Published online Nov 28, 2014. doi: 10.3748/wjg.v20.i44.16544
Revised: April 29, 2014
Accepted: May 25, 2014
Published online: November 28, 2014
Processing time: 279 Days and 5.9 Hours
Gallstones represent the most frequent aetiology of acute pancreatitis in many statistics all over the world, estimated between 40%-60%. Accurate diagnosis of acute biliary pancreatitis (ABP) is of outmost importance because clearance of lithiasis [gallbladder and common bile duct (CBD)] rules out recurrences. Confirmation of biliary lithiasis is done by imaging. The sensitivity of the ultrasonography (US) in the detection of gallstones is over 95% in uncomplicated cases, but in ABP, sensitivity for gallstone detection is lower, being less than 80% due to the ileus and bowel distension. Sensitivity of transabdominal ultrasonography (TUS) for choledocolithiasis varies between 50%-80%, but the specificity is high, reaching 95%. Diameter of the bile duct may be orientative for diagnosis. Endoscopic ultrasonography (EUS) seems to be a more effective tool to diagnose ABP rather than endoscopic retrograde cholangiopancreatography (ERCP), which should be performed only for therapeutic purposes. As the sensitivity and specificity of computerized tomography are lower as compared to state-of-the-art magnetic resonance cholangiopancreatography (MRCP) or EUS, especially for small stones and small diameter of CBD, the later techniques are nowadays preferred for the evaluation of ABP patients. ERCP has the highest accuracy for the diagnosis of choledocholithiasis and is used as a reference standard in many studies, especially after sphincterotomy and balloon extraction of CBD stones. Laparoscopic ultrasonography is a useful tool for the intraoperative diagnosis of choledocholithiasis. Routine exploration of the CBD in cases of patients scheduled for cholecystectomy after an attack of ABP was not proven useful. A significant rate of the so-called idiopathic pancreatitis is actually caused by microlithiasis and/or biliary sludge. In conclusion, the general algorithm for CBD stone detection starts with anamnesis, serum biochemistry and then TUS, followed by EUS or MRCP. In the end, bile duct microscopic analysis may be performed by bile harvested during ERCP in case of recurrent attacks of ABP and these should be followed by laparoscopic cholecystectomy.
Core tip: Gallstones represent the most frequent aetiology of acute pancreatitis estimated between 40%-60%. Clearance of lithiasis (gallbladder and common bile duct, CBD rules out recurrences. Confirmation of biliary lithiasis is done by imaging. Endoscopic ultrasonography (EUS) seems to be a more effective tool to diagnose acute biliary pancreatitis rather than endoscopic retrograde cholangiopancreatography, which should be performed only for therapeutic purposes. As the sensitivity and specificity of computerized tomography are lower as compared to state-of-the-art magnetic resonance cholangiopancreatography or EUS, especially for small stones and small diameter of CBD, the later techniques are preferred nowadays.
- Citation: Surlin V, Săftoiu A, Dumitrescu D. Imaging tests for accurate diagnosis of acute biliary pancreatitis. World J Gastroenterol 2014; 20(44): 16544-16549
- URL: https://www.wjgnet.com/1007-9327/full/v20/i44/16544.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i44.16544
Gallstones represent the most frequent aetiology of acute pancreatitis in many statistics all over the world. The proportion from the total number of acute pancreatitis cases is estimated between 40%-60%, with variations due especially to diagnostic efforts and availability of imaging tests[1]. Accurate diagnosis of acute biliary pancreatitis (ABP) is of outmost importance because clearance of lithiasis (gallbladder and common bile duct, CBD) rules out recurrences, very frequent otherwise, with 30% to 50% of the patients developing recurrent acute pancreatitis relatively soon after discharge (average time 108 d), some of them maybe more severe than the previous episode[2].
Once the diagnosis of acute pancreatitis is made, grounded on generally acknowledged criteria of abdominal pain and three times more than normal hyperamilasemia/hyperlipidemia and/or intravenous (iv) contrast-enhanced helical computerized tomography (CT) scan/magnetic resonance imaging (MRI)/ transabdominal ultrasonography (TUS), the biliary aetiology is suspected if jaundice, elevated alanine aminotransferase (ALT) (three times more than normal) or a dilated CBD are present[3]. To those criteria we might add statistical data of a higher incidence in women, between 50 and 70 years of age[1].
Confirmation of biliary lithiasis is done by imaging. Clearance of biliary lithiasis implies a cholecystectomy and the removal of CBD stones. The minimal invasive approach is preferred nowadays, either by combined approach of laparoscopic cholecystectomy and endoscopic extraction of CBD stones, or total laparoscopic approach (cholecystectomy and CBD exploration and calculi extraction). Thus, once a diagnosis of gallbladder lithiasis is made, especially for microlithiasis, the most important thing is to establish whether there is also a CBD stone. Over 90% of the CBD stones come from the gallbladder through the cystic duct. Primary stones arising in the CBD are rarer and usually due to conditions that alter the normal flow of the bile and create conditions for bile stasis. “Silent stones” in the CBD may be present in up to 15% in patients younger than 60 years undergoing cholecystectomy, and even more frequent in older patients[4]. However, the incidence of ABP in choledocholithiasis is only 3%-8%[1]. Even more important, after triggering the acute pancreatitis, most of stones pass through the papilla into the duodenum[5]. Thus, the percentage of CBD stones in ABP decreases from 28.6% in the first 4 h to 8% at 1 wk[6,7].
The first, and the most available and commonly performed is TUS. It seeks for lithiasis in the gallbladder, CBD or indirect signs of biliary obstruction, e.g., dilation of the CBD. The sensitivity of the US in the detection of gallstones is over 95% in uncomplicated cases, but in ABP, sensitivity for gallstone detection is lower, being only 67%-78% due to the ileus and bowel distension[8]. Sensitivity of TUS for choledocholithiasis varies between 50%-80%, but the specificity is high, reaching 95%[9].
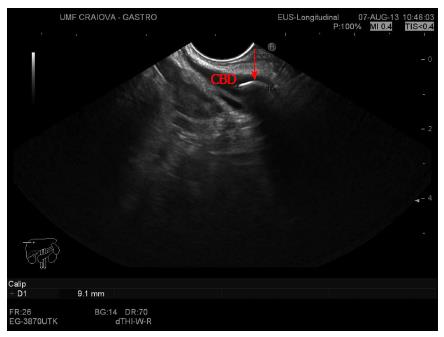
Diameter of the bile duct may be orientative for diagnosis. In a prospective study, the diameter of the CBD was measured before cholecystectomy and it was compared afterwards with finding stones at the surgical intervention. There were no stones in the CBD if the diameter was less or equal to 3 mm, while 7.7% of patients with the ducts measuring 4 mm or more had stones. If the size increased, the probability of having stones also increased, nearly all ducts of 9 mm or more had stones[10] (Figure 1).
Endoscopic US is more accurate than transcutaneous US, with a sensitivity of over 90% and an even higher specificity[11,12]. Nevertheless, the technique is more expensive and it requires a longer learning curve. EUS seems to be a more effective tool to diagnose ABP rather than ERCP, which should be performed only for therapeutic purposes. In a systematic review of clinical trials from 1994 to 2010, comparing EUS and ERCP in ABP, it was found that EUS avoided ERCP in 71.2% of cases, had no related complication, while ERCP was complicated in over 20% of cases. The clinical course of ABP was not influenced by either of those explorations[13]. A meta-analysis performed on 36 studies with 3532 patients revealed a sensitivity of 89% and a specificity of 94% for choledocholithiasis[14], with another meta-analysis performed on 2673 patients showing even higher numbers of 94% sensitivity and 95% specificity[15]. Consequently, EUS is an important diagnostic tool for the presence of CBD stones, as it accurately visualizes the CBD without the need of instrumentation[16]. There is now enough evidence to support the use of EUS before ERCP, even for smaller stones (less than 4 mm), as it can spare at least two thirds of ERCPs[17]. Moreover, as compared to MRCP, EUS has the same sensitivity, specificity and accuracy, although the sensitivity of MRCP seems to diminish in small (less than 6 mm) CBD stones. Thus, EUS has a significant impact for surgical decision making, especially in the patients with suspected ABP[18] (Figure 2).
Unenhanced helical CT scan has a variable accuracy for the detection of choledocholithiasis, with a sensitivity of 60%-87% and a specificity of 97%-100%[19,20]. CT-cholangiography has a higher performance for the diagnosis of choledocolithiasis with a sensitivity of 85%-96% and a specificity of 88%-98%[19,21]. As the sensitivity and specificity of CT are lower as compared to state-of-the-art MRCP or EUS, especially for small stones and small diameter of CBD, the later techniques are nowadays preferred for the evaluation of ABP patients.
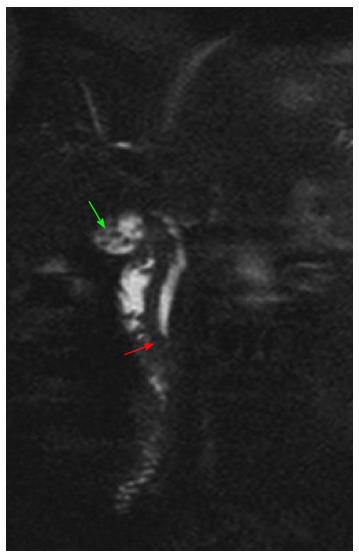
MRCP has a high reported accuracy in the diagnosis of choledocholithiasis. Meta-analyses report pooled sensitivities of 92%-94%[7,22] and a specificity of 99%. There are still controversies regarding the optimal imaging method in the preoperative assessment of patients with ABP, but MRCP has the advantage of a non-invasive method that could properly detect CBD lithiasis. The efficacy of MRCP in detecting CBD stones and to assess the time of choledochal passage of calculi was also compared to ERCP. Overall, MRCP had a positive predictive value 90.5%, negative predictive value 95.2%, sensitivity 82.6%, specificity 97.5% and overall accuracy 94.2%. Moreover, MRCP diagnoses anatomical variants of cystic duct and acute cholecystitis[6,7]. A prospective study compared the efficacy of EUS compared to MRCP and ERCP in the same patients with suspected extrahepatic biliary disease, taking into account also the economic aspect. Results regarding choledocholithiasis were that EUS was more sensitive than MRCP in the detection of choledocholithiasis (80% vs 40%), with similar specificity. Rate of acute pancreatitis after ERCP was 6.6%. EUS strategy had the greatest cost-utility by avoiding unnecessary ERCP examinations[23]. Nevertheless, a systematic review showed a similar diagnostic value for prospective studies that compared MRCP and EUS for the detection of CBD stones[24] (Figure 3).
ERCP has the highest accuracy for the diagnosis of choledocholithiasis and is used as a reference standard in many studies, especially after sphincterotomy and balloon extraction of CBD stones. Diagnostic ERCP does not, however, detect all stones and in one study its sensitivity was 89% in comparison with EUS, especially for small stones hidden by contrast injection[12]. EUS has been compared to ERCP in a prospective randomized fashion in cases of acute pancreatitis suspected to have a biliary cause. The patients had EUS or ERCP examinations within 24 h from admission. If EUS detected choledocholithiasis, therapeutic ERCP was performed immediately. EUS was successful in all patients, but ERCP failed in 10%, the difference being significant. Also ERCP failed to identify stones in 8.5%. Morbidity, hospital stays and mortality was similar in both groups[25]. The preferred approach for concomitant gallbladder and CBD stones in the laparoscopic era is sequential preoperative ERCP followed by laparoscopic cholecystectomy, although this has been found to have similar efficacy, maybe with a shorter hospital stay with laparoscopic CBD exploration during cholecystectomy[26]. The same conclusion was also reached by a Cochrane systemic review comparing the endoscopic versus surgical treatment of CBD stones, with laparoscopic CBD clearance being as effective as pre- or post-operative ERCP[27].
Laparoscopic ultrasonography (LUS) is a useful tool for the intraoperative diagnosis of choledocolithiasis. Thus, LUS was compared to laparoscopic cholangiography with the same specificity (100%) and positive predictive value (100%), and a sensitivity of 93%[28]. Nevertheless, laparoscopic exploration of the bile duct is as safe and effective as postoperative ERCP in clearing stones from the common duct[29]. The benefit of routine intraoperative cholangiography at the time of cholecystectomy in patients with ABP submitted to laparoscopic cholecystectomy was also questioned. Thus, patients with ABP submitted to cholecystectomy with or without intraoperative cholangiography and CBD exploration were compared in terms of outcome. At 3.8 years of follow up there was no significant difference regarding the rate of recurrent pancreatitis or biliary complications, suggesting that intraoperative cholangiography does not improve outcome after cholecystectomy for gallstone pancreatitis[30]. Another study showed that laparoscopic cholecystectomy (LC) can be performed safely without intraoperative cholangiography (IOC). Thus, from the patients with symptomatic gallstone disease, about 9.2% were selected for preoperative ERCP based upon preoperative clinical, laboratory and ultrasound criteria. In those patients, 58% were found with choledocholithiasis, and stone clearance was achieved in all cases. The other patients were submitted to laparoscopic cholecystectomy with no injury of CBD, no mortality and a rate of retained CBD stones of 1.5% at 2 years follow-up[31].
The necessity of routine exploration of the CBD in cases of patients scheduled for cholecystectomy after an attack of ABP was submitted to question. Ito et al[32] investigated this in cases of low risk for choledocholithiasis. The authors included 148 patients without preoperative ERCP, normal and decreasing liver function tests, and normal CBD diameter. They were divided into 2 groups - with or without intraoperative cholangiography. Follow-up didn’t find any significant differences between the 2 groups regarding postoperative episodes of acute pancreatitis, cholangitis or changes in liver function tests. Authors concluded that direct CBD exploration could be safely avoided in selected cases of ABP, with low-risk for choledocholithiasis.
Some of the acute pancreatitis cases remain idiopathic even after complete serum biochemistry, ultrasound and CT evaluations. Nevertheless, the aetiology of acute pancreatitis should be determined in at least 80% of cases and no more than 20% should be classified as idiopathic (recommendation grade B)[33]. These represent between 10% and 30% in different series. Some studies suggested that more accurate imaging tests for biliary lithiasis detection may reveal the biliary cause in those cases. In our experience, it also happened that once we introduced in our hospital EUS and ERCP there was a shift between the leading causes for acute pancreatitis between the alcoholic and biliary causes, many of idiopathic pancreatitis being actually biliary ones. Recently, some studies showed that a significant rate of the so-called idiopathic pancreatitis are actually caused by microlithiasis and/or biliary sludge, identified by the presence of cholesterol monohidrate and/or calcium bilirubinate microcrystals in the biliary sediment.
Microlithiasis is a viscous precipitate containing mucin, cholesterol and calcium bilirubinate which can obstruct the pancreatic duct. US has a sensitivity of only about 55% in detecting microlithiasis and does not allow for analysis of the chemical composition of bile[34]. This is an important cause of recurrent acute pancreatitis. Though a EUS procedure is diagnostic, with a high sensitivity and specificity[35] a duodenal aspirate or a bile duct aspirate for the microliths[36] at ERCP is confirmatory. In a series of 86 patients[37] with acute pancreatitis, 21 patients had microlithiasis. Six patients were subjected to cholecystectomy and 4 patients to endoscopic sphincterotomy. Fewer recurrences were noted in patients receiving either of the two treatment modalities compared to the group managed conservatively. The treatment protocol would warrant a cholecystectomy in all patients unless contraindicated. In those with a high operative risk, endoscopic biliary sphincterotomy is a safe and viable option[38]. Ursodeoxycholic acid is an alternative in those with bleeding tendencies[39]. Thus, microlithiasis or biliary sludge as a causative aetiology for acute pancreatitis remains controversial and not well understood. Several studies have demonstrated the presence of biliary sludge in as many as 75% of patients with unexplained acute pancreatitis[37]. Bile analysis with microscopic examination is considered the gold standard for diagnosis. Bile can be obtained directly while cannulating the bile duct during ERCP or following CCK stimulation on EGD. ERCP with bile aspiration from the CBD has a reported sensitivity of 83% in detecting microlithiasis[40].
In patients considered to have idiopathic acute pancreatitis, after negative routine work-up for biliary etiology, EUS is recommended as the first step to assess for occult microlithiasis, neoplasms and chronic pancreatitis. If EUS is negative, rare and uncommon causes should be looked for. MRCP (secretin-stimulated) is advised to identify or rule out rare morphologic abnormalities. If aetiology still remains unidentified, genetic counselling (not necessarily genetic testing) should be considered in order to search for hereditary or other genetic causes[3].
In conclusion, the general algorithm for CBD stone detection starts with anamnesis, serum biochemistry and then TUS, followed by EUS or MRCP. In the end, bile duct microscopic analysis may be performed by bile harvested during ERCP in case of recurrent attacks of ABP and these should be followed by laparoscopic cholecystectomy.
P- Reviewer: Nakazawa T, Sperti C, van Erpecum K S- Editor: Nan J L- Editor: A E- Editor: Ma S
| 1. | Larson SD, Nealon WH, Evers BM. Management of gallstone pancreatitis. Adv Surg. 2006;40:265-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Testoni PA, Mariani A, Curioni S, Zanello A, Masci E. MRCP-secretin test-guided management of idiopathic recurrent pancreatitis: long-term outcomes. Gastrointest Endosc. 2008;67:1028-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Sherman S, Alvarez C, Robert M, Ashley SW, Reber HA, Lehman GA. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 1993;13:e1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1080] [Cited by in RCA: 1039] [Article Influence: 86.6] [Reference Citation Analysis (6)] |
| 4. | National Institutes of Health Consensus Development Conference Statement on Gallstones and Laparoscopic Cholecystectomy. Am J Surg. 1993;165:390-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 143] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Ayub K, Imada R, Slavin J. Endoscopic retrograde cholangiopancreatography in gallstone-associated acute pancreatitis. Cochrane Database Syst Rev. 2004;CD003630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | De Waele E, Op de Beeck B, De Waele B, Delvaux G. Magnetic resonance cholangiopancreatography in the preoperative assessment of patients with biliary pancreatitis. Pancreatology. 2007;7:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | MSAC Report: Magnetic Resonance Cholangiopancreatography, Canberra, ACT, Australia, Department of Health and Ageing, Commonwealth of Australia. 2005. Available from: http://www.msac.gov.au. |
| 8. | Neoptolemos JP, Hall AW, Finlay DF, Berry JM, Carr-Locke DL, Fossard DP. The urgent diagnosis of gallstones in acute pancreatitis: a prospective study of three methods. Br J Surg. 1984;71:230-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 69] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Vilgrain V, Palazzo L. Choledocholithiasis: role of US and endoscopic ultrasound. Abdom Imaging. 2001;26:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Hunt DR, Reiter L, Scott AJ. Pre-operative ultrasound measurement of bile duct diameter: basis for selective cholangiography. Aust N Z J Surg. 1990;60:189-192. [PubMed] |
| 11. | de Lédinghen V, Lecesne R, Raymond JM, Gense V, Amouretti M, Drouillard J, Couzigou P, Silvain C. Diagnosis of choledocholithiasis: EUS or magnetic resonance cholangiography? A prospective controlled study. Gastrointest Endosc. 1999;49:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 135] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Prat F, Amouyal G, Amouyal P, Pelletier G, Fritsch J, Choury AD, Buffet C, Etienne JP. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis. Lancet. 1996;347:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 168] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | De Lisi S, Leandro G, Buscarini E. Endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography in acute biliary pancreatitis: a systematic review. Eur J Gastroenterol Hepatol. 2011;23:367-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Garrow D, Miller S, Sinha D, Conway J, Hoffman BJ, Hawes RH, Romagnuolo J. Endoscopic ultrasound: a meta-analysis of test performance in suspected biliary obstruction. Clin Gastroenterol Hepatol. 2007;5:616-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 113] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Tse F, Liu L, Barkun AN, Armstrong D, Moayyedi P. EUS: a meta-analysis of test performance in suspected choledocholithiasis. Gastrointest Endosc. 2008;67:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008;57:1004-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 353] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 17. | Fusaroli P, Kypraios D, Caletti G, Eloubeidi MA. Pancreatico-biliary endoscopic ultrasound: a systematic review of the levels of evidence, performance and outcomes. World J Gastroenterol. 2012;18:4243-4256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Papanikolaou IS, Adler A, Neumann U, Neuhaus P, Rösch T. Endoscopic ultrasound in pancreatic disease--its influence on surgical decision-making. An update 2008. Pancreatology. 2009;9:55-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Cabada Giadás T, Sarría Octavio de Toledo L, Martínez-Berganza Asensio MT, Cozcolluela Cabrejas R, Alberdi Ibáñez I, Alvarez López A, García-Asensio S. Helical CT cholangiography in the evaluation of the biliary tract: application to the diagnosis of choledocholithiasis. Abdom Imaging. 2002;27:61-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Jiménez Cuenca I, del Olmo Martínez L, Pérez Homs M. Helical CT without contrast in choledocholithiasis diagnosis. Eur Radiol. 2001;11:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Takahashi M, Saida Y, Itai Y, Gunji N, Orii K, Watanabe Y. Reevaluation of spiral CT cholangiography: basic considerations and reliability for detecting choledocholithiasis in 80 patients. J Comput Assist Tomogr. 2000;24:859-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Romagnuolo J, Bardou M, Rahme E, Joseph L, Reinhold C, Barkun AN. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. 2003;139:547-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 264] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 23. | Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, Francis IR, Nandi PS. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. Am J Gastroenterol. 2001;96:2900-2904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 24. | Ledro-Cano D. Suspected choledocholithiasis: endoscopic ultrasound or magnetic resonance cholangio-pancreatography? A systematic review. Eur J Gastroenterol Hepatol. 2007;19:1007-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Liu CL, Fan ST, Lo CM, Tso WK, Wong Y, Poon RT, Lam CM, Wong BC, Wong J. Comparison of early endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the management of acute biliary pancreatitis: a prospective randomized study. Clin Gastroenterol Hepatol. 2005;3:1238-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Li MK, Tang CN, Lai EC. Managing concomitant gallbladder stones and common bile duct stones in the laparoscopic era: a systematic review. Asian J Endosc Surg. 2011;4:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2006;CD003327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 130] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 28. | Cociorvei A, Calu V. [Laparoscopic ultrasound in biliary diseases]. Chirurgia (Bucur). 2011;106:353-358. [PubMed] |
| 29. | Rhodes M, Sussman L, Cohen L, Lewis MP. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 288] [Article Influence: 10.7] [Reference Citation Analysis (1)] |
| 30. | Johnson PM, Walsh MJ. The impact of intraoperative cholangiography on recurrent pancreatitis and biliary complications in patients with gallstone pancreatitis. J Gastrointest Surg. 2012;16:2220-2224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Lepner U, Grünthal V. Intraoperative cholangiography can be safely omitted during laparoscopic cholecystectomy: a prospective study of 413 consecutive patients. Scand J Surg. 2005;94:197-200. [PubMed] |
| 32. | Ito K, Ito H, Tavakkolizadeh A, Whang EE. Is ductal evaluation always necessary before or during surgery for biliary pancreatitis? Am J Surg. 2008;195:463-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Working Party of the British Society of Gastroenterology; Association of Surgeons of Great Britain and Ireland; Pancreatic Society of Great Britain and Ireland; Association of Upper GI Surgeons of Great Britain and Ireland. UK guidelines for the management of acute pancreatitis. Gut. 2005;54 Suppl 3:iii1-iii9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 330] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 34. | Ko CW, Sekijima JH, Lee SP. Biliary sludge. Ann Intern Med. 1999;130:301-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 127] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 35. | Dahan P, Andant C, Lévy P, Amouyal P, Amouyal G, Dumont M, Erlinger S, Sauvanet A, Belghiti J, Zins M. Prospective evaluation of endoscopic ultrasonography and microscopic examination of duodenal bile in the diagnosis of cholecystolithiasis in 45 patients with normal conventional ultrasonography. Gut. 1996;38:277-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 107] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 36. | Geenen JE, Nash JA. The role of sphincter of Oddi manometry and biliary microscopy in evaluating idiopathic recurrent pancreatitis. Endoscopy. 1998;30:A237-A241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Lee SP, Nicholls JF, Park HZ. Biliary sludge as a cause of acute pancreatitis. N Engl J Med. 1992;326:589-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 311] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 38. | Kozarek R. Role of ERCP in acute pancreatitis. Gastrointest Endosc. 2002;56:S231-S236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Ros E, Navarro S, Bru C, Garcia-Pugés A, Valderrama R. Occult microlithiasis in ‘idiopathic’ acute pancreatitis: prevention of relapses by cholecystectomy or ursodeoxycholic acid therapy. Gastroenterology. 1991;101:1701-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 40. | Hernandez L, Catalano M. Endoscopic Techniques (ERCP, EUS) for the Evaluation of Unexplained Acute Pancreatitis. Techn in Gastrointestinal Endoscopy. 2004;6:84-90. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |