Published online Nov 14, 2014. doi: 10.3748/wjg.v20.i42.15937
Revised: August 29, 2014
Accepted: September 29, 2014
Published online: November 14, 2014
Processing time: 151 Days and 15.8 Hours
Endoscopic variceal obturation of gastric varices with tissue glue is considered the first choice for management of gastric varices, and is usually safe and effective. However, there is still a low incidence of complications and some are even fatal. Here, we present a case in which endoscopic variceal ligation caused laceration of the esophageal varicose vein with tissue glue emboli and massive bleeding after 3 mo. Cessation of bleeding was achieved via variceal sclerotherapy using a cap-fitted gastroscope. Methods of recognizing an esophageal varicose vein with tissue glue plug are discussed.
Core tip: Complications can occur during and after treatment of gastric varices via endoscopic variceal obturation with tissue glue. Laceration of the esophageal varicose vein with tissue glue emboli and massive bleeding caused by endoscopic variceal ligation are reported here. Cap-fitted gastroscopy may be helpful in sclerotherapy for cardiac varices by providing better endoscopic vision.
- Citation: Wei XQ, Gu HY, Wu ZE, Miao HB, Wang PQ, Wen ZF, Wu B. Endoscopic variceal ligation caused massive bleeding due to laceration of an esophageal varicose vein with tissue glue emboli. World J Gastroenterol 2014; 20(42): 15937-15940
- URL: https://www.wjgnet.com/1007-9327/full/v20/i42/15937.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i42.15937
Endoscopic variceal obturation of gastric varices with tissue glue is considered the first choice for management of gastric varices, and is usually safe and effective. There is still a low incidence of complications and some are even fatal. Here, we present a case in which endoscopic variceal ligation (EVL) caused laceration of the esophageal varicose vein with tissue glue emboli and massive bleeding 3 mo after the treatment. Hemostasis was achieved via sclerotherapy of the bleeding varices through cap-fitted gastroscopy. More accurate methods of recognizing an esophageal varicose vein with tissue glue plug should be provided.
A 54-year-old woman was admitted to our department on September 5, 2013 upon her first episode of severe upper gastrointestinal bleeding presenting with hematemesis and melena. She had been on regular lamivudine-based therapy for hepatitis-B-virus-related decompensated liver cirrhosis for 4 years, and had a history of partial splenic arterial embolization for hypersplenism for 3 years. Esophagogastroduodenoscopy (EGD) was performed when she had stable vital signs, with cessation of bleeding after successful internal therapy. Severe Sarin type 2 gastroesophageal varices[1] with obvious red color signs on both gastric varices (GVs) and esophageal varices (EVs) and mild portal hypertensive gastropathy were observed. The largest GV was approximate 12 mm in diameter. Three pericardial GVs with red color signs were obturated with 3, 2 and 2 mL of homogenous tissue glue mixtures of N-butyl-2-cyanoacrylate (Histoacryl) and lipiodol with a ratio of 1:1, via a standardized injection method as secondary prophylaxis[2]. No complication of ectopic embolism was observed on plain chest X-ray film after the procedure. For further treatment of the EVs, monthly follow-up EGD was suggested, however, the patient returned at 1 and 3 mo after the first endoscopic therapy. The patient underwent EVL at the most severe sites using Wilson-Cook 6 Shooter multi-band ligator during her second EGD.
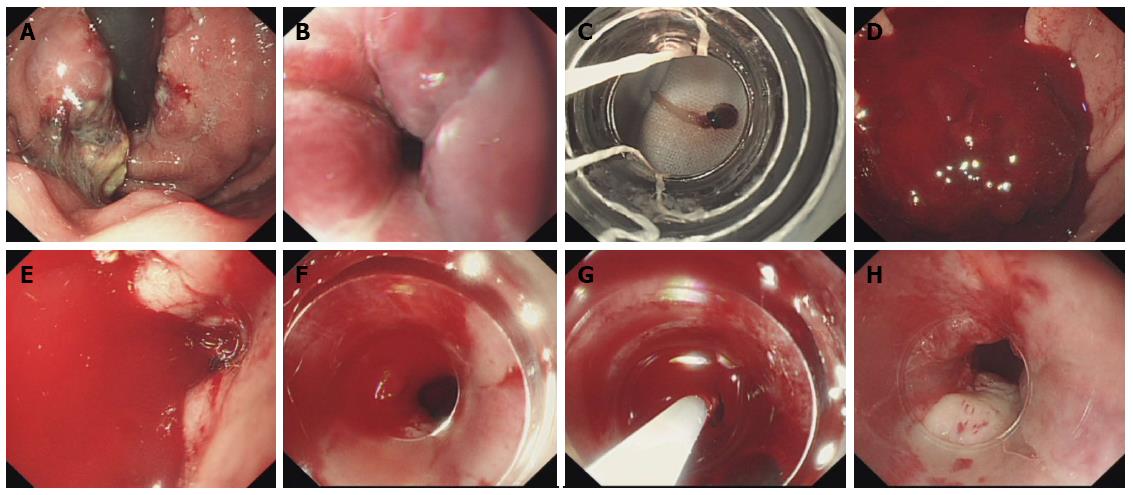
On December 9, 2013, the third EGD was performed and EVL was planned to eliminate some of the remaining EVs as a part of the sequential therapy. Some extruded glue was observed in the gastric fundus (Figure 1A). An EV that was continuous with the GV on the greater curvature of the stomach was picked up as the first EV to be ligated. Grossly, this vein was straight, blue in color, approximate 9 mm in diameter, and mild red color signs was observed on its surface (Figure 1B). It was similar in endoscopic appearance with the numerous other EVs that we have observed in our experience of > 10 years. The ligation site was approximate 5 mm proximal to the Z-line and 38 cm from the incisor. By suction with a regular negative pressure of 0.04 kPa, a nodular variceal protrusion bulb was formed in the cavity of the transparent cap, however, the bulb could not be released from the cavity. We then put the handle button into a two way mode and released the handling string. We also tried to wash out the bulb through the air flow and water flow, but we still failed to release the bulb from the cap cavity and the endoscopic field of vision was lost. We had to withdraw the endoscope gently and a tadpole-shaped, semi-transparent substance adhering to the transparent cap was found. It was approximate 10 mm long and approximate 3 mm in diameter and was identified as a piece of soft, semi-solidified tissue glue partially covered by a small piece of mucosa and blood vessel wall (Figure 1C). Hematemesis developed and the patient’s blood pressure dropped suddenly to 70/50 mmHg. These signs suggested that, despite its normal-like appearance, the targeted EV had carried a large amount of tissue glue that was extended from the GVs, and suction of this special EV with a tissue glue plug had torn its vessel wall and caused massive upper gastrointestinal bleeding.
Intravenous fluids and transfusion were started immediately for volume expansion and vital signs were monitored closely. We then took off the ligator system and inserted the endoscope again, and massive bleeding was observed (Figure 1D). However, a clear endoscopic view was not possible (Figure 1E), because the bleeding was too massive and vision was blurred by the high tension in the luminal wall and frequent peristaltic movement of the gastric cardia, which can often result from close contact of the mucosa with the front end of the endoscope. The responsible vein had to be empirically located and 5 mL of 1% aethoxysklerol was injected intravenously at the site, approximate 36 cm from the incisor, however, this turned out to be ineffective because the bleeding was not stemmed. Endoscopy was then performed with the aid of a transparent cap with the rigid front-end part of 10 mm left outside, and a better endoscopic view was achieved by pressing against the esophageal wall with the transparent cap. Blood was seen spurting from the ruptured EV, which was approximate 5 mm proximal to the Z-line and 38 cm from the incisor. The site of the vein responsible for the bleeding was located precisely (Figure 1F), and a further 10 mL 1% aethoxysklerol was injected intravenously with the aid of the transparent cap (Figure 1G). The bleeding eventually ceased (Figure 1H) and there was no re-bleeding after the procedure. The patient was prescribed 10 mg propranolol three times daily 1 wk later and she has been well since then. We suggested construction of a transjugular intrahepatic portosystemic shunt, however, the patient has not yet received this.
GVs are present in 5%-30% of patients with portal hypertension, and the overall incidence of bleeding caused by variceal rupture varies from 3% to 30%[3,4]. Endoscopic variceal obturation of GVs with tissue glue is considered the first choice for management of GVs[5]. Although the incidence of complications from endoscopic GV obturation with tissue glue is low, there are still some complications that may include abdominal pain, massive intraoperative bleeding, rebleeding due to early-onset extrusion of tissue glue cast, giant gastric ulcer, sepsis, and distant embolization[6]. Ectopic emboli may occur in the brain, lung, kidney, right atrium and portal vein, and may be fatal[6-8]. Here, we report a case in which massive bleeding was due to laceration by EVL of the esophageal varicose vein with a tissue glue plug. To the best of our knowledge, this is the first report of this complication. The tissue glue plug in the esophageal varicose vein should be formed by tissue glue that was extended from the gastric varicose vein with injection of N-butyl-2-cyanoacrylate. Therefore, ligation of a varicose vein with a tissue glue plug can be dangerous, and there raises a question about how to differentiate a varicose vein with a tissue glue plug from that without a plug.
Cipolletta et al[9] have reported treatment of acutely bleeding EVs using tissue glue injection followed by EVL, however, they have not described how to recognize the glue plug. Usually, when we perform EVL in a patient with a history of tissue glue injection for GVs, we compress the varicose vein gently using the transparent cap to establish whether it is hard. The ligation site should be at least 5-10 mm proximal to the Z-line and the suction should be performed slowly and gently with a relatively lower suction pressure so that we can determine whether the nodular variceal protrusion bulb is formed easily. If it is felt that the esophageal varicose vein is too hard when it is compressed with the transparent cap, or if the nodular variceal protrusion bulb cannot be formed easily, the procedure should be stopped and another ligation site should be selected. On the present occasion, we failed to recognize the plug since the glue was still soft, and the esophageal varicose vein was torn by the ligation band and massive bleeding occurred. More accurate methods of recognizing esophageal varicose vein tissue with glue plug should be provided. In theory, plain computed tomography (CT) combined with 2D or 3D CT venography after tissue glue injection provides detailed information[10]. Endoscopic ultrasound (EUS)-guided transesophageal treatment of gastric fundal varices, with combined coiling and cyanoacrylate glue injection, and EUS-guided treatment of bleeding duodenal varices have been used to judge the adequacy of endoscopic therapy by demonstrating absence of blood flow in the varices[11,12]. Therefore, EUS can help to determine whether there is a glue embolus in the EV. However, this kind of work has not yet been done.
The endoscopic vision is often blurred by the high tension in the luminal wall and frequent peristaltic movement of the cardia, which can result from close contact of the mucosa with the front end of the endoscope[13]. Cap-fitted gastroscopy improves visualization and targeting of lesions and improves biopsy accuracy in Barrett’s esophagus[13,14]. Here, we showed that with the help of a transparent cap, visualization of the cardiac area was improved, even in the situation of massive bleeding and targeting of the bleeding varices became easier and more accurate. Cap-fitted gastroscopy seems to be helpful in sclerotherapy for cardiac varices, however, this needs confirmation from more studies specifically for EVs treatment in the future.
In the present case, cessation of bleeding was achieved via endoscopic variceal sclerotherapy. However, if endoscopic variceal sclerotherapy fails to work, what should be done? There are only a few reports in the literature of the same complication. According to experience with management of massive bleedings caused by gastroesophageal varices rupture, we think that the Sengstaken-Blakemore tube should be used, followed by transjugular intrahepatic portosystemic shunt or surgery.
In conclusion, EV embolization can occur when tissue glue injection is used to obturate the gastric fundal varices of the gastroesophageal varices. Varicose vein ligation with a tissue glue plug can be dangerous and severe bleeding may occur. A more accurate method of recognizing the tissue glue plug in an esophageal varicose vein should be provided. Cap-fitted gastroscopy may be helpful in sclerotherapy for cardiac varices.
A 54-year-old woman presented with massive upper gastrointestinal bleeding due to laceration of an esophageal varicose vein with tissue glue emboli.
Massive gastrointestinal bleeding caused by laceration of an esophageal varicose vein with tissue glue emboli.
Spontaneous rupture of esophageal varices.
The diagnosis of this case did not depend on laboratory tests.
During the procedure of endoscopic variceal ligation, laceration of an esophageal varicose vein with tissue glue emboli and a tadpole-shaped, semi-transparent substance adhering to the transparent cap were found.
Pathological examinations were not required to make the diagnosis in this case.
Massive bleeding due to laceration of an esophageal varicose vein with tissue glue emboli was stopped by variceal sclerotherapy using a cap-fitted gastroscope.
No previous report was found of bleeding due to laceration of an esophageal varix during ligation that might be attributed to the presence of glue in the lumen.
Cap-fitted endoscopy means that the examination is performed with the aid of a transparent cap fitted to the front-end of the endoscope.
Esophageal varicose vein with tissue glue emboli can occur after endoscopic variceal obturation of gastric varices. Laceration of this kind of varix and massive bleeding can be caused by endoscopic variceal ligation.
A rare case of massive bleeding due to the laceration of an esophageal varicose vein with tissue glue emboli was ceased by cap-fitted endoscopic variceal sclerotherapy. The utility of recognizing the presence of glue in the varix by endoscopic ultrasound needs to be confirmed.
P- Reviewer: Cardoso CRL, Lai YC, Ranieri G, Wang K S- Editor: Qi Y L- Editor: A E- Editor: Ma S
| 1. | Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-1349. [PubMed] |
| 2. | Seewald S, Ang TL, Imazu H, Naga M, Omar S, Groth S, Seitz U, Zhong Y, Thonke F, Soehendra N. A standardized injection technique and regimen ensures success and safety of N-butyl-2-cyanoacrylate injection for the treatment of gastric fundal varices (with videos). Gastrointest Endosc. 2008;68:447-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 116] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Toubia N, Sanyal AJ. Portal hypertension and variceal hemorrhage. Med Clin North Am. 2008;92:551-74, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175-1189. [PubMed] |
| 5. | Park WG, Yeh RW, Triadafilopoulos G. Injection therapies for variceal bleeding disorders of the GI tract. Gastrointest Endosc. 2008;67:313-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Cheng LF, Wang ZQ, Li CZ, Lin W, Yeo AE, Jin B. Low incidence of complications from endoscopic gastric variceal obturation with butyl cyanoacrylate. Clin Gastroenterol Hepatol. 2010;8:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 7. | Miyakoda K, Takedatsu H, Emori K, Inoue H, Toyonaga A, Mitsuyama K, Tsuruta O, Sata M. N-butyl-2-cyanoacrylate (histoacryl) glue in the right atrium after endoscopic injection for a ruptured duodenal varix: complication of histoacryl injection. Dig Endosc. 2012;24:192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Chang CJ, Shiau YT, Chen TL, Hou MC, Sun CH, Liao WC, Lin HC, Lee SD. Pyogenic portal vein thrombosis as a reservoir of persistent septicemia after cyanoacrylate injection for bleeding gastric varices. Digestion. 2008;78:139-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Cipolletta L, Zambelli A, Bianco MA, De Grazia F, Meucci C, Lupinacci G, Salerno R, Piscopo R, Marmo R, Orsini L. Acrylate glue injection for acutely bleeding oesophageal varices: A prospective cohort study. Dig Liver Dis. 2009;41:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Chen TW, Yang ZG, Li X, Wang QL, Qian LL, Wang RR. Evaluation of entire gastric fundic and esophageal varices secondary to posthepatitic cirrhosis: portal venography using 64-row MDCT. Abdom Imaging. 2010;35:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Iwase H, Suga S, Morise K, Kuroiwa A, Yamaguchi T, Horiuchi Y. Color Doppler endoscopic ultrasonography for the evaluation of gastric varices and endoscopic obliteration with cyanoacrylate glue. Gastrointest Endosc. 1995;41:150-154. [PubMed] |
| 12. | Rana SS, Bhasin DK, Rao C, Singh K. Endoscopic ultrasound-guided treatment of bleeding duodenal varix. Indian J Gastroenterol. 2011;30:280-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Chen BL, Xing XB, Wang JH, Feng T, Xiong LS, Wang JP, Cui Y. Improved biopsy accuracy in Barrett’s esophagus with a transparent cap. World J Gastroenterol. 2014;20:4718-4722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Yap CK, Ng HS. Cap-fitted gastroscopy improves visualization and targeting of lesions. Gastrointest Endosc. 2001;53:93-95. [PubMed] |