Published online Nov 14, 2014. doi: 10.3748/wjg.v20.i42.15916
Revised: June 3, 2014
Accepted: June 14, 2014
Published online: November 14, 2014
Processing time: 243 Days and 12 Hours
An endoscopic or radiologic percutaneous approach may be an initial minimally invasive method for treating biliary strictures after living donor liver transplantation; however, cannulation of biliary strictures is sometimes difficult due to the presence of a sharp or twisted angle within the stricture or a complete stricture. When an angulated or twisted biliary stricture interrupts passage of a guidewire over the stricture, it is difficult to replace the percutaneous biliary drainage catheter with inside stents by endoscopic retrograde cholangiopancreatography. The rendezvous technique can be used to overcome this difficulty. In addition to the classical rendezvous method, in cases with complete transection of the common bile duct a modified technique involving the insertion of a snare into the subhepatic space has been successfully performed. Herein, we report a modified rendezvous technique in the duodenal bulb as an extraordinary location for a patient with duct-to-duct anastomotic complete stricture after liver transplantation.
Core tip: An endoscopic-radiologic rendezvous technique may be used for stent application in the treatment of biliary strictures where previous endoscopic retrograde cholangiopancreatography and percutaneous transhepatic attempts have failed. Recently, it was reported that successful endoscopic-radiologic rendezvous procedures were performed in the subhepatic space in patients with complete transections of the common bile duct, especially secondary to surgical injury. Herein, we report a modified rendezvous technique in the duodenal bulb as an extraordinary location in a patient with a duct-to-duct complete anastomotic stricture after liver transplantation.
- Citation: Odemis B, Oztas E, Yurdakul M, Torun S, Suna N, Kayacetin E. Interesting rendezvous location in a liver transplantation patient with anastomosis stricture. World J Gastroenterol 2014; 20(42): 15916-15919
- URL: https://www.wjgnet.com/1007-9327/full/v20/i42/15916.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i42.15916
Biliary strictures are not uncommon after living donor liver transplantation (LDLT), and two-thirds of biliary strictures can be treated by endoscopic retrograde cholangiopancreatography (ERCP). If ERCP fails, percutaneous transhepatic biliary drainage (PTBD) is recommended[1,2]. Although maintaining a PTBD catheter for a long period is beneficial for treating biliary strictures, it may be difficult for patients, especially in liver transplant patients, due to the development of PTBD catheter-related complications, such as leakage, pain, infection, and accidental removal of the PTBD catheter. Therefore, replacing PTBD catheters with inside stents is recommended. When an angulated or twisted biliary stricture interrupts passage of a guidewire over the stricture, it is difficult to replace the PTBD catheter with inside stents by ERCP[3]. The rendezvous technique can be used to overcome this difficulty. The rendezvous procedure is classically performed after transhepatic advancement of a guidewire through the papilla for subsequent ERCP[4,5]. In addition to this classical rendezvous method, in cases with complete transection of the common bile duct (CBD), a modified technique involving the insertion of a snare into the subhepatic space has been successfully performed[6,7]. Herein, we report a modified rendezvous technique in the duodenal bulb as an extraordinary location in a patient with a duct-to-duct complete anastomotic stricture after liver transplantation.
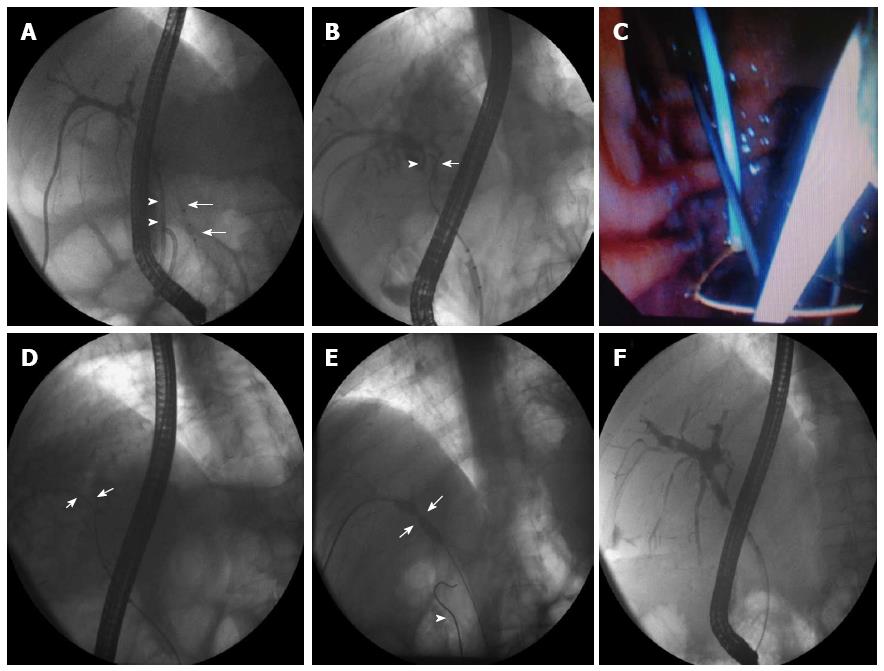
A 53-year-old-man was admitted to our clinic for removal of a percutaneous internal-external biliary drainage catheter and insertion of stents via ERCP. He had a history of right lobe LDLT due to hepatitis B-related cirrhosis and hepatocellular carcinoma three years ago. After a short time, a duct-to-duct anastomotic stricture developed. Because cannulation of the intrahepatic bile ducts via ERCP was unsuccessful, an internal-external biliary drainage catheter was inserted after balloon dilatation of the stricture via percutaneous transhepatic cholangiography (PTC). The biliary drainage catheter was kept in place, and the patient had undergone balloon dilatation of the stricture via a transhepatic route five times in the previous seven months. After admission to our clinic, ERCP was performed. At the beginning of ERCP, the tip of the internal-external biliary drainage catheter was protruding from the apex of the bulbus, an astonishing endoscopic finding. Intrahepatic bile ducts could not be opacified after a balloon (Anrei Medical Co. Ltd Hangzhou, China) occluded cholangiography obtained through the papilla, and all attempts at advancing a guidewire (0.035 inch VisiGlide, Olympus Europa Holding GMBH Hamburg, Germany) proximally into the intrahepatic bile ducts failed (Figure 1A, B). On a simultaneous PTC, a guidewire could not be advanced into the CBD despite several attempts (Figure 1B). These findings indicated complete stenosis of the anastomosis during the previous year; therefore, we resolved these problems by performing a modified rendezvous technique. A guidewire inserted through the papilla was intentionally pushed strongly into the paracholedochal space at the level of the stricture, which was then spontaneously advanced into the bulbus of the duodenum alongside the biliary drainage catheter. Later, a snare (Micro-Tech Nanjing Co. Ltd. Hamburg, Germany) was slowly introduced via the transhepatic route into the bulbus and the guidewire was caught by closing the snare under endoscopic visualization (Figure 1C). The guidewire was pulled proximally all the way through the percutaneous access (Figure 1D). This was followed by a 5 and 7 mm balloon (Ventura biliary dilatation catheter, Panmedikal, Gloucester, United Kingdom), dilatation of the stricture (Figure 1E) and placement of an internal-external biliary drainage catheter through the papilla. Two weeks later, the drainage catheter was removed and two biliary plastic stents (Erdamed Biliary Stent, Istanbul, Turkey) were inserted into the right anterior and posterior segments of the liver via ERCP. In the third month of follow-up, the stricture was almost completely resolved and the patient was then followed stent-free (Figure 1F).
There have been no other reports in the literature regarding the misplacement of the internal portion of the percutaneous internal-external drainage catheter to the duodenal bulb, and this case was the first in our clinic. In patients with liver transplantation, placement of the PTBD catheter in the wrong location, such as the duodenal bulb as in our case, can cause several complications, such as leakage, pain, infection, and accidental removal of the PTBD catheter. Two alternatives can be performed in such cases in which transpapillary cannulation of the intrahepatic bile ducts is not possible because of complete stenosis of the anastomosis. The first option is to accept the overall risks and to live with the PTBD catheter, and the second is surgery. The rendezvous procedure is classically performed after transhepatic advancement of a guidewire through the papilla for subsequent ERCP[5]. In a recent report, Fiocca et al[6] performed a 100% successful endoscopic-radiologic rendezvous procedure in the subhepatic space in patients with complete transection of the common bile duct. We also successfully performed this technique in another patient with a complete transection of the CBD due to previous cholecystectomy[7]. This experience encouraged us to perform the same endoscopic-radiologic rendezvous technique in the duodenal bulb. The procedure was successful, and we avoided the possible risks that may develop due to PTBD or surgery. We suggest that the rendezvous technique can be performed as an initial method for treating similar biliary complications after liver transplantation.
A 53-year-old-man with a history of right lobe living donor liver transplantation (LDLT) due to hepatitis B-related cirrhosis and hepatocellular carcinoma three years ago was admitted to our clinic for removal of a percutaneous internal-external biliary drainage catheter and with the complaint of pruritis.
The signs were scratch wounds on the skin secondary to pruritis, large abdominal scar due to previous liver transplantation and a percutaneous biliary drainage catheter on the abdomen.
Stricture of the biliary anastomosis, biliary injury, ischemic cholangiopathy, chronic rejection, posttransplantation disease recurrence.
Hemoglobin: 11.5 g/dL; aspartate aminotransferase: 99 U/L; alanine aminotransferase: 87 U/L; alkaline phosphatase: 475 U/L; glutamyltransferase: 155 U/L; total bilirubin: 1.8 mg/dL; direct bilirubin: 1.4 mg/dL; other laboratory tests were within normal limits.
The tip of the internal-external biliary drainage catheter was protruding from the bulbus during endoscopic retrograde cholangiopancreatography (ERCP) and a stricture blocking advance of the guidewire proximally was recorded on cholangiography.
Pathological examination was not performed.
After passage between the proximal and distal segments of the bulbus was achieved via the endoscopic-radiologic rendezvous method, balloon dilatation of the stricture and placement of an internal-external biliary drainage catheter through the papilla were performed.
Biliary strictures are common in LDLT patients, and ERCP, percutaneous transhepatic cholangiography or, infrequently, surgical management is necessary for treatment.
This case report suggests that an endoscopic radiologic rendezvous technique can be performed as an alternative method for treating biliary strictures in which the conventional endoscopic and radiologic methods have failed after liver transplantation, even if the rendezvous localization is the duodenal bulb. This procedure should be considered before invasive management options, such as surgery.
The endoscopic radiologic rendezvous technique is a viable alternative method for treating biliary strictures, especially in patients with liver transplantation.
P- Reviewer: Sakai Y S- Editor: Gou SX L- Editor: Webster JR E- Editor: Liu XM
| 1. | Yazumi S, Yoshimoto T, Hisatsune H, Hasegawa K, Kida M, Tada S, Uenoyama Y, Yamauchi J, Shio S, Kasahara M. Endoscopic treatment of biliary complications after right-lobe living-donor liver transplantation with duct-to-duct biliary anastomosis. J Hepatobiliary Pancreat Surg. 2006;13:502-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 106] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Kim ES, Lee BJ, Won JY, Choi JY, Lee DK. Percutaneous transhepatic biliary drainage may serve as a successful rescue procedure in failed cases of endoscopic therapy for a post-living donor liver transplantation biliary stricture. Gastrointest Endosc. 2009;69:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Sharma S, Gurakar A, Jabbour N. Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 2008;14:759-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 275] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 4. | Aytekin C, Boyvat F, Yimaz U, Harman A, Haberal M. Use of the rendezvous technique in the treatment of biliary anastomotic disruption in a liver transplant recipient. Liver Transpl. 2006;12:1423-1426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Chang JH, Lee IS, Chun HJ, Choi JY, Yoon SK, Kim DG, You YK, Choi MG, Choi KY, Chung IS. Usefulness of the rendezvous technique for biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. Gut Liver. 2010;4:68-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Fiocca F, Salvatori FM, Fanelli F, Bruni A, Ceci V, Corona M, Donatelli G. Complete transection of the main bile duct: minimally invasive treatment with an endoscopic-radiologic rendezvous. Gastrointest Endosc. 2011;74:1393-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Ödemiş B, Shorbagi A, Köksal AŞ, Özdemir E, Torun S, Yüksel M, Kayaçetin E. The “Lasso” technique: snare-assisted endoscopic-radiological rendezvous technique for the management of complete transection of the main bile duct. Gastrointest Endosc. 2013;78:554-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |