below the umbilicus for laparoscopy. A 30-degree telescope was subsequently inserted for peritoneal cavity examination and to rule out metastatic disease. Four additional trocars (one 12 mm, three 5 mm) were inserted into the left upper flank, left flank, right upper flank, and right flank quadrants, respectively; these five trocars were arranged in a V pattern[3].
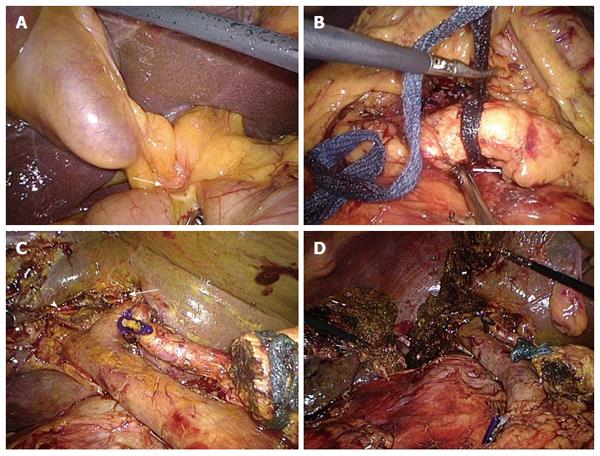
After a general examination, the tumor was found to be located in the middle section of the common bile duct invading the duodenum (Figure 2A). The gallbladder was dissected from the liver bed and the cystic duct and cystic artery were isolated and clipped. The anterior wall of the common bile duct above the cystic duct insertion was dissected and the tissue appeared to be clear of tumor invasion. A decision was made to perform a total laparoscopic pancreaticoduodenectomy.
After carefully exposing and preserving the common hepatic artery, the gastroduodenal artery was dissected and divided. The inferior border of the pancreatic neck was dissected and a retropancreatic tunnel was created above the superior mesenteric vein/portal vein and an umbilical tape was placed (Figure 2B).
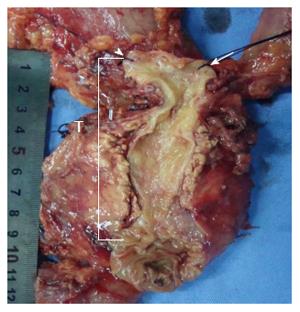
The jejunum was divided approximately 15 cm distal from the ligament of Treitz with an endoscopic linear stapler and the mesentery was mobilized. The distal duodenum and proximal jejunum were pushed to the right side of the operative field, under the mesenteric vessels. The distal stomach was transected with endoscopic linear staplers for standard resection. The pancreas neck was then divided using a harmonic scalpel. The duodenum and uncinate process were carefully dissected along the lateral border of the superior mesenteric artery. The hepatic artery, the common bile duct and the portal vein were dissected. The hepatic hilum was completely skeletonized as well as the hepatoduodenal ligament. The right hepatic bile duct and the left hepatic bile duct were separated and sharply transected (Figure 2C). The resected specimen after laparoscopic pancreaticoduodenectomy was removed using an endoscopic bag by enlarging the incision at the periumbilical port (Figure 3). The distal common bile duct was resected and the specimen was sent for frozen section which revealed a negative margin for the left hepatic bile duct and a positive margin for the right hepatic bile duct. Pneumoperitoneum was reestablished. The residual right hepatic bile duct was dissected again and a further 0.5 cm of tissue was resected. Frozen section results revealed a positive margin again. In order to achieve an R0 resection, laparoscopic right hemihepatectomy was performed after informed consent was obtained.
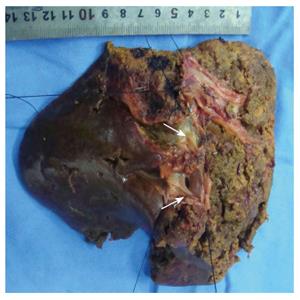
The right liver was fully mobilized. The left hepatic artery and left portal vein were carefully dissected and preserved. The right hepatic artery and right portal vein were ligated and divided. The short hepatic veins were clamped and severed. An ischemic line was noted on the liver surface; the hepatic parenchyma was transected along this demarcation line using a harmonic scalpel and an endoscopic stapling device. A right hemihepatectomy was then performed (Figure 2D). The liver specimen was retrieved through the periumbilical port. Child’s approach was used for the reconstruction. The first anastomosis was a duct-to-mucosa pancreaticojejunostomy, with a stent placed in the pancreatic duct. The seromuscular layer of the jejunum and the capsule of the pancreas were secured from the anterior and posterior layers. The second anastomosis was an end-to-side hepaticojejunostomy; which was stitched with running 3-0 absorbable sutures. The final anastomosis was a side-to-side gastroenterostomy located 40 cm downstream from the hepaticojejunostomy (by an endoscopic linear stapler) and the common enterotomy was closed with 3-0 Vicryl. One drainage tube was placed near the transection plane of the liver and the other two silicon drains were placed adjacent to the anastomoses of the hepaticojejunostomy and pancreaticojejunostomy.
The operation lasted 600 min and the estimated blood loss was 450 mL. The patient was sent to a normal ward after a one day stay in the intensive care unit. On the 2nd postoperative day, his drainage tube revealed bile leakage. The amount of bile leakage was 80-100 mL per day and decreased gradually to 20-30 mL per day two weeks later. The patient started to take semi-fluid food on the 6th day after surgery and no obvious intra-abdominal infections were noted. The two silicon drains were removed and he was discharged on the 16th postoperative day with the drainage tube in place. Postoperative pathology revealed a well-differentiated cholangiocarcinoma invading the duodenum. The tumor had spread to the distal common bile duct 1.5 cm from Vater’s ampulla (Figure 4). The margin of liver parenchyma, pancreas and stomach were negative and 14 lymph nodes were all negative (Figure 5). The last drainage tube was removed 2 wk after discharge. There was no complaints during the next 4 mo after surgery.
Surgical resection remains the only option for long-term survival in patients with cholangiocarcinoma. However, some laterally advanced cholangiocarcinomas behave as ductal spread or local invasion. The main goal of definitive surgery is R0 resection and in some cases hepatopancreatoduodenectomy (HPD) may be performed. Since researchers reported the first series of HPD cases (5 locally advanced gallbladder cancers) in 1980, HPD remains among the most challenging operations for hepatobiliary surgeons today[4,5]. Despite the poor survival rate and high morbidity and mortality in the first decade after diagnosis, HPD is persistently performed in several specialized centers[6]. With recent progress in diagnostic procedures, surgical techniques and perioperative patient care, many studies have shown increased long-term survival after this aggressive procedure. Ebata et al[7] reported 85 HPD procedures performed between 1992 and 2011 with a 5-year survival rate of 37%, mean blood loss of 2696 mL, and a rate of major postoperative complications of 77.6%. In patients with M0 disease, the 5-year survival rate was 54%. The indication for HPD in patients with cholangiocarcinoma is still controversial. Nagino[8] concluded that HPD should be carried out for the following indications: (1) diffusely infiltrating tumors of the entire extrahepatic bile duct; (2) downward superficial spread; or (3) bulky nodal metastases of the pancreatoduodenal region. The case presented here was a Bismuth IIIa tumor invading the duodenum. HPD was deemed the best choice of treatment and postoperative pathology revealed a successful R0 resection.
Recent progress in laparoscopic technology has broadened the clinical applications of laparoscopy. Many series of hepatic and pancreatic laparoscopic surgeries have been reported, and many of these cases were advanced malignancies with favorable surgical and oncological outcomes. However, laparoscopic right hemihepatectomy and pancreaticoduodenectomy are still the most difficult laparoscopic procedures due to the complexity of the operation (intricate dissection, multiple reconstructions) and possible intra-operative risks (uncontrollable massive bleeding and gas embolism). Advanced laparoscopic skills are in high demand and require a steep learning curve. To our knowledge this is the first report of LHPD for a cholangiocarcinoma in the English literature.
Advanced laparoscopic hepato-biliary-pancreatic surgery was adopted in 2003 at our institution, and 22 successful laparoscopic pancreaticoduodenectomy had been performed up until December 2013[1,3,9-11]. Cumulative attending experience in laparoscopic hepatectomy, hepaticojejunostomy, pancreaticojejuno- stomy and gastroenterostomy is fundamental to performing this extremely difficult procedure successfully.
Clinical experience gained from the present case included: (1) Laparoscopy assisted strategic guidance remains invaluable for tumor staging and evaluation of treatment options. Therefore, laparoscopic pancreaticoduodenectomy was performed prior to laparoscopic hemihepatectomy. Fortunately, during the operation, the frozen section of the left hepatic bile duct was negative; otherwise the patient would have undergone an R1 resection; (2) Compared with conventional HPD procedures, this case had less blood loss, fewer postoperative complications, quicker recovery similar to other typical minimally invasive surgery. The magnified visualization of the anatomy during the operation and pneumoperitoneum CO2 pressure are probable reasons for the reduced blood loss; (3) The 5 trocar approach was utilized for the entire LHPD. We apply the 5 trocar strategy to perform laparoscopic hepatopancreatobiliary surgery and gastrectomy routinely including only one 12 mm trocar, which is an economically feasible and relatively safe procedure; and (4) During this time-consuming procedure, maintaining the constancy of the internal environment of the patient is important. Despite the efforts of the anesthesiologists, we used a warming device to maintain the patient’s body temperature. In the late stage of the operation, end-tidal carbon dioxide partial pressure was as high as 48 mmHg. We reduced the CO2 pressure to 12 mmHg. During the operation, the surgeons took 5 breaks, each lasting approximately 20 min to allow both patient and surgeon to rest. After each break, circulatory and respiratory functions were found improved.
In conclusion, this is the first reported case of LHPD and the results suggest that LHPD is a feasible and safe procedure when performed in highly specialized centers and in suitable patients with cholangiocarcinoma.
The patient was a 61-year-old male who presented with the chief complaint of painless jaundice for 20 d.
A Bismuth IIIa cholangiocarcinoma invading the duodenum.
Primary sclerosing cholangitis; bile duct adenoma; benign biliary stricture.
Liver function tests revealed aspartate aminotransferase 103 U/L, alanine aminotransferase 248 U/L, alkaline phosphatase 422 U/L, gamma glutamyl transpeptidase 1165 U/L, total bilirubin 103.4 μmol/L, and direct bilirubin 67.4 μmol/L. Levels of tumor markers (carcinoembryonic antigen, alpha fetoprotein, and carbohydrate antigen 19-9) were within normal ranges.
Enhanced computed tomography and magnetic resonance cholangiopancreatography scan revealed hepatic and upper common bile duct stenosis with intrahepatic bile duct dilatation as well as extensive irregular thickening of the common bile duct wall.
Postoperative pathology revealed a well-differentiated cholangiocarcinoma invading the duodenum. The tumor had spread to the distal common bile duct 1.5 cm from Vater’s ampulla. The margin of liver parenchyma, pancreas and stomach were negative for metastases.
The patient was treated with laparoscopic hepatopancreatoduodenectomy (LHPD).
This is the first reported case of LHPD and the results suggest that LHPD is a feasible and safe procedure when performed in highly specialized centers and in suitable patients with cholangiocarcinoma.
This is the first successful reported LHPD for a cholangiocarcinoma. The surgical outcome is satisfactory compared with conventional hepatopancreatoduodenectomy. But a long-term follow-up is needed in order to evaluate oncological feasibility and safety.
P- Reviewer: Rerknimitr R, Vasilieva LE S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
| 1. | Cai X, Li Z, Zhang Y, Yu H, Liang X, Jin R, Luo F. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc. 2014;28:1334-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Kendrick ML. Laparoscopic and robotic resection for pancreatic cancer. Cancer J. 2012;18:571-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Zhang RC, Xu XW, Wu D, Zhou YC, Ajoodhea H, Chen K, Mou YP. Laparoscopic transduodenal local resection of periampullary neuroendocrine tumor: a case report. World J Gastroenterol. 2013;19:6693-6698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Ebata T, Yokoyama Y, Igami T, Sugawara G, Mizuno T, Nagino M. Review of hepatopancreatoduodenectomy for biliary cancer: an extended radical approach of Japanese origin. J Hepatobiliary Pancreat Sci. 2014;21:550-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Miwa S, Kobayashi A, Akahane Y, Nakata T, Mihara M, Kusama K, Ogawa S, Soeda J, Miyagawa S. Is major hepatectomy with pancreatoduodenectomy justified for advanced biliary malignancy? J Hepatobiliary Pancreat Surg. 2007;14:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Ota T, Araida T, Yamamoto M, Takasaki K. Operative outcome and problems of right hepatic lobectomy with pancreatoduodenectomy for advanced carcinoma of the biliary tract. J Hepatobiliary Pancreat Surg. 2007;14:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y, Nagino M. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 2012;256:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 160] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 8. | Nagino M. Perihilar cholangiocarcinoma: a surgeon’s viewpoint on current topics. J Gastroenterol. 2012;47:1165-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 9. | Chen K, Mou YP, Xu XW, Cai JQ, Wu D, Pan Y, Zhang RC. Short-term surgical and long-term survival outcomes after laparoscopic distal gastrectomy with D2 lymphadenectomy for gastric cancer. BMC Gastroenterol. 2014;14:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Yan JF, Mou YP, Xu XW, Ni JJ, Chen DW, Zhu YP, Chen QL, Zhou YC, Xie K. [Laparoscopic distal pancreatectomy: the experience of 68 cases in a single centre]. Zhonghua Waike Zazhi. 2012;50:802-805. [PubMed] |
| 11. | Zhang RC, Yan JF, Xu XW, Chen K, Ajoodhea H, Mou YP. Laparoscopic vs open distal pancreatectomy for solid pseudopapillary tumor of the pancreas. World J Gastroenterol. 2013;19:6272-6277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |