Published online Nov 14, 2014. doi: 10.3748/wjg.v20.i42.15476
Revised: February 19, 2014
Accepted: June 13, 2014
Published online: November 14, 2014
Processing time: 375 Days and 14.5 Hours
Hepatitis C is a liver disease that is transmitted through contact with the blood of an infected person. An estimated 150 million individuals worldwide have been chronically infected with the hepatitis C virus (HCV). Hepatitis C shows significant genetic variation in the global population, due to the high rate of viral RNA mutation. There are six variants of the virus (HCV genotypes 1, 2, 3, 4, 5, and 6), with 15 recorded subtypes that vary in prevalence across different regions of the world. A variety of devices are used to diagnose hepatitis C, including HCV antibody test, HCV viral load test, HCV genotype test and liver biopsy. Rapid, inexpensive, sensitive, and robust analytical devices are therefore essential for effective diagnosis and monitoring of disease treatment. This review provides an overview of current electrochemical immunosensor and genosensor technologies employed in HCV detection. There are a limited number of publications showing electrochemical biosensors being used for the detection of HCV. Due to their simplicity, specificity, and reliability, electrochemical biosensor devices have potential clinical applications in several viral infections.
Core tip: The global market for hepatitis C virus (HCV) treatment will reach $20 billion annually by the end of the decade. Therefore, a considerable interest in developing simple and reliable methods for detecting and quantifying HCV is required. Conventional HCV diagnostic tests include virus isolation, immunofluorescence microscopy, enzyme immunoassays and polymerase chain reaction techniques are becoming obsolete for routine clinical practices. In this issue, the current knowledge on the alternative diagnostic devices for HCV detection is updated, addressing all the topics with a practical point of view to make this “Topic Highlight” interesting and useful to most clinicians.
- Citation: Uliana CV, Riccardi CS, Yamanaka H. Diagnostic tests for hepatitis C: Recent trends in electrochemical immunosensor and genosensor analysis. World J Gastroenterol 2014; 20(42): 15476-15491
- URL: https://www.wjgnet.com/1007-9327/full/v20/i42/15476.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i42.15476
Hepatitis C virus (HCV) infection is a global health problem[1]. HCV is a small (36-65 nm in size) and positive-sense single-stranded RNA virus[2]. It can be transmitted through contact with the blood of an infected person, organ transplantations, blood transfusions, renal dialysis, and intravenous drug abuse[3]. An estimated 2%-3% of the world’s population, corresponding to approximately 130-170 million persons, has been infected with HCV[4]. Although recent advances in the treatment of HCV genotype 1 infection using directly acting antiviral agents are encouraging, there is still a need to develop vaccine strategies capable of preventing infection[5].
HCV infection has low cure rates and causes serious adverse effects in some patients, with chronic infections including cirrhosis and hepatocellular carcinoma[6]. Accurate and sensitive diagnosis in the early stages of HCV infection is important[7]; past HCV infection has no significant influence on the risk of hepatocellular carcinoma[8].
Research into new cost-effective and validated techniques is ongoing, and aims to inform the best practices for detecting HCV infection and for distinguishing between a resolved HCV infection and a false positive for HCV antibody in patients with levels of HCV RNA that are not detectable. The understanding of HCV diagnostic strategies is important in order to be able to provide comprehensive guidance on testing, reporting, and clinical management, and will improve case definitions for disease notification and surveillance.
Serological and virological tests have become essential in the management of HCV infection in order to diagnose infection, plan treatment, and assess the virological response to antiviral therapy. Virological tools include anti-HCV antibody detection, serological determination of the HCV genotype, and molecular assays that detect and quantify HCV RNA and determine the HCV genotype. Anti-HCV antibody testing and HCV RNA testing are used to diagnose acute and chronic hepatitis C. Only patients with detectable HCV RNA should be considered for pegylated interferon-alpha and ribavirin therapy, and the HCV genotype should be systematically characterized before treatment, as it determines the type and duration of treatment, the dose of ribavirin, and the virological monitoring procedure. HCV RNA monitoring during therapy is used to tailor the duration of treatment in HCV genotype 1 infection, and molecular assays are used to establish the end of treatment and, most importantly, the sustained virological response (in other words, the therapy endpoint)[9].
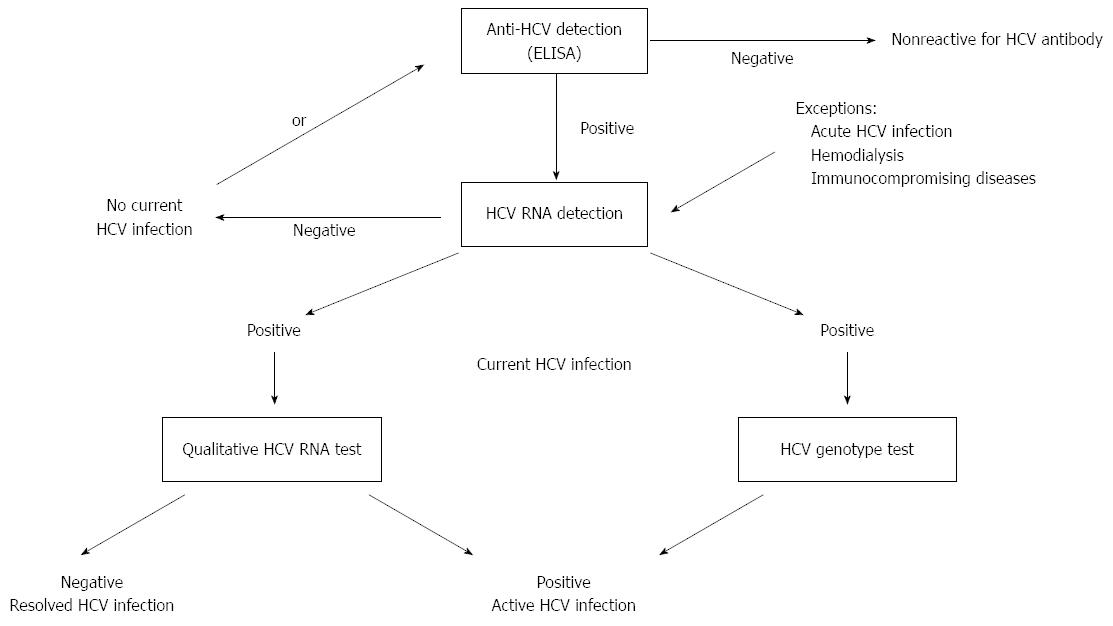
The most commonly used assay for anti-HCV is the enzyme-linked immunosorbent assay (ELISA, Figure 1). The advantages of this technique include automation, highly reproducible results, and low cost. Three generations of ELISA for anti-HCV have been developed over the past decade.
The first generation of HCV ELISAs, reported in 1989, was produced using recombinant proteins complementary to the NS4 region of the HCV genome, and was used for HCV antibody screening of blood donations[10]. These tests had limited sensitivity and specificity. In the procedure, single recombinant antigens from the NS4 region of the HCV genome are immobilized in the wells of a microtiter plate. The presence of anti-HCV antibodies is revealed by anti-antibodies labeled with an enzyme that catalyzes the transformation of the substrate into a colored compound that can be measured by spectrophotometry[11].
Gray and Wreghitt (1989)[12] reported an adaptation of a first generation ELISA for detecting anti-HCV to differentiate nonspecific (low avidity) antibody binding from specific (high avidity) binding by antibodies generated during long-term infection.
Second generation tests have included recombinant/synthetic antigens from the core and nonstructural NS3 and NS4 regions of the HCV genome. This immunoassay improved the sensitivity and specificity of the test. Furthermore, it has proved to be quite effective as a screening test in individuals who are high-risk for chronic hepatitis C. Approximately 92%-95% of chronic hepatitis C cases can be detected by second generation ELISA. Finally, the anti-HCV can be detected approximately 10 wk after the initial infection, compared to an average of 16 wk using the first generation ELISA[13].
Clinical studies have shown a significant number of HCV-infected individuals who developed antibodies to the NS5 non-structural protein of the virus. Therefore, the third generation tests include antigens from the NS5 region of the viral genome, in addition to NS3, NS4, and the core[14-16]. The third generation tests provide improved sensitivity and have shortened the antibody detection period to around 5 wk[17]. The specificity of the anti-HCV assay (3rd generation) was found to be 99.5% for blood donor samples and 99.4% for routine clinical specimens[18].
Ward et al[19] (1994) reported a modified anti-HCV ELISA to show that anti-HCV avidity in dialysis patients increases with time after primary infection. Furthermore, it was observed that patients given immunosuppressive therapy did not show a progressive increase in anti-HCV antibody avidity, as was observed for non-immunosuppressed controls, suggesting that immunosuppression slows the maturation of IgG avidity[12,19]. Kanno and Kazuyama[20] (2002) reported that anti-HCV avidity was lower in sera taken from patients with resolved infection than in sera from chronically infected patients, and that the avidity index declined in the latter after treatment with interferon.
Detection of anti-HCV antibodies is unable to distinguish between a current or past infection, because people will retain anti-HCV antibodies for life once they have been exposed to HCV[21]. In addition, the testing for anti-HCV antibodies might provide false negative results, because it takes 45-68 d to develop anti-HCV antibodies following HCV infection[22]. On the other hand, detection of HCV RNA can distinguish between a current or past infection. However, detection of HCV RNA could provide false positive results due to contamination. It is also too expensive and labor-intensive for routine use. It has been reported that the HCV core antigen can be detected in the serum of most patients during the acute infection[23,24].
HCV core antigen levels correlate well with HCV RNA levels, and may consequently be used as an indirect marker of HCV replication, in a low-cost alternative technique for diagnosis of acute HCV infection[25-29]. The HCV core antigen has been reported to appear earlier than the anti-HCV antibody, and may be detected within 1 or 2 d following the appearance of HCV RNA in serum[30-32].
Effective treatment is available for HVC infection, but since the disease is asymptomatic, most people with HCV do not know they are infected. Since 1998, the Center for Disease Control and Prevention (CDC) has recommended HCV testing for persons with risk factors for HCV infection[33]. The recommended testing sequence for detection of current HCV infection is shown in Figure 1. Firstly, the presence of anti-HCV antibodies in a blood sample is evaluated. A non-reactive test result indicates the absence of HCV infection. If the individual is suspected to have been exposed to HCV, a HCV RNA test is recommended.
An HCV antibody reaction is assumed to be indicative of an infection, and subsequent supplementary anti-HCV or HCV RNA tests are required. A repeated reactive result is consistent with a current HCV infection, a resolved HCV infection, or a false positive result for HCV antibodies. The test for HCV RNA is evaluated in order to confirm current infection. If the data are indicative of an HCV reaction and HCV RNA is detected, the individual has a current HCV infection. All patients should have a baseline HCV RNA level measured prior to starting treatment. If the data are indicative of an HCV reaction and HCV RNA is not detected, then there is no current HCV infection. If distinction between true and false positivity for HCV antibodies is desired, and if the sample is repeatedly reactive in the initial test, supplementary HCV antibody assays are recommended. This is also the case if the person tested is suspected of having had exposure to HCV within the past 6 mo, has clinical evidence of HCV disease, or if there is concern regarding the handling or storage of the test specimen[34].
In 2003, CDC published guidelines for the laboratory testing of antibodies to HCV and the reporting of results[35], and issued an update in 2013 due to (1) changes in the availability of certain commercial HCV antibody tests; (2) evidence that many persons identified as reactive by an HCV antibody test might not subsequently be evaluated to determine if they have current HCV infection[36]; and (3) significant advances in the development of antiviral agents with improved efficacy against HCV[37].
A rapid test for HCV antibodies should firstly be used. Anti-HCV assays to detect antibodies to HCV Encoded Antigen, include Abbott PRISM HCV (Abbott, 2006)[38] and the Ortho HCV Version 3.0 ELISA Test System (Ortho-Clinical, 2009)[39].
In 2011, the United States Food and Drug Administration (FDA) approved the OraQuick® HCV Rapid Antibody platform using finger prick capillary blood and venipuncture whole blood, which enables healthcare providers to deliver an accurate diagnosis in 20 min[40]. The FDA also approved the waived test permitting use of the assay in untraditional settings such as physicians’ offices, hospital emergency departments, health department clinics, and other independent counseling and testing sites[41].
In a next step, all positive HCV screening serologic tests require confirmation by HCV RNA detection. FDA-approved HCV nucleic acid tests (HCV NAT) for detection of HCV RNA should be used for testing individual samples or pooled samples of blood from at-risk patients who test reactive for HCV antibodies. Qualitative and quantitative HCV NAT assays include the UltraQual HCV RT-PCR Assay (2001)[42], the COBAS AmpliScreen HCV Test, v. 2.0 (2002)[43], the HCV RT PCR Assay (2007)[44], and the Multiplex Assay COBAS TaqScreen MPX Test (2008)[45].
Other FDA recommendations include supplementary testing for HCV antibodies. If testing is desired to distinguish between true and false positivity for HCV antibodies, anti-HCV monitoring may be performed with a second HCV antibody assay, approved by the FDA for diagnosis of HCV infection, which is different from the assay used for the initial antibody testing. HCV antibody assays vary according to their antigens, test platforms, and performance characteristics, so biological false positivity is unlikely to be exhibited by more than one test when multiple tests are applied to a single specimen[46].
A specific and sensitive method for the quantification of HCV core antigen using an ELISA screening method has been reported[47,48]. However, while ELISA is less expensive than an HCV RNA test, its limitations mean that alternative methods with lower detection limits, higher sensitivity and selectivity, and faster responses need to be developed[49].
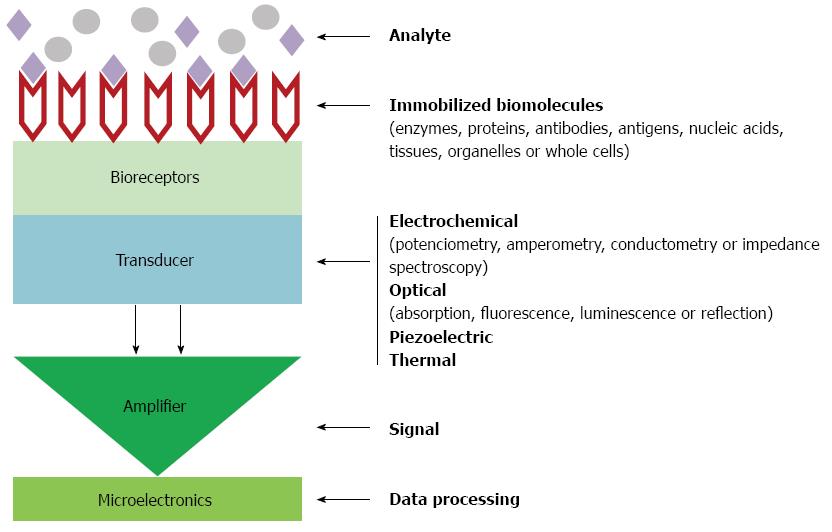
To this end, biosensor technology has the potential to provide fast and accurate anti-HCV and HCV RNA detection. According to IUPAC, a biosensor is a device that uses specific biochemical reactions mediated by isolated enzymes, immunosystems, tissues, organelles, or whole cells to detect chemical compounds, usually by means of electrical, thermal, or optical signals[50]. Figure 2 shows a schematic diagram of biosensor devices. The biological recognition element immobilized on bioreceptor surface interacts to analyte; the tranducer converts the recognition event into a measurable signal; finally, the output from the transducer is amplified, processed and displayed. The intensity of signal can be proportional to the analyte concentrations.
In the present review, the focus will be on the most recent developments in the technology of electrochemical immunosensors and DNA biosensors or genosensors for use in HCV studies, including information on applications and future prospects for HCV diagnostics.
Immunosensors are solid-state affinity ligand-based biosensing devices that couple immunochemical reactions to appropriate transducers. Generally, an immunosensor consists of a sensing element and a transducer. The sensing element is formed by means of the immobilization of antigens or antibodies, and the binding event is transformed into a measurable signal by the transducer[51]. The merits of immunosensors are obviously related to the selectivity and affinity of the antibody-analyte binding reaction. These devices are responsible for the transformation of specific antibody-antigen (Ab-Ag) interactions into measurable piezoelectric[52], acoustic[53], electrochemical[21,54-56], magnetic[57], or optical signals[58,59], and have been extensively studied for clinical diagnosis[60].
In recent years, great progress in nanoscience and nanotechnology has opened new opportunities for assembling electrochemical immunosensors. Various nanomaterials have been utilized for the fabrication of electrochemical immunosensors, including colloidal gold/silver, semiconductors, carbon or silica nanoparticles, and magnetic beads[61]. Among these nanomaterials, novel carbon nanostructures such as carbon nanotubes (CNT), carbon nanofibers (CNF), and carbon nanorods (CNR) are popular as the support materials for electrochemical immunosensors, due to their electrical conductivity, large surface area, good chemical stability, and excellent biocompatibility[62-67]. Carbon materials have been extensively used as immobilized substrates for the fabrication of biosensors, because of their attractive mechanical, electronic, and chemical properties[68]. Several researchers have focused on the ability of surface-confined CNTs to promote electron-transfer reactions in biosensing devices[69,70]. CNTs can also be coated with high loads of enzymes and secondary antibodies for signal amplification in sandwich immunoassays[71]. The superior physical and chemical properties of graphitized mesoporous carbons (GMCs), including high specific surface area, good electrical conductivity, excellent chemical stability, and large pore volumes, indicate their potential for application in electrochemical biosensors[72]. The immunosensor formats used for monitoring viral infections include sandwich-type and competitive-type assays. In a competitive format, unlabeled analyte (usually the antigen) in the test sample is measured by its ability to compete with the labeled antigen in the immunoassay. Typically, the detectable signal decreases with the increase of analyte concentration, due to the effect of the background signal[73]. Furthermore, depending on the immunoassay format used, these tests can be either direct (where the immunochemical reaction is directly determined by measuring the physical changes induced by the formation of the complex) or indirect (where a sensitively detectable label is combined with the antibody or antigen of interest)[74]. The distinction has an entirely different meaning to the use of the terms direct and indirect in the immunoassay field, where both are tracer-related. They are distinguished according to whether the antibody binding is directly detected (for example, after an enzyme-labeled antibody is bound to an immobilized coating conjugate, or an enzyme tracer is bound to an immobilized antibody), or whether the detection only takes place after a secondary binding reaction (such as when an enzyme-labeled secondary antibody is used to label a first antibody bound to an immobilized coating conjugate)[75,76].
In contrast, non-competitive immunoassay formats (usually the sandwich-type formats) provide the highest levels of sensitivity and specificity, due to the use of a pair of matched antibodies[77].
For the indirect assay modes, this significantly facilitates the problem of signal generation. The tracer labels either the occupied binding sites of the antibodies or the free sites. As for the sandwich-type immunosensors, the primary antibodies are usually immobilized on a solid-state support, and the sandwiched immunocomplex is formed between the immobilized primary antibodies and signal antibodies (usually enzyme-labeled antibodies or nanoparticle-labeled antibodies). The detectable signal mainly derives from the labeled signal tags. In spite of many advances in this field, there is still a paucity of novel approaches for improving the simplicity, selectivity, and sensitivity of clinical immunoassays, in order to respond to the demands and needs of modern medical diagnostics and biomedical research applications. In this regard, the protein-mediated assembly of nanoparticles is a potential tool for the fabrication of new sandwich-type immunosensors. This approach combines tunable nanoparticle features (size, surface functionality, and core properties) with the unique physical and chemical properties of proteins and peptides.
The measurement of the labeled analyte (usually the antibody) is directly proportional to the amount of antigen present in the sample, so the detectable signal increases with increasing amounts of the target analyte[78]. The sandwich-type assay is therefore one of the most popular schemes used in immunosensing and immunoassays. Although the antigen-antibody reaction can cause the detectable signal to change to some extent, the change is comparatively small. High-affinity antibodies and appropriate labels are usually employed for the amplification of the detectable signal[79].
Typical methods involve the use of an indicator system (such as an enzyme label) that results in the amplification of the measured product[80]. Since, for steric reasons, there is usually a 1:1 ratio of enzyme and signal antibody used in the traditional enzyme immunoassays, the detectable signal is always limited[81]. The rapidly emerging research field of nanoparticle labels, and the processes used to generate, manipulate, and deploy nanomaterials, provides exciting new possibilities for the advanced development of new analytical tools and instrumentation. One major advantage of using nanoparticle labels lies in the ability to control and tailor their properties to meet the needs of specific applications. Compared to the bulk materials, the nanomaterials offer unique chemical and physical properties, such as high surface-to-volume ratios and unique conductivities and optical properties[82], and can provide good biocompatibility.
Various nanoparticle labels including noble metal nanoparticles, carbon nanomaterials, semiconductor nanoparticles, metal oxide nanostructures, and hybrid nanostructures have been developed for use in the sandwich-type immunosensors and immunoassays[21]. Antibodies (antigens) labeled with nanoparticles can retain their bioactivity and interact with their counterparts, and the amount or concentration of an analyte can be determined, based on the detection of the nanoparticles[83]. The enormous signal enhancement associated with the use of nanomaterial amplifying labels and with the formation of nanoparticle-antibody-antigen assemblies provides the basis for ultrasensitive immunosensing and immunoassays[28,84]. When one antibody on the nanoparticle reacts with the corresponding antigen, other biomolecules labeled on the nanoparticle will be carried over, and thus participate in the reaction. Therefore, the high amount immobilized with the antibodies can increase the possibility of antigen-antibody reaction, while the enzymes can enhance the sensitivity by amplification of the detectable signal.
Several studies have revealed significant correlations between HCV core antigen levels and HCV RNA levels in untreated patients with high viral loads[28].
There are various methods that can be used to detect HCV core antigen[24,85,86]. The advantages of excellent sensitivity, rapid response, and cost-effectiveness of the nanostructured metal oxides make them the preferred choice for the fabrication of biosensors[87-89].
Electrochemical immunosensors, based on the highly specific molecular recognition of an antigen by its antibodies, have attracted a high level of interest in clinical diagnostics, and will be expected to provide fast and highly sensitive detection of HCV core antigen[55]. However, to the best of our knowledge, there are few reports concerning the use of electrochemical immunosensors for detection of HCV core antigen. It is valuable to explore the possibility of using electrochemical immunosensors to detect HCV core antigens in clinical applications. Table 1 indicates recent developments in HCV detection using electrochemical immunosensors.
| Electrode | Immunosensor format | Antigen | Labelled system | Technique | Performance of the immunosensor | Ref. |
| 3-Mercaptopropionic, acid was assembled on gold electrode to form a self-assembled monolayer | - | Thionine HCV horseradish peroxidase (HRP) antibody | - | Cyclic voltammetry and Linear scan voltammetry | The linearity of Hepatitis C in the range of 3.2 to 16 mg/L with the correlation coefficient of 0.995 | [90] |
| Glassy carbon electrode modified with a nanocomposite (gold/zirconia/chitosan) | Sandwich-type | HCV core | Label-free | Cyclic voltammetry, Electrochemical impedance spectroscopy | Stability: 98.5% (30 d) | [91] |
| Detection limit: 0.17 ng/mLRSD (different electrodes): 5.1%, 3.9% and 4.8% for 2, 32 and 128 ng/mL HCV core antigen | ||||||
| GMCs-MB nanocomposite | Sandwich-type | HCV core | Horseradish peroxidase-DNA-coated CMWNTs as a secondary antibody layer | Cyclic voltammetry, Electrochemical impedance spectroscopy | Stability: 91.6% (10 d) | [92] |
| Detection limit: 0.01 pg/mL | ||||||
| Regeneration: 8 mol/L urea solution (RSD, 3.1%) | ||||||
| Glassy carbon electrode was modified with an Au-MoO3/Chitosan nanocomposite | Sandwich-type | HCV non-structural 5A protein | Horseradish peroxidase-labelled antibody | Cyclic voltammetry, Chronoamperometry, Electrochemical impedance spectroscopy | Detection range: 1.0 ng/mL-50 μg/mL | [93] |
| Silk fibroin nanostructured films on screen-printed carbono electrode | Direct assay | HCV non-structural 5A protein | Label-free | Cyclic voltammetry | Sensitivity: 28 μA/μgDetection range: 0 μg/mL-0.2 μg/mL | [94] |
Li et al[90] (2005) reported an electrochemical immunosensor for clinical application, with detection of HCV in human serum. Cyclic voltammetry and linear scanning voltammetry were used to investigate the chemical characteristics of the immunosensor. Linear scanning voltammetry provided linearity for hepatitis C in the range 3.2-16 mg/L, and a correlation coefficient of 0.995. This method was in good agreement with the enzyme-linked immunosorbent assay.
Ma et al[91] (2012) reported a label-free electrochemical immunosensor for detecting the core antigen of the HCV. A glassy carbon electrode was modified with a nanocomposite made from gold nanoparticles, zirconia nanoparticles, and chitosan. A sandwich-type immunosensor was developed that displayed high sensitivity to the HCV core antigen in the concentration range 2-512 ng/mL, with a detection limit of 0.17 ng/mL (at S/N = 3). Under optimized conditions, this immunosensor exhibited a wide linear range, good stability, and high sensitivity for the detection of HCV core antigen. The assay was convenient and cost-effective, and had promising potential for the early clinical diagnosis of HCV infection. This immunosensor provides an alternative approach towards the diagnosis of HCV.
In 2013, an ultrasensitive and selective electrochemical immunosensor was developed for the detection of HCV core antigen. The immunosensor consists of an electrode modified with graphitized mesoporous carbon-methylene blue (GMC-MB) nanocomposite, with horseradish peroxidase-DNA-coated carboxyl multi-wall carbon nanotubes (CMWNTs) as a secondary antibody layer. After modification of the electrode with the GMC-MB nanocomposite, Au nanoparticles were electrodeposited onto the electrode to immobilize the captured antibodies. The bridging probe and secondary antibodies linked to the CMWNTs, together with DNA concatemers, were obtained by hybridization of the biotin-tagged signal and auxiliary probes. Finally, streptavidin-horseradish peroxidases (HRP) were labeled on the secondary antibody layer by means of a biotin-streptavidin system. The MB reduction current was generated in the presence of hydrogen peroxide, and was monitored by square wave voltammetry. Under optimum conditions, the amperometric signal increased linearly with the core antigen concentration (in the range 0.25-300 pg/mL). The immunosensor had a detection limit of as low as 0.01 pg/mL, and showed high selectivity. The new protocol presented acceptable stability and reproducibility, as well as favorable recovery for HCV core antigen in human serum. The proposed immunosensor has considerable potential for use in clinical applications, and provides a promising universal multi-sHRP-DNA-CMWNTs label for different analytes[92].
A novel electrochemical immunosensor was prepared for the detection of the non-structural 5A protein of HCV. A glassy carbon electrode was modified with an Au-MoO3/chitosan nanocomposite that exhibited good conductivity and biocompatibility. Mesoporous silica with a large specific surface served as a nanocarrier for horseradish peroxidase and the polyclonal antibody as the reporter probe. The immunosensor was characterized by scanning electron microscopy, electrochemical impedance spectroscopy, and cyclic voltammetry. Following the sandwich-type immunoreaction, horseradish peroxidase was efficiently captured on the surface of the electrode to catalyze the decomposition of hydrogen peroxide. The analytical signal was obtained as an amperometric i-t curve (chronoamperometry). The reported assay had a wide concentration range (between 1 ng/mL and 50 μg/mL) and a low detection limit of 1 ng/mL for the HCV non-structural 5A protein. The results demonstrated excellent reproducibility, high selectivity, and outstanding stability for determination of the HCV non-structural 5A protein, and the technique was successfully applied for detection of the analyte in real serum samples. A one-step modification procedure with Au-MoO3/chitosan nanoparticles was introduced to avoid cumulative error in multistep modification, and an RSD of 4.5% was obtained. Benefits of the biosensor included a short analysis time, a low limit of detection, high selectivity, and excellent stability for the determination of HCV NS5A, and the technique was successfully used to detect HCV in real samples[93].
Moraes et al[94] (2013) demonstrated the feasibility of immunosensors based on nanostructured silk fibroin (SF) films prepared by the layer-by-layer technique. The antigenic NS5A-1 peptide, derived from the HCV NS5A protein, was immobilized into the films in order to prepare a highly specific immunosensor. UV-Vis absorption measurements indicated that the peptide was proportionally adsorbed onto SF in each bilayer deposited. Fluorescence and circular dichroism (CD) spectra indicated that the SF/peptide film interaction induced secondary structure in NS5A-1. This amperometric sensor (SF/NS5A-1) proved to be highly sensitive when the composite film was tested in the presence of anti-HCV. The peptide/silk fibroin interaction can provide new architectures of immunosensors based on antigenic peptide and SF as an immobilization matrix. The immunosensor described was able to detect the antibody using a dilution range from 1:100 to 1:10000, with a sensitivity of 28 μA/μg per milliliter. The sensitivity of the device was determined from the slope of the curve of the linear response plotted against the anti-HVC concentration in the range 0-0.2 μg/mL (0 to 1:500).
Immunosensor formats for hepatitis viruses have employed both piezoelectric[95,96] and surface plasmon resonance-based transducers[97]. Alternatively, cell-based assays have been considered for HCV detection, using interaction of the virus with hepatocytes immobilized in a reactor coupled to electroimpedance monitoring[98], and specific detection of viral protease in mammalian cells using green fluorescent protein as reporter molecule has been described[99]. However, the immunochemical assays cannot discriminate between current and previous exposures, and in the case of acute infection, the antibodies might not be present[100]. For these reasons, the detection of HCV RNA using the polymerase chain reaction (PCR) is a valuable alternative assay[101,102]. The oligonucleotide probes suitable for capture of target sequences were investigated using BIAcore[103-105].
The DNA molecule has structural features that allow its immobilization on electrode surfaces as single (ss-DNA) or double (ds-DNA) helices[106,107], to produce electrochemical biosensors or genosensors[108-110]. Genosensors are an alternative for the determination of a range of analytes in different samples in order to evaluate damage and/or protection of the DNA molecule, and are suitable tools for the analysis and determination of DNA in order to diagnose diseases.
DNA hybridization technology has been applied in biosensor systems, particularly for diagnostic tests, and offers lower cost, speed, and simplicity of execution. In the hybridization process, the electrode is modified by immobilizing the ss-DNA probe, which identifies the complementary DNA strands and forms a double-stranded hybrid. This identification is effective and specific in the presence of other non-complementary sequences[110,111]. HCV is a single-stranded RNA virus, so the RNA should first be isolated from the serum of the patient, after which complementary DNA (cDNA) is produced by transcriptase reaction, and finally the DNA can be amplified by the PCR.
Although a variety of techniques can be employed to monitor HCV DNA hybridization, in this review the focus is on electrochemical biosensors. Various electrodic materials can be modified with DNA, including gold[112,113], graphite[114], carbon paste[115], and boron doped diamond[116]. There are many ways in which nucleic acids can be immobilized onto electrodes, including covalent attachment, affinity, self-assembled monolayers (SAM), adsorption, and electrochemical adsorption[109,117].
Hybridization detection can be performed directly or indirectly[118,119]. Direct detection (or label-free detection) involves the measurement of changes in electrochemical signals related to the electroactivity of DNA bases, most commonly from oxidation of guanine or adenine moieties in DNA strands. Charge transfer resistance measured using electrochemical impedance spectroscopy (EIS)[120] is also direct detection, while indirect detection can be based on the incorporation of electroactive indicators, using a DNA sequence previously labeled with a redox-active enzyme or nanoparticles[121]. Indirect DNA hybridization detection can be performed using electrochemical techniques such as amperometry, differential pulse voltammetry (DPV), square wave voltammetry (SWV), and cyclic voltammetry (CV)[122], except when monitoring using guanine or adenine.
A selective and sensitive label-free DNA hybridization electrochemical method for detection of HCV was proposed by dos Santos Riccardi et al[123]. Specific sequence HCV type-1 DNA probes were immobilized on polypyrrole films deposited on Pt microelectrodes. The monitoring of the hybridization with the complementary DNA was based on electrostatic modulation of the ion-exchange kinetics of the polypyrrole film, and allowed the detection of HCV-1 with a limit of detection (LOD) of 1.82 × 10-21 mol/L. With this biosensor, HCV-1 DNA detection did not show unspecific interactions in the presence of mismatched sequences from different HCV genotypes, such as 2a/c, 2b, and 3.
Alteration in the guanine oxidation signal after duplex formation between the probe and target DNA was used for DNA hybridization detection in the work developed by Pournaghi-Azar et al[124]. A 20-mer oligonucleotide called PHCV1, complementary to the universal sequence of the HCV1a core protein gene, was used as the probe, and its complementary oligonucleotide (HCV1a), corresponding to the consensus sequence of the HCV1 core protein gene, was used as the target DNA. After optimization of probe immobilization and hybridization conditions, the selectivity of the biosensor was studied using non-complementary oligonucleotides. The biosensor presented a LOD of 6.5 nmol/L, which, according to the authors, was comparable with other label-free (guanine-based) electrochemical hybridization detection methods.
The use of disposable electrodes in the construction of DNA biosensors can be advantageous, since these electrodes have low construction cost, good reproducibility of the area, the possibility of large-scale production, and the absence of surface inactivation. Different disposable electrodes have been used, including pencil graphite electrodes (PGE) and recordable gold CD-Rs.
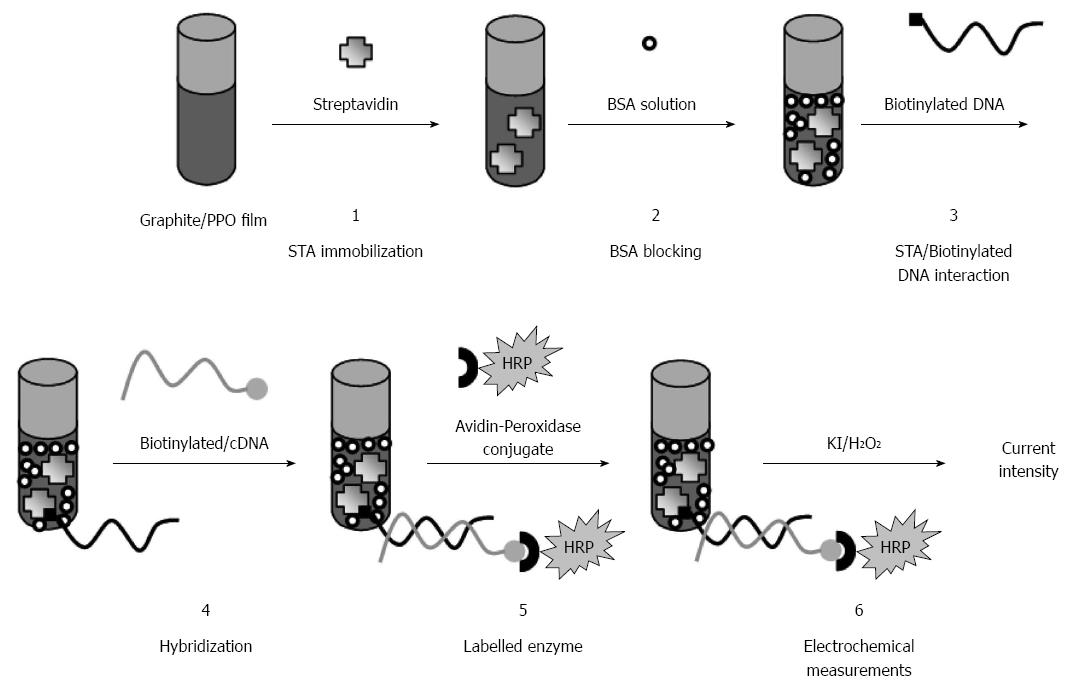
Riccardi Cdos et al[125] developed a disposable HCV genosensor with thin film siloxane-poly(propylene oxide) hybrids prepared by the sol-gel method and deposited onto a PGE surface by dip-coating (Figure 3). The recognition probe immobilization was based on the streptavidin (STA)/biotin attachment, since strong interaction occurs between avidin (or streptavidin) and biotin. The STA was encapsulated in the films, and biotinylated 18-mer DNA probes for HCV (genotypes 1, 2a/c, 2b, and 3) were immobilized by means of STA. The complementary DNA was hybridized to the immobilized target-specific oligonucleotide probe, followed by avidin-peroxidase labeling. Using the amperometric technique, the hybridization event was detected by monitoring the enzymatic response at -0.45V vs Ag|AgCl, using H2O2 as enzyme substrate and KI as electron mediator. Negative and positive controls were analyzed, together with positive samples of sera from patients, and the HCV 1, 2a/c, 2b, and 3 oligonucleotide probes immobilized on PGE were able to distinguish between positive and negative serum samples.
Genosensor development requires that several parameters be optimized, such as the type of immobilization, concentration of immobilized biomolecules, amongst others, which leads to an increase in the number of experiments required. The application of statistical tools is therefore very important in order to be able to explore and analyze the extensive range of data obtained for a system. Chemometric studies were employed for the development of another biosensor for HCV using PGE[126]. The main steps of the methodology were the immobilization of STA on a sol-gel film deposited on the PGE surface, followed by interaction with biotinylated DNA probes specific for HCV. The hybridization reaction occurred when the electrode was placed in contact with biotinylated complementary DNA, and avidin-peroxidase labeling was performed to indirectly detect the HCV. Electrochemical measurements of the enzymatic activity were performed using H2O2 and 5-aminosalicylic acid as substrate and electron mediator, respectively. Fractional factorial and factorial with center point designs were applied in order to simultaneously evaluate the variables of interest that had a significant influence on the biosensor response. MINITAB software was used to generate level combinations for all factors used in the assays. This strategy had several advantages, such as a reduced number of experimental runs, more information, and optimization of the experimental conditions in terms of the biosensor response. It was possible to obtain optimized concentrations and incubation times for all the biomolecules tested.
Also applying chemometric experiments for the optimization of many parameters, gold electrodes built using a recordable compact disc (CDtrodes) were used for the construction of a disposable genosensor for HCV[113]. The variables evaluated were the degree of dilution and incubation time of DNA probes for HCV-1, dilution and incubation time of complementary DNA, and concentration and incubation time of conjugate avidin-peroxidase, which was the label for hybridization. The enzymatic response was measured by constant potential amperometry, at -0.05 V vs Ag|AgCl(KClsat). After optimization of all the parameters for biomolecule immobilization, the amperometric genosensor was employed for HCV-1 DNA detection in HCV-infected patients previously submitted to the standard qualitative Amplicor HCV test. The results showed that the current intensities for the positive samples were higher than for the negative samples. The factorial design procedure enabled the identification of critical parameters, while knowledge of the chemistry involved enabled further refinement of the technique, where necessary. Full and fractional factorial design methods were employed for the optimization of a biosensor for hepatitis C diagnosis, and could be extended to other types of DNA-based biosensors.
A versatile electronic detection platform based on disposable DNA chips was described by Umek et al[127], who fabricated an electrode array containing capture probes specific for sequences in the HCV on separate electrodes. Printed circuit board technology was used to manufacture chips with 14 exposed gold electrodes, each of which was wired to a connector at the chip edge. The gold electrodes were coated with a self-assembled monolayer containing DNA capture probes. Unlabeled nucleic acid targets were immobilized on the surface of the SAM by sequence-specific hybridization with the DNA capture probe. A separate signaling probe, containing ferrocene-modified nucleotides and complementary to the target in the region adjoining the capture probe binding site, was held in close proximity to the SAM in a sandwich complex. Since ferrocene is a redox-active metal compound, when a given potential is applied to the electrode, electron transfer occurs between the ferrocene and the electrodic surface. The authors demonstrated that the versatility of this electronic detection platform made it suitable for multiple applications in diagnostics and pharmacogenetics.
Instead of employing enzymes as a label for hybridization, Liu et al[128] reported the cleavage capacity of an endonuclease enzyme in the DNA analysis. The authors developed an approach for qualitative and quantitative HCV detection based on site-specific DNA cleavage of BamHI endonuclease, an enzyme derived from Bacillus amyloliquefaciens. The enzyme recognizes the palindromic sequence 5’ GGATCC-3’ and cleaves after the first nucleotide, leaving four-base 5’ overhangs[129]. The thionine-labeled probe DNA was self-assembled on the surface of a gold electrode and hybridized with target cDNA, which is a 21-mer oligonucleotide related to HCV. The detection was based on variation of the electrochemical signal of thionine[23] or ferroceneacetic acid (FcA)[25], measured by cyclic voltammetry before and after digestion with BamHI endonuclease. BamHI recognizes the duplex symmetrical sequence 5’-GGATCC-3’ and catalyzes double-stranded cleavage between the guanines in the presence of Mg2+. After the hybridization with complementary DNA, the cyclic voltammogram showed a pair of redox peaks corresponding to the thionine process. After hybridization, the electrode was immersed in a solution containing BamHI, the dsDNA was cleaved at a specific site (5’-G/GATCC-3’), and the thionine was removed from the electrode surface. Therefore, no thionine redox peak was observed, and the DNA-BamHI endonuclease interaction model could be used for qualitative HCV detection. The developed method was used to detect HCV in serum samples from patients. The results demonstrated that the samples characterized as positive using the standard qualitative Amplicor HCV test were able to hybridize with the probe on the electrode, with the voltammetric signal of thionine decreasing significantly after cleavage by BamHI, while those samples appearing as negative in the Amplicor assay were unable to hybridize, so that the thionine response remained almost unchanged after cleavage by BamHI. The major advantages of this enzymatic cleavage assay were its good specificity, ease of use, and the ability to perform real-time monitoring. Gold nanoparticles (AuNPs) amplified the signal of the electroactive label molecule (thionine)[130].
Peptide nucleic acid (PNA) is an extremely good structural mimic of DNA (or RNA), capable of forming Watson-Crick base pair-dependent double helices with DNA or RNA complementary sequences[131]. Its structure is simple, consisting of repeating N-(2-aminoethyl)-glycine units linked by amide bonds. The purine (A, G) and pyrimidine (C, T) bases are attached to the backbone through methylene carbonyl linkages[132]. Unlike DNA or DNA analogs, PNAs do not contain any (pentose) sugar moieties or phosphate groups. An interesting property of PNA is that the neutral backbone also increases the rate of hybridization significantly in assays where either the target or the probe is immobilized[133].
Detection of the DNA sequence related to the HCV genotype 3a (pHCV3a) core/E1 region was performed by the group of Dr Pournaghi-Azar using PNA[134-137]. In the first work[134], the PNA probe was covalently attached on a gold electrode, followed by hybridization with a complementary DNA. The hybridization was detected by accumulating methylene blue (MB) as an electroactive indicator, and the reduction signal of the accumulated MB was measured by using DP voltammetry. A significant increase in the MB signal was observed after hybridization with complementary oligonucleotide. Increase in the peak current was attributed to hybridization of the PNA probe with the ds-DNA, resulting in PNA/ds-DNA formation, with which more MB molecules interacted. On the other hand, non-complementary oligonucleotide showed no significant interaction with PNA, since the MB signal was low. The results suggested that the DNA sensor responded selectively to the target. The biosensor presented a LOD of 5.7 × 10-11 mol/L, was highly reproducible, and with regeneration could be used seven times for detection of the target DNA. The authors[137] also developed a biosensor based on direct detection of the target DNA sequence in recombinant plasmid without denaturation of ds-DNA. The detection principle was based on hybridization between the PNA, immobilized on a gold disk electrode, and the target double-stranded plasmid. The sequence corresponded to a consensus sequence in the core/E1 region of the HCV genome, and was used as a universal segment for detection of all HCV genotypes. Plasmid molecules were used as double-stranded structures (ds-pl) for hybridization without denaturation, with the target having a length of 4568 bp and containing core/E1 encoding cDNA. A non-complementary plasmid was also used. Detection of the hybridization was accomplished by monitoring the difference between the DP voltammetric response of methylene blue accumulated on the PNA, before and after hybridization with complementary ds-pl. After optimization of the parameters, including treatment with RNase A enzyme, washing time, and washing temperature, interaction between PNA and the complementary plasmid resulted in a considerable increase in the MB reduction signal, while the non-complementary plasmid did not lead to any significant increase of the signal, due to the absence of significant hybridization between the probe and non-complementary ds-pl. In this method, the ds-DNA denaturation step was not necessary, which was adequate for the detection of target DNA in real samples.
Instead of using DNA or PNA, Park et al[133] used ribonucleic acid (RNA) oligomer of the internal ribosome entry site sequence specific to the HCV as a target for a biosensor based on hybridization with the PNA molecule. The HCV genome composed of 9600 bases contains untranslated regions (UTR) at both ends, which play important roles in translation and transcription. In the 5′ UTR, there is an internal ribosome entry site (IRES) sequence, which is one of the most conservative regions in the whole HCV genome. Therefore, it is not transformed during its mutation, and can be considered a suitable target for HCV analysis. A gold electrode was modified by the SAM of 3-thiophene-acetamide-diaza-18-crown-6 (TADC) to hold amine-terminated PNA. The nonspecifically bound PNA molecules were removed by displacing them via the formation of 3-mercaptopropionic acid (MPA), and finally the electrode modified with PNA and MPA was dipped into the target RNA solution. RNA detection was conducted by Fourier transform electrochemical impedance spectroscopy (FT-EIS) in the presence of the Fe(CN)63-/4- redox probe. The ratio of charge-transfer resistance before and after hybridization showed a linear increase with log[CRNA], and the LOD was approximately 23 pmol/L.
In most genosensors, the function of electrochemically active compounds is only to act as indicators. The electrochemical indicators have different binding affinities towards ss-DNA and ds-DNA, and show different response signals. In recent work, Zhang et al[138] selected the [Co(phen)2(L-Cys)] metal complex, used as an indicator in DNA biosensors, to act as an indicator as well as to play a role in immobilization of probe DNA, which simplified the construction procedure. The gold electrode was modified by firstly immersing it in saturated L-Cys methanol solution, followed by dropping [Co(phen)2Cl2]Cl dimethyl sulfoxide onto the L-Cys-modified electrode surface to produce [Co(phen)2(L-Cys)]. The DNA probe was immobilized by dropping the solution onto the modified electrode. Hybridization was carried out using a specific oligonucleotide sequence of HCV subtype 1b. The results obtained by square wave voltammetry indicated that the current intensity of the probe decreased sharply when it hybridized with complementary DNA, while one-base mismatch of the target DNA caused a very different response signal, and no hybridization signal was found for the non-complementary DNA. The sensor showed a response for detection of the specific oligonucleotide sequence that was linear to the logarithm of the concentration in the range 1.0 pmol/L to 1.0 μmol/L. According to the authors, the design concept is workable and [Co(phen)2(L-Cys)] can play the dual roles of electrochemical indicator and anchor for probe DNA immobilization during construction of the sensor.
A commercial electrochemical sensor, called eSensor® HCV Genotyping Test[138], was designed for the typing and subtyping of HCV 1a, 1b, 2a/c, 2b, 3, 4, 5, and 6a/b. In the device, the target DNA is mixed with the signal probe solution in the cartridge, and is analyzed using electrochemical detection. DNA from a positive sample is amplified by PCR using specific primers. The amplified DNA is converted to single stranded DNA by exonuclease digestion, and then combined with a signal buffer containing ferrocene-labeled signal probes that are specific for the different subtypes. The mixture of amplified sample and signal buffer is loaded onto a cartridge containing single-stranded oligonucleotide capture probes bound to gold-plated electrodes. The cartridge is inserted into the XT-8 instrument, where the single-stranded targets first hybridize to the perfect match signal probe and then hybridize to the complementary sequences of the capture probe. The presence of each target is determined by voltammetry, which generates specific electric signals from the ferrocene-labeled signal probe. This novel technology was validated by Sam et al[139]. The amplicon from the commercial kit served as a template for nested PCR, followed by a direct analysis on the electrochemical eSensor® XT-8 detection system for the identification of HCV genotypes. The assay was validated for limit of detection, which was below 175 IU/mL for all the subtypes except 6ab, as well as specificity, accuracy, and precision. The authors reported high performance characteristics, which should facilitate viral genotyping for personalization of dose and duration of treatment. The high sensitivity, good intra- and inter-assay precision, and agreement with a validated method make this assay particularly well suited for clinical HCV genotyping to guide antiviral therapy.
Studies of electrochemical immunosensors and genosensors for hepatitis C virus have demonstrated the potential usefulness of these approaches in public health applications. The methodology for immobilization of the antigen, ss-DNA, and PNA onto the electrode is similar, but the patient does not need to produce antibody immediately after the exposure. Very good sensitivity can be obtained with genosensors, but replication of c-DNA requires PCR technology. Nanotechnologies applied to biosensors have improved the methods for construction of these devices, with miniaturization increasing portability, accuracy, and reliability. An ideal electrochemical biosensor should be both integrated and highly automated in order to improve the efficiency of diagnostic testing. The global biosensor market is currently worth US $2.3 billion, and is expected to double in value over the next 5 years, with an annual growth rate in excess of 10% (http://unsw.technologypublisher.com/technology/3102). However, the main challenge is to obtain the results in a short period of time, at home or in the doctor’s office, using a point-of-care (POC) device that could be operated by non-laboratory personnel.
P- Reviewer: Camps J, Lei KF S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
| 1. | Idrees S, Ashfaq UA. Structural analysis and epitope prediction of HCV E1 protein isolated in Pakistan: an in-silico approach. Virol J. 2013;10:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Tang D, Tang J, Su B, Li Q, Chen G. Electrochemical detection of hepatitis C virus with signal amplification using BamHI endonuclease and horseradish peroxidase-encapsulated nanogold hollow spheres. Chem Commun (Camb). 2011;47:9477-9479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Center for Disease Control and Prevention. Hepatitis C Information for Health Professionals. Accessed in August 25, 2013. Available from: http://www.cdc.gov/hepatitis/hcv/hcvfaq.htm. |
| 4. | Averhoff FM, Glass N, Holtzman D. Global burden of hepatitis C: considerations for healthcare providers in the United States. Clin Infect Dis. 2012;55 Suppl 1:S10-S15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 215] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 5. | Torresi J, Johnson D, Wedemeyer H. Progress in the development of preventive and therapeutic vaccines for hepatitis C virus. J Hepatol. 2011;54:1273-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Castello G, Scala S, Palmieri G, Curley SA, Izzo F. HCV-related hepatocellular carcinoma: From chronic inflammation to cancer. Clin Immunol. 2010;134:237-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 112] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Schnuriger A, Dominguez S, Valantin MA, Tubiana R, Duvivier C, Ghosn J, Simon A, Katlama C, Thibault V. Early detection of hepatitis C virus infection by use of a new combined antigen-antibody detection assay: potential use for high-risk individuals. J Clin Microbiol. 2006;44:1561-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Ishiguro S, Inoue M, Tanaka Y, Mizokami M, Iwasaki M, Tsugane S; JPHC Study Group. Impact of viral load of hepatitis C on the incidence of hepatocellular carcinoma: A population-based cohort study (JPHC Study). Cancer Lett. 2011;300:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Chevaliez S, Pawlotsky JM. Hepatitis C virus serologic and virologic tests and clinical diagnosis of HCV-related liver disease. Int J Med Sci. 2006;3:35-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Kuo G, Choo QL, Alter HJ, Gitnick GL, Redeker AG, Purcell RH, Miyamura T, Dienstag JL, Alter MJ, Stevens CE. An assay for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitis. Science. 1989;244:362-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2495] [Cited by in RCA: 2342] [Article Influence: 65.1] [Reference Citation Analysis (0)] |
| 11. | Pawlotsky JM. Use and interpretation of virological tests for hepatitis C. Hepatology. 2002;36:S65-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Gray JJ, Wreghitt TG. Immunoglobulin G avidity in Epstein-Barr virus infection in organ transplant recipients. Serodiagn Immunother Infect Dis. 1989;3:389-393. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Gretch DR. Diagnostic tests for hepatitis C. Hepatology. 1997;26:43S-47S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 151] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Kao JH, Lai MY, Hwang YT, Yang PM, Chen PJ, Sheu JC, Wang TH, Hsu HC, Chen DS. Chronic hepatitis C without anti-hepatitis C antibodies by second-generation assay. A clinicopathologic study and demonstration of the usefulness of a third-generation assay. Dig Dis Sci. 1996;41:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Uyttendaele S, Claeys H, Mertens W, Verhaert H, Vermylen C. Evaluation of third-generation screening and confirmatory assays for HCV antibodies. Vox Sang. 1994;66:122-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Barrera JM, Francis B, Ercilla G, Nelles M, Achord D, Darner J, Lee SR. Improved detection of anti-HCV in post-transfusion hepatitis by a third-generation ELISA. Vox Sang. 1995;68:15-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 118] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Colin C, Lanoir D, Touzet S, Meyaud-Kraemer L, Bailly F, Trepo C. Sensitivity and specificity of third-generation hepatitis C virus antibody detection assays: an analysis of the literature. J Viral Hepat. 2001;8:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 150] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Alborino F, Burighel A, Tiller FW, van Helden J, Gabriel C, Raineri A, Catapano R, Stekel H. Multicenter evaluation of a fully automated third-generation anti-HCV antibody screening test with excellent sensitivity and specificity. Med Microbiol Immunol. 2011;200:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 19. | Ward KN, Dhaliwal W, Ashworth KL, Clutterbuck EJ, Teo CG. Measurement of antibody avidity for hepatitis C virus distinguishes primary antibody responses from passively acquired antibody. J Med Virol. 1994;43:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Kanno A, Kazuyama Y. Immunoglobulin G antibody avidity assay for serodiagnosis of hepatitis C virus infection. J Med Virol. 2002;68:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Pei X, Zhang B, Tang J, Liu B, Lai W, Tang D. Sandwich-type immunosensors and immunoassays exploiting nanostructure labels: A review. Anal Chim Acta. 2013;758:1-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 309] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 22. | Hofmann WP, Dries V, Herrmann E, Gärtner B, Zeuzem S, Sarrazin C. Comparison of transcription mediated amplification (TMA) and reverse transcription polymerase chain reaction (RT-PCR) for detection of hepatitis C virus RNA in liver tissue. J Clin Virol. 2005;32:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Bouvier-Alias M, Patel K, Dahari H, Beaucourt S, Larderie P, Blatt L, Hezode C, Picchio G, Dhumeaux D, Neumann AU. Clinical utility of total HCV core antigen quantification: a new indirect marker of HCV replication. Hepatology. 2002;36:211-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 157] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 24. | Gaudy C, Thevenas C, Tichet J, Mariotte N, Goudeau A, Dubois F. Usefulness of the hepatitis C virus core antigen assay for screening of a population undergoing routine medical checkup. J Clin Microbiol. 2005;43:1722-1726. [PubMed] |
| 25. | Zanetti AR, Romanò L, Brunetto M, Colombo M, Bellati G, Tackney C. Total HCV core antigen assay: a new marker of hepatitis C viremia for monitoring the progress of therapy. J Med Virol. 2003;70:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Tanaka N, Moriya K, Kiyosawa K, Koike K, Aoyama T. Hepatitis C virus core protein induces spontaneous and persistent activation of peroxisome proliferator-activated receptor alpha in transgenic mice: implications for HCV-associated hepatocarcinogenesis. Int J Cancer. 2008;122:124-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 27. | Krishnadas DK, Li W, Kumar R, Tyrrell DL, Agrawal B. HCV-core and NS3 antigens play disparate role in inducing regulatory or effector T cells in vivo: Implications for viral persistence or clearance. Vaccine. 2010;28:2104-2114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Park Y, Lee JH, Kim BS, Kim do Y, Han KH, Kim HS. New automated hepatitis C virus (HCV) core antigen assay as an alternative to real-time PCR for HCV RNA quantification. J Clin Microbiol. 2010;48:2253-2256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 29. | Moscato GA, Giannelli G, Grandi B, Pieri D, Marsi O, Guarducci I, Batini I, Altomare E, Antonaci S, Capria A. Quantitative determination of hepatitis C core antigen in therapy monitoring for chronic hepatitis C. Intervirology. 2011;54:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Laperche S, Le Marrec N, Girault A, Bouchardeau F, Servant-Delmas A, Maniez-Montreuil M, Gallian P, Levayer T, Morel P, Simon N. Simultaneous detection of hepatitis C virus (HCV) core antigen and anti-HCV antibodies improves the early detection of HCV infection. J Clin Microbiol. 2005;43:3877-3883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 31. | Leary TP, Gutierrez RA, Muerhoff AS, Birkenmeyer LG, Desai SM, Dawson GJ. A chemiluminescent, magnetic particle-based immunoassay for the detection of hepatitis C virus core antigen in human serum or plasma. J Med Virol. 2006;78:1436-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Widell A, Molnegren V, Pieksma F, Calmann M, Peterson J, Lee SR. Detection of hepatitis C core antigen in serum or plasma as a marker of hepatitis C viraemia in the serological window-phase. Transfus Med. 2002;12:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1998;47:1-39. [PubMed] |
| 34. | Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-365. [PubMed] |
| 35. | Alter MJ, Kuhnert WL, Finelli L; Centers for Disease Control and Prevention. Guidelines for laboratory testing and result reporting of antibody to hepatitis C virus. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52:1-13, 15; quiz CE1-4. [PubMed] |
| 36. | Centers for Disease Control and Prevention (CDC). Vital signs: evaluation of hepatitis C virus infection testing and reporting - eight U.S. sites, 2005-2011. MMWR Morb Mortal Wkly Rep. 2013;62:357-361. [PubMed] |
| 37. | Poordad F, Dieterich D. Treating hepatitis C: current standard of care and emerging direct-acting antiviral agents. J Viral Hepat. 2012;19:449-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 140] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 38. | Abbott Laboratories. Abbott Prism® HCV. Hepatitis C Virus Encoded Antigens (Recombinant c100-3, HCr43, NS5). Diagnostics Division. USA. 2006. Accessed in September 20, 2013. Available from: http://www.fda.gov/downloads/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/InfectiousDisease/UCM089367.pdf. |
| 39. | Ortho-Clinical Diagnostics, Inc.. Ortho HCV Version 3.0 ELISA. Hepatitis C Virus Encoded Antigen (HCV Encoded Antigen/Enzyme Immuno Assay (EIA), Version 3.0/Recombinant and Synthetic). Accessed in September 20, 2013. Available from: http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/InfectiousDisease/ucm176413.htm. |
| 40. | OraSure Technologies, Inc. OraQuick HCV: rapid antibody test. 2011. Accessed in September 20, 2013. Available from: http://www.orasure.com/products-infectious/products-infectious-oraquick-hcv.asp. |
| 41. | Shivkumar S, Peeling R, Jafari Y, Joseph L, Pant Pai N. Accuracy of rapid and point-of-care screening tests for hepatitis C: a systematic review and meta-analysis. Ann Intern Med. 2012;157:558-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 42. | National Genetics Institute. UltraQual HCV RT-PCR assay: hepatitis C virus reverse transcriptase polymerase chain reaction (PCR) assay. Accessed in September 20, 2013. Available from: http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/InfectiousDisease/ucm148187.htm. |
| 43. | Roche Molecular Systems, Inc.. COBAS AmpliScreen HCV Test, version 2.0.: hepatitis C virus (hepatitis C virus/polymerase chain reaction/blood cell derived). Accessed in September 20, 2013. Available from: http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/InfectiousDisease/ucm173197.htm. |
| 44. | BioLife Plasma Services, L.P.. Hepatitis C Virus (HCV) Reverse Transcription (RT) Polymerase Chain Reaction (PCR) Assay. Accessed in September 20, 2013. Available from: http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/InfectiousDisease/ucm148311.htm. |
| 45. | Roche Molecular Systems, Inc.. COBAS TaqScreen MPX Test. Accessed in September 20, 2013. Available from: http://www.fda.gov/ BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/BloodDonorScreening/InfectiousDisease/ucm176438.htm. |
| 46. | Vermeersch P, Van Ranst M, Lagrou K. Validation of a strategy for HCV antibody testing with two enzyme immunoassays in a routine clinical laboratory. J Clin Virol. 2008;42:394-398. [PubMed] |
| 47. | Aoyagi K, Ohue C, Iida K, Kimura T, Tanaka E, Kiyosawa K, Yagi S. Development of a simple and highly sensitive enzyme immunoassay for hepatitis C virus core antigen. J Clin Microbiol. 1999;37:1802-1808. [PubMed] |
| 48. | Ergünay K, Sener B, Alp A, Karakaya J, Hasçelik G. Utility of a commercial quantitative hepatitis C virus core antigen assay in a diagnostic laboratory setting. Diagn Microbiol Infect Dis. 2011;70:486-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 49. | Medici MC, Furlini G, Rodella A, Fuertes A, Monachetti A, Calderaro A, Galli S, Terlenghi L, Olivares M, Bagnarelli P. Hepatitis C virus core antigen: analytical performances, correlation with viremia and potential applications of a quantitative, automated immunoassay. J Clin Virol. 2011;51:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 50. | McNaught AD, Wilkinson A, editors . Compendium of Chemical Terminology. 2nd ed. The “Gold Book”. Oxford: IUPAC 2006; . [DOI] [Full Text] |
| 51. | Marco MP, Gee S, Hammock BD; Immunochemical techniques for environmental analysis II. Antibody production and immunoassay development. Trends Analyt Chem. 1995;14:341–350. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 52. | Jin X, Jin X, Chen L, Jiang J, Shen G, Yu R. Piezoelectric immunosensor with gold nanoparticles enhanced competitive immunoreaction technique for quantification of aflatoxin B1. Biosens Bioelectron. 2009;24:2580-2585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 53. | Krishnamoorthy S, Iliadis AA, Bei T, Chrousos GP. An interleukin-6 ZnO/SiO(2)/Si surface acoustic wave biosensor. Biosens Bioelectron. 2008;24:313-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 54. | Fu XH. Electrochemical immunoassay for carbohydrate antigen-125 based on polythionine and gold hollow microspheres modified glassy carbon electrodes. Electroanal. 2007;19:1831–1839. [RCA] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 55. | Tang D, Yuan R, Chai Y. Ultrasensitive electrochemical immunosensor for clinical immunoassay using thionine-doped magnetic gold nanospheres as labels and horseradish peroxidase as enhancer. Anal Chem. 2008;80:1582-1588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 285] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 56. | Tang D, Niessner R, Knopp D. Flow-injection electrochemical immunosensor for the detection of human IgG based on glucose oxidase-derivated biomimetic interface. Biosens Bioelectron. 2009;24:2125-2130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 57. | Mani V, Chikkaveeraiah BV, Patel V, Gutkind JS, Rusling JF. Ultrasensitive immunosensor for cancer biomarker proteins using gold nanoparticle film electrodes and multienzyme-particle amplification. ACS Nano. 2009;3:585-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 473] [Cited by in RCA: 369] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 58. | Fu Z, Hao C, Fei X, Ju H. Flow-injection chemiluminescent immunoassay for alpha-fetoprotein based on epoxysilane modified glass microbeads. J Immunol Methods. 2006;312:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 59. | Sánchez-Martínez ML, Aguilar-Caballos MP, Gómez-Hens A. Long-wavelength fluorescence polarization immunoassay: determination of amikacin on solid surface and gliadins in solution. Anal Chem. 2007;79:7424-7430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 60. | Watterson JM, Stallcup P, Escamilla D, Chernay P, Reyes A, Trevino SC. Evaluation of the Ortho-Clinical Diagnostics Vitros ECi Anti-HCV test: comparison with three other methods. J Clin Lab Anal. 2007;21:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 61. | Suni II. Impedance methods for electrochemical sensors using nanomaterials. TRAC- Trends Anal Chem. 2008;27:604-611. [RCA] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 207] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 62. | Viswanathan S, Rani C, Vijay Anand A, Ho JA. Disposable electrochemical immunosensor for carcinoembryonic antigen using ferrocene liposomes and MWCNT screen-printed electrode. Biosens Bioelectron. 2009;24:1984-1989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 107] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 63. | Wu L, Yan F, Ju H. An amperometric immunosensor for separation-free immunoassay of CA125 based on its covalent immobilization coupled with thionine on carbon nanofiber. J Immunol Methods. 2007;322:12-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 64. | Wang J, Lin Y. Functionalized carbon nanotubes and nanofibers for biosensing applications. Trends Analyt Chem. 2008;27:619-626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 247] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 65. | Cui R, Huang H, Yin Z, Gao D, Zhu JJ. Horseradish peroxidase-functionalized gold nanoparticle label for amplified immunoanalysis based on gold nanoparticles/carbon nanotubes hybrids modified biosensor. Biosens Bioelectron. 2008;23:1666-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 194] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 66. | Jie G, Zhang J, Wang D, Cheng C, Chen HY, Zhu JJ. Electrochemiluminescence immunosensor based on CdSe nanocomposites. Anal Chem. 2008;80:4033-4039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 196] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 67. | Chen X, Zhang K, Zhou J, Xuan J, Yan W, Jiang LP, Zhu JJ. Electrochemical immunosensor based on colloidal carbon sphere array. Biosens Bioelectron. 2010;25:1130-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 68. | Viswanathan S, Rani C, Ho JA. Electrochemical immunosensor for multiplexed detection of food-borne pathogens using nanocrystal bioconjugates and MWCNT screen-printed electrode. Talanta. 2012;94:315-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 69. | Maehashi K, Katsura T, Kerman K, Takamura Y, Matsumoto K, Tamiya E. Label-free protein biosensor based on aptamer-modified carbon nanotube field-effect transistors. Anal Chem. 2007;79:782-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 545] [Cited by in RCA: 374] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 70. | Luo XL, Xu JJ, Wang JL, Chen HY. Electrochemically deposited nanocomposite of chitosan and carbon nanotubes for biosensor application. Chem Commun (Camb). 2005;2169-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 71. | Wang J, Liu G, Jan MR. Ultrasensitive electrical biosensing of proteins and DNA: carbon-nanotube derived amplification of the recognition and transduction events. J Am Chem Soc. 2004;126:3010-3011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 406] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 72. | Neimark AV, Lin Y, Ravikovitch PI, Thommes M. Quenched solid density functional theory and pore size analysis of micro-mesoporous carbons. Carbon. 2009;47:1617-1628. [DOI] [Full Text] |
| 73. | Tang D, Zhong Z, Niessner R, Knopp D. Multifunctional magnetic bead-based electrochemical immunoassay for the detection of aflatoxin B1 in food. Analyst. 2009;134:1554-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 74. | Hock B. Antibodies for immunosensors: a review. Anal Chim Acta. 1997;347:177-186. [RCA] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 73] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 75. | D'Orazio P. Biosensors in clinical chemistry - 2011 update. Clin Chim Acta. 2011;412:1749-1761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 76. | Luppa PB, Sokoll LJ, Chan DW. Immunosensors--principles and applications to clinical chemistry. Clin Chim Acta. 2001;314:1-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 574] [Cited by in RCA: 374] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 77. | Quinton J, Kolodych S, Chaumonet M, Bevilacqua V, Nevers MC, Volland H, Gabillet S, Thuéry P, Créminon C, Taran F. Reaction discovery by using a sandwich immunoassay. Angew Chem Int Ed Engl. 2012;51:6144-6148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 78. | Tang D, Ren J. In situ amplified electrochemical immunoassay for carcinoembryonic antigen using horseradish peroxidase-encapsulated nanogold hollow microspheres as labels. Anal Chem. 2008;80:8064-8070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 163] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 79. | Li Q, Zeng L, Wang J, Tang D, Liu B, Chen G, Wei M. Magnetic mesoporous organic-inorganic NiCo2O4 hybrid nanomaterials for electrochemical immunosensors. ACS Appl Mater Interfaces. 2011;3:1366-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 80. | Su B, Tang D, Tang J, Cui Y, Chen G. Multiarmed star-like platinum nanowires with multienzyme assembly for direct electronic determination of carcinoembryoninc antigen in serum. Biosens Bioelectron. 2011;30:229-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 81. | Zhang B, Tang D, Liu B, Cui Y, Chen H, Chen G. Nanogold-functionalized magnetic beads with redox activity for sensitive electrochemical immunoassay of thyroid-stimulating hormone. Anal Chim Acta. 2012;711:17-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 82. | Tang J, Tang D, Niessner R, Knopp D, Chen G. Hierarchical dendritic gold microstructure-based aptasensor for ultrasensitive electrochemical detection of thrombin using functionalized mesoporous silica nanospheres as signal tags. Anal Chim Acta. 2012;720:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 83. | Brakmann S. DNA-based barcodes, nanoparticles, and nanostructures for the ultrasensitive detection and quantification of proteins. Angew Chem Int Ed Engl. 2004;43:5730-5734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 84. | Amaro M, Oaew S, Surareungchai W. Scano-magneto immunoassay based on carbon nanotubes/gold nanoparticles nanocomposite for Salmonella enterica serovar Typhimurium detection. Biosens Bioelectron. 2012;38:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 85. | Morota K, Fujinami R, Kinukawa H, Machida T, Ohno K, Saegusa H, Takeda K. A new sensitive and automated chemiluminescent microparticle immunoassay for quantitative determination of hepatitis C virus core antigen. J Virol Methods. 2009;157:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 86. | Lee S, Kim YS, Jo M, Jin M, Lee DK, Kim S. Chip-based detection of hepatitis C virus using RNA aptamers that specifically bind to HCV core antigen. Biochem Biophys Res Commun. 2007;358:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 87. | Lu L, Liu B, Li S, Zhang W, Xie G. Improved electrochemical immunosensor for myeloperoxidase in human serum based on nanogold/cerium dioxide-BMIMPF6/L-Cysteine composite film. Colloids Surf B Biointerfaces. 2011;86:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 88. | Yin ZJ, Wu JJ, Yang ZS. A sensitive mercury (II) sensor based on CuO nanoshuttles/ poly(thionine)modified glassy carbon electrode. Microchim Acta. 2010;170:307-312. [RCA] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 89. | Wang L, Sun Y, Wang J, Wang J, Yu A, Zhang H, Song D. Preparation of surface plasmon resonance biosensor based on magnetic core/shell Fe3O4/SiO2 and Fe3O4/Ag/SiO2 nanoparticles. Colloids Surf B Biointerfaces. 2011;84:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 90. | Li MJ, Dai XF, Liu ZM, Cai PX, Bai Y. A hepatitis C electrochemical immunosensor based on thionine covalently bound to self-assembled monolayer. Fenxi Huaxue. 2005;33:1701-1704. |
| 91. | Ma C, Xie G, Zhang W, Liang M, Liu B, Xiang H. Label-free sandwich type of immunosensor for hepatitis C virus core antigen based on the use of gold nanoparticles on a nanostructured metal oxide surface. Microchimica Acta. 2012;178:331-340. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 92. | Ma C, Liang M, Wang L, Xiang H, Jiang Y, Li Y, Xie G. MultisHRP-DNA-coated CMWNTs as signal labels for an ultrasensitive hepatitis C virus core antigen electrochemical immunosensor. Biosens Bioelectron. 2013;47:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 93. | Liang M, Wang L, Ma CX, Zhang MJ, Xie GM. Sandwich immunoassay for hepatitis C virus non-structural 5A protein using a glassy carbon electrode modified with an Au-MoO3/chitosan nanocomposite. Anal Letters. 2013;46:1241-1254. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 94. | Moraes ML, Lima LR, Silva RR, Cavicchioli M, Ribeiro SJ. Immunosensor based on immobilization of antigenic peptide NS5A-1 from HCV and silk fibroin in nanostructured films. Langmuir. 2013;29:3829-3834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 95. | Konig B, Gratzel M. A piezoelectric immunosensor for hepatitis viruses. Anal Chim Acta. 1995;309:19-25. [RCA] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 96. | Chen ZZ, Wang KM, Chen YK, Xiao D, Yang XH, Shao GQ. Development of a piezoelectric immunosensor for hepatitis B surface antigen. Gaodeng Xuexiao Huaxue Xuebao. 2002;23:1044-1046. |
| 97. | Chen ZZ, Wang KM, Yang XH, Huang SS, Huang HM, Li D, Wang Q. Determination of hepatitis B surface antigen by surface plasmon resonance biosensor. Acta Chimica Sinica. 2003;61:137-140. |
| 98. | Kintzios S, Pistola E, Konstas J, Bem F, Matakiadis T, Alexandropoulos N, Biselis I, Levin R. The application of the bioelectric recognition assay for the detection of human and plant viruses: definition of operational parameters. Biosens Bioelectron. 2001;16:467-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 99. | Lee JC, Shih YF, Hsu SP, Chang TY, Chen LH, Hsu JT. Development of a cell-based assay for monitoring specific hepatitis C virus NS3/4A protease activity in mammalian cells. Anal Biochem. 2003;316:162-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 100. | Mitsui T, Iwano K, Masuko K, Yamazaki C, Okamoto H, Tsuda F, Tanaka T, Mishiro S. Hepatitis C virus infection in medical personnel after needlestick accident. Hepatology. 1992;16:1109-1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 226] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 101. | Young KKY, Resnick R, Myers TW. Detection of hepatitis C virus RNA by a combined reverse transcriptase-polymerase chain reaction assay. J Clin Microbiol. 1993;31:882-886. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 102. | Hennig H, Luhm J, Hartwig D, Klüter H, Kirchner H. A novel RT-PCR for reliable and rapid HCV RNA screening of blood donations. Transfusion. 2001;41:1100-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 103. | Richalet-Sécordel PM, Poisson F, Van Regenmortel MH. Uses of biosensor technology in the development of probes for viral diagnosis. Clin Diagn Virol. 1996;5:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 104. | O'Meara D, Nilsson P, Nygren PA, Uhlén M, Lundeberg J. Capture of single-stranded DNA assisted by oligonucleotide modules. Anal Biochem. 1998;255:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 105. | O'Meara D, Yun Z, Sönnerborg A, Lundeberg J. Cooperative oligonucleotides mediating direct capture of hepatitis C virus RNA from serum. J Clin Microbiol. 1998;36:2454-2459. [PubMed] |
| 106. | Liu A, Wang K, Weng S, Lei Y, Lin L, Chen W, Lin X, Chen Y. Development of electrochemical DNA biosensors. Trends Analyt Chem. 2012;37:101-111. [RCA] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 107. | Paleček E, Fojta M. Electrochemical DNA sensors. Bioelectronics: from theory to applications. Jerusalem: Wiley 2006; 127-192. |
| 108. | Mascini M, Palchetti I, Marrazza G. DNA electrochemical biosensors. Fresenius J Anal Chem. 2001;369:15-22. [PubMed] |
| 109. | Pividori MI, Merkoçi A, Alegret S. Electrochemical genosensor design: immobilisation of oligonucleotides onto transducer surfaces and detection methods. Biosens Bioelectron. 2000;15:291-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 239] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 110. | Teles FRR, Fonseca LP. Trends in DNA biosensors. Talanta. 2008;77:606-623. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 284] [Cited by in RCA: 225] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 111. | Kadkol SS, Gage WR, Pasternack GR. In situ hybridization-theory and practice. Mol Diagn. 1999;4:169-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 112. | Skládal P, dos Santos Riccardi C, Yamanaka H, da Costa PI. Piezoelectric biosensors for real-time monitoring of hybridization and detection of hepatitis C virus. J Virol Methods. 2004;117:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 113. | Uliana CV, Tognolli JO, Yamanaka H. Application of factorial design experiments to the development of a disposable amperometric DNA biosensor. Electroanalysis. 2011;23:2607-2615. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 114. | Souza E, Nascimento G, Santana N, Ferreira D, Lima M, Natividade E, Martins D, Lima-Filho J. Label-free electrochemical detection of the specific oligonucleotide sequence of dengue virus type 1 on pencil graphite electrodes. Sensors (Basel). 2011;11:5616-5629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 115. | Ligaj M, Jasnowska J, Musiał WG, Filipiak , M . Covalent attachment of single-stranded DNA to carbon paste electrode modified by activated carboxyl groups. Electrochim Acta. 2006;51:5193-5198. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 116. | Vermeeren V, Wenmackers S, Wagner P, Michiels L. DNA sensors with diamond as a promising alternative transducer material. Sensors (Basel). 2009;9:5600-5636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 117. | Pividori MI, Alegret S. DNA adsorption on carbonaceous materials. Top Curr Chem. 2005;260:1-36. [RCA] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 118. | Labuda J, Brett AMO, Evtugyn G, Fojta M, Mascini M, Ozsoz M, Palchetti I, Paleček E, Wang J. Electrochemical nucleic acid-based biosensors: concepts, terms, and methodology (IUPAC Technical Report). Pure Appl Chem. 2010;82:1161-1187. [RCA] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 162] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 119. | Wang J. Electrochemical nucleic acid biosensors. Anal Chim Acta. 2002;469:63-71. [RCA] [DOI] [Full Text] [Cited by in Crossref: 458] [Cited by in RCA: 368] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 120. | Park JY, Park SM. DNA hybridization sensors based on electrochemical impedance spectroscopy as a detection tool. Sensors (Basel). 2009;9:9513-9532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 121. | Kerman K, Kobayashi M, Tamiya E. Recent trends in electrochemical DNA biosensor technology. Meas Sci Technol. 2004;15:R1-R11. [DOI] [Full Text] |
| 122. | Paleček E, Bartošík M. Electrochemistry of nucleic acids. Chem Rev. 2012;112:3427-3481. [RCA] [DOI] [Full Text] [Cited by in Crossref: 515] [Cited by in RCA: 470] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 123. | dos Santos Riccardi C, Kranz C, Kowalik J, Yamanaka H, Mizaikoff B, Josowicz M. Label-free DNA detection of hepatitis C virus based on modified conducting polypyrrole films at microelectrodes and atomic force microscopy tip-integrated electrodes. Anal Chem. 2008;80:237-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 124. | Pournaghi-Azar MH, Ahour F, Hejaz MS. Differential pulse voltammetric detection of hepatitis c virus 1a oligonucleotide chain by a label-free electrochemical DNA hybridization biosensor using consensus sequence of hepatitis c virus 1a probe on the pencil graphite electrode. Electroanalysis. 2009;21:1822-1828. [RCA] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 125. | Riccardi Cdos S, Dahmouche K, Santilli CV, da Costa PI, Yamanaka H. Immobilization of streptavidin in sol-gel films: Application on the diagnosis of hepatitis C virus. Talanta. 2006;70:637-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 126. | Uliana CV, Riccardi CS, Tognolli JO, Yamanaka H. Optimization of an amperometric biosensor for detection of Hepatitis C virus using fractional factorial designs. J Braz Chem Soc. 2008;19:782-787. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 127. | Umek RM, Lin SW, Vielmetter J, Terbrueggen RH, Irvine B, Yu CJ, Kayyem JF, Yowanto H, Blackburn GF, Farkas DH. Electronic detection of nucleic acids: a versatile platform for molecular diagnostics. J Mol Diagn. 2001;3:74-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 161] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 128. | Liu S, Hu Y, Jin J, Zhang H, Cai C. Electrochemical detection of hepatitis C virus based on site-specific DNA cleavage of BamHI endonuclease. Chem Commun (Camb). 2009;1635-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 129. | Vanamee ÉS, Viadiu H, Lukacs CM, Aggarwal AK. Two of a kind: BamHI and BglII. Restriction endonucleases. Heidelberg: Springer 2004; 215-233. |
| 130. | Liu S, Wu P, Li W, Zhang H, Cai C. Ultrasensitive and selective electrochemical identification of hepatitis C virus genotype 1b based on specific endonuclease combined with gold nanoparticles signal amplification. Anal Chem. 2011;83:4752-4758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 131. | Nielsen PE. The many faces of PNA. Peptide nucleic acids, morpholinos and related antisense biomolecules. New York: Springer 2006; 3-13. |
| 132. | Nielsen PE, Egholm M. An introduction to peptide nucleic acid. Curr Issues Mol Biol. 1999;1:89-104. [PubMed] |
| 133. | Park JY, Lee YS, Chang BY, Kim BH, Jeon S, Park SM. Label-free impedimetric sensor for a ribonucleic acid oligomer specific to hepatitis C virus at a self-assembled monolayer-covered electrode. Anal Chem. 2010;82:8342-8348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 134. | Hejazi MS, Pournaghi-Azar MH, Ahour F. Electrochemical detection of short sequences of hepatitis C 3a virus using a peptide nucleic acid-assembled gold electrode. Anal Biochem. 2010;399:118-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 135. | Pournaghi-Azar MH, Ahour F, Hejazi MS. Direct detection and discrimination of double-stranded oligonucleotide corresponding to hepatitis C virus genotype 3a using an electrochemical DNA biosensor based on peptide nucleic acid and double-stranded DNA hybridization. Anal Bioanal Chem. 2010;397:3581-3587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 136. | Ahour F, Pournaghi-Azara MH, Hejazi MS. An electrochemical approach for direct detection and discrimination of fully match and single base mismatch double-stranded oligonucleotides corresponding to universal region of hepatitis C virus. Anal Methods. 2012;4:967-972. [DOI] [Full Text] |
| 137. | Ahour F, Pournaghi-Azar MH, Alipour E, Hejazi MS. Detection and discrimination of recombinant plasmid encoding hepatitis C virus core/E1 gene based on PNA and double-stranded DNA hybridization. Biosens Bioelectron. 2013;45:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 138. | Zhang Z, Li X, Wang C, Xiong Y, Liu P, Zhang C. Cobalt complex plays a dual role in the construction of E-DNA sensor. J Electroanal Chem. 2013;690:117-120. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 139. | Sam SS, Steinmetz HB, Tsongalis GJ, Tafe LJ, Lefferts JA. Validation of a solid-phase electrochemical array for genotyping hepatitis C virus. Exp Mol Pathol. 2013;95:18-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |