Published online Nov 7, 2014. doi: 10.3748/wjg.v20.i41.15462
Revised: July 25, 2014
Accepted: September 29, 2014
Published online: November 7, 2014
Processing time: 218 Days and 1.8 Hours
Acquired vesico-rectal fistula is an uncommon complication of pelvic malignant tumors, surgical injury, inflammatory disorders such as tuberculosis infection, radiotherapy and less commonly diverticulum of the urinary tract. The fistula is often identified by urinary tract abnormalities such as dysuria, recurrent urinary tract infection, pneumaturia, and fecaluria. Here, we report an unusual case of a patient with a vesico-rectal fistula of tuberculous origin, presenting with severe acute diarrhea, metabolic acidosis, hyperchloremia and hypokalemia while with only mild urinary tract symptoms. The patient was cured by tuberculostatic therapy.
Core tip: A tuberculous vesico-rectal fistula presenting with severe acute diarrhea, metabolic acidosis, hyperchloremia and hypokalemia while with only mild urinary tract symptoms is uncommon. Physicians should bear in mind that diarrhea and acidosis can be caused by vesico-rectal fistula as a rare cause and can be cured by tuberculostatic therapy.
- Citation: Wei XQ, Zou Y, Wu ZE, Abassa KK, Mao W, Tao J, Kang Z, Wen ZF, Wu B. Acute diarrhea and metabolic acidosis caused by tuberculous vesico-rectal fistula. World J Gastroenterol 2014; 20(41): 15462-15466
- URL: https://www.wjgnet.com/1007-9327/full/v20/i41/15462.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i41.15462
Acquired entero-vesical fistula and vesico-enteral fistula are uncommon complications of colorectal and pelvic malignant tumors, surgical injury, inflammatory disorders such as tuberculosis infection and Crohn’s disease, radiotherapy and less commonly diverticulum of the urinary tract or the intestinal tract[1]. The fistulas are often characterized by recurrent urinary tract infection, dysuria, fecaluria, pneumaturia or sometimes by intestinal abnormalities such as diarrhea, melena and hematemesis[2]. There have also been a few reports concerning electrolytes and acid-base disturbance[3,4]. Here, we present a rare case of a male with a vesico-rectal fistula of tuberculous origin, characterized by severe acute diarrhea, metabolic acidosis, hypokalemia and hyperchloremia while with only mild urinary tract symptoms. The symptoms were relieved totally after one month’s tuberculostatic therapy.
A 41-year-old male was referred to the department of gastroenterology of our hospital in March 2012 from a local hospital because of sustaining diarrhea for one month. A month prior to his admission, the patient had noticed a dramatic change in his stool habit, passing yellowish watery stool 7-10 times a day, almost 100-200 mL each time, but there were no rectal tenesmus, bloody diarrhea, melena, hematemesis or fever. He complained of oliguria, mild dry mouth, occasionally nausea without vomiting, anorexia and mild intermittent lower abdominal pain that radiated to the lower back and was relieved after bowel movements. The daily urine volume was only 200-300 mL. He reported no fatigue, urinary frequency, urgency of micturition, odynuria, dysuria, hematuria, pneumaturia, fecal uriao, arthralgia, chest pain or cough. Five days prior to his admission, he started passing dark urine which he described as “black tea in color”, but still no urinary frequency, urgency of micturition and dysuria were noted. He had lost weight of more than 5 kg in the past six months. On physical examination, he was afebrile, and had rigid abdomen, lower abdominal tenderness, tender ureter on palpation, tender flank, especially in the kidney area, tender lumbocostal point, and active bowel sounds. Other physical examinations were unremarkable.
Routine stool tests showed increased erythrocytes (++) and leukocytes (++) for one time, but did not reveal any erythrocytes or leukocytes for two times during the first three days of hospitalization. Urine analysis was as follows (normal range in parentheses): pH 6.7 (5.4-8.4), specific gravity 1.020 (1.003-1.030), protein+, occult blood+++, urine erythrocytes 2753.3 counts/μL (0-18 counts/μL), and urine leukocytes 33308.3 counts/μL (0-18 counts/μL). Phase-contrast microscopic examination showed that all the urine red blood cells (RBC) were not malformed. Although the daily urine volume was only 250 mL, the urine chemistry showed sodium 81.4 mmol/L, potassium 14.8 mmol/L, chloride 130 mmol/L, and urine anion gap (sodium + potassium - chloride) -34.2 mmol/L. Laboratory blood tests showed the following indexes: hemoglobin 74 g/L (120-140 g/L), peripheral white cell count 9.85 × 109/L (5 × 109-10 × 109/L), neutrophils 78.7% (40%-60%), peripheral red cell count 3.03 × 1012/L (4.0 × 1012-4.5 × 1012/L), platelet count 685 ×109/L (100 × 109-300 × 109/L), peripheral eosinophil count 0.07 × 109/L (0.02 × 109-0.52 × 109/L) , serum sodium 134.7 mmol/L(137-147 mmol/L), serum potassium 2.64 mmol/L (3.5-5.3 mmol/L), serum chloride 119.2 mmol/L (99-110 mmol/L), serum HCO3- 11.4 mmol/L (20.2-29.2 mmol/L), and serum anion gap (sodium + potassium - chloride - HCO3-) 6.74 mmol/L (8-16mmol/L). Arterial blood gas analysis (under ambient conditions) revealed pH 7.23 (7.35-7.45), PaCO2 22.5 mmHg (35-45 mmHg) and PaO2 98 mmHg (80-100 mmHg), albumin 33.9 g/L (36-51 g/L), total immunoglobulin 34.3g/L (25-35g/L ), total bilirubin 5.3 μmol/L (4-23.9 μmol/L), alkaline phosphatase 57 U/L (35-125 U/L), c-glutamyltranspeptidase 18U/L (7-50 U/L), aspartate aminotransferase 8 U/L (14-40U/L), alanine aminotransferase 11 U/L (5-35 U/L), creatinine 129.9 μmol/L (31.8-91.0 μmol/L), blood urine nitrogen 7.88 g/L (2.4-8.2 g/L), uric acid 184 μmol/L (90-420 μmol/L), prothrombin time 13.6 s (11.0-14.5 s), C-reactive protein 49.5mg/L (0-6.0 mg/L), erythrocyte sedimentation rate 140 mm/h (0-20 mm/h); and serum carcinoembryonic antigen (CEA) alpha-fetoprotein (AFP), cancer antigen 125(CA125) and cancer antigen 19-9 (CA19-9) were 1.1 μg/L (0-5 μg/L), 1.7 μg/L (0-8 μg/L), 17.2 U/mL (0-35U/mL) and 6.14 U/mL (0-35U/mL), respectively. Hepatitis B and C markers were negative. Antinuclear antibodies (ANA), antineutrophilcytoplasmic antibody (ANCA) and rheumatoid factor (RF) were not found in the blood. Tuberculosis (TB)-related antibodies were present in the blood, and the TB-purified protein derivative (PPD) skin test was strongly positive, while serum adenosine deaminase (ADA) level was within normal range as 7 U/L (4-22 U/L). T-SPOT.TB test was positive, indicating the presence of an active tuberculosis infection. All these abnormal results became normal when the patient was followed up one year later.
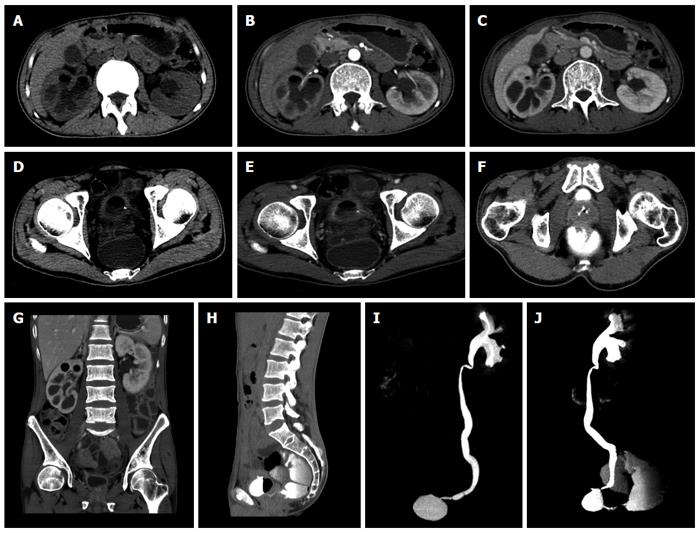
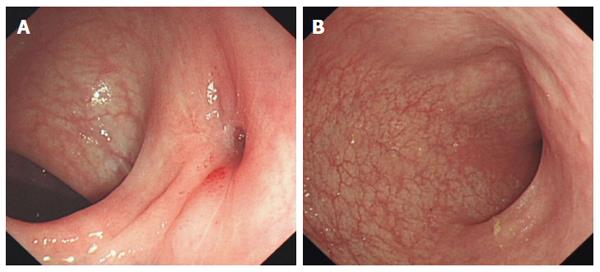
Abdominal computed tomography (CT) scan and CT urography (CTU) revealed a vesico-rectal fistula, an infection pattern (with suspected tuberculosis) on the right kidney and right ureter with right renal insufficiency and left ureto-cystic stones with hydronephrosis (Figure 1). To our regret, the patient refused a follow-up abdominal CT scan and CTU examination for economic reasons. Colonoscopy was performed and revealed a circumscribed fistulous tract arising from the anterior rectal wall located at 4 cm proximal to anus, with red and swollen surrounding mucosa, which disappeared totally after 12 mo treatment (Figure 2). However, the biopsy of the surrounding mucosa only revealed chronic inflammation.
Sodium bicarbonate 2 g and potassium citrate 1 g three times a day were supplemented to treat the metabolic acidosis, and the serum levels of potassium, chloride and bicarbonate all became normal soon after 3 d treatment. Before admission and during the beginning period of admission, the patient was started on an intravenous levofloxacin 0.5 g once a day for 10 d as experimental antibacterial therapy in a local hospital and our department. Antidiarrheal drugs (smectite powder 3 g tid) and antispasmic drugs (drotaverine hydrochloride 40 mg tid) were also prescribed by us, but there was no relief of diarrhea. According to the results of CTU and T-SPOT.TB, the antibiotic was stopped and the patient was given isoniazide 0.3 g and rifampicin 0.45 g once a day, and pyrazinamid 0.25 g tid. Fortunately, the diarrhea disappeared totally 4 wk later and no surgery was needed. Sodium bicarbonate and potassium citrate supplementations were no longer needed. After 12 mo tuberculostatic therapy, the patient received an ureteroscopic lithotripsy in another hospital and he has reported no abnormalities since then.
Acquired fistulas between the urinary tract and the intestine are uncommon complications of colorectal and pelvic malignant tumors, surgical injury, inflammatory disorders such as tuberculosis infection and Crohn’s disease, radiotherapy and less commonly diverticulum of the urinary tract or the gastrointestinal tract[1]. The most common symptoms of these acquired fistulas are recurrent urinary tract infection, dysuria, fecaluria, pneumaturia, ect. While the intestinal symptoms such as diarrhea may also be the main complaint sometimes[2]. In this paper, we report an untypical case with acute diarrhea, hyperchloremic metabolic acidosis and hypokalemia caused by a vesico-rectal fistula of tuberculous origin, while with only mild urinary tract symptoms and without fever and night sweating. Although numerous red blood cells and white blood cells were found in the urine which indicated a severe inflammation of the urinary tract, acute diarrhea was the chief complaint by this patient and there were no prominent symptoms of the urinary tract. Usually, the most possible cause of diarrhea, metabolic acidosis and hypokalemia occurring simultaneously should be colitis of various causes, however, the experimental antibacterial treatment for an infectious colitis and antidiarrheal drugs did not work in this case. The tuberculosis infection of urinary tract and the acquired tuberculous vesico-rectal fistula were identified to be the cause in the end.
In urological diseases, it is well known that both the reconstruction of the urinary tract with parts of the gastrointestinal tract and urinary diversion can cause acid-base disturbances. The mechanism of acid-base disturbance is mainly as the followings: when the urine that is delivered by the fistula passes through the lower gut, serum bicarbonate will be excreted and chloride will be absorbed by the Cl-/HCO3- exchangers in the intestinal epithelia; when the urine passes through the colon, the urease of some certain bacteria can convert the urea into bicarbonate ion and ammonium ion, and then a lot of bicarbonate ions will be excreted into the stool and a lot of ammonium ions will be reabsorbed together with chloride or in exchange with sodium[5,6]. Since the urinary anion gap in this case was negative, an intact ability of increasing the excretion of ammonium ions through urine was indicated. Systemic depletion of potassium and hypokalemia have also been reported as a possible complication of ureterosigmoidostomy before[7]. The hypokalemia of this case should be a result of the loss of potassium contained in the watery stools.
With the extensive use of the noninvasive CT scan with or without 3-dimensional reconstruction, the diagnosis of colovesical fistulas and vesico-rectal fistulas becomes more accurate. In a group of 24 patients with enterovesical fistulas, Sarr et al[8] found that the diagnostic sensitivity of CT scan was 100%, while those of the small intestinal radiography, the cystoscopy, the cystogram and the intravenous pyelogram were as low as 38%, 6%, 4% and 0% respectively. Positive CT scan findings had been obtained as the followings: the phenomenon that the thickened bladder wall contacted intimately with the thickened intestinal wall at the site of a fistula was found in all the 24 patients and the air within the bladder without a recent history of transurethral instrumentation was seen in 20 patients. These findings show that CT scan is the most accurate method to make the diagnosis of colovesical fistulas and should be taken as an initial evaluation for suspected enterovesical fistulas or vesico-enteral fistulas[9]. In comparison with conventional CT, 3-dimensional CT can provide a better and more complete visualization of the anatomic relationship between the colon and the bladder in colovesical fistulas and vesico-rectal fistulas and can provide further aids in making a diagnosis and in facilitating the surgical operation[10-12]. As a matter of fact, the differential diagnosis between enterovesical fistulas and vesico-enteral fistulas is not easy sometimes; colonoendoscopic examination and cystoscopic examination may be of great help. The diagnosis of vesico-rectal fistula was made by abdominal CT and CTU in our patient, and confirmed by colon endoscopic examination.
Although most of the vesico-rectal fistulas and colovesical fistulas are cured via surgery[13-16], the knowledge of the treatment for tuberculous vesico-rectal fistula is very limited. Here, we report a rare case of tuberculous vesico-rectal fistula presenting with severe acute diarrhea, metabolic acidosis and hypokalemia cured by tuberculostatic therapy and supplementation of sodium bicarbonate and potassium citrate. This will add important knowledge to the literature. However, it still remains undetermined whether all tuberculous fistulas can be cured by conservative therapy.
In conclusion, gastroenterologists should keep in mind that diarrhea and acidosis can be caused by vesico-rectal fistula as a rare cause and tuberculous vesico-rectal fistula can be cured by conservative therapy in the case reported here. CT scan with or without 3-dimensional reconstruction should be taken intially to make the diagnosis of vesico-enteral fistulas and enterovesical fistulas.
A 41-year-old man presented with severe acute diarrhea, metabolic acidosis, hyperchloremia and hypokalemia while with only mild urinary tract symptoms.
Severe acute diarrhea and hyperchloremic metabolic acidosis caused by a tuberculous vesico-rectal fistula.
Recto-vesical fistula and colitis.
Tuberculosis-related antibodies, positive; T-SPOT.TB, positive; serum potassium 2.64 mmol/L; serum chloride 119.2 mmol/L; serum HCO3-, 11.4 mmol/L; and arterial blood pH 7.23.
Computed tomography scan revealed a vesico-rectal fistula and a suspected tuberculosis infection of the right kidney and the right ureter.
Tuberculosis was not confirmed by the pathological diagnosis since the biopsy was taken from the rectum but not from the bladder.
Tuberculostatic therapy was prescribed.
It is not easy to establish a diagnosis of vesico-rectal fistulas presenting with severe acute diarrhea and hyperchloremic metabolic acidosis since it is very rare.
Vesico-rectal fistulas are fistulas between the bladder and the rectum which are caused by the bladder disorders of various causes.
Tuberculous vesico-rectal fistulas can be presented with severe acute diarrhea, metabolic acidosis, hyperchloremia and hypokalemia while with only mild urinary tract symptom, and can be cured by tuberculostatic therapy.
The case report is focussed on a very important topic, intestinal tuberculosis. The report is well-illustrated and well-written. Clincial key points of diagnosis and outcome are addressed. The report could be improved by demonstrating histological features.
P- Reviewer: Bassotti G, Gassler N, Lakatos PL, Luo HS S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
| 1. | Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188:617-621. [PubMed] |
| 2. | Kurtz LE, Sheikh JM, Greenberg RE. Image of the month. Acute diarrhea caused by a rectovesical fistula after laparoscopic prostatectomy. Clin Gastroenterol Hepatol. 2010;8:A30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Murakami K, Tomita M, Kawamura N, Hasegawa M, Nabeshima K, Hiki Y, Sugiyama S. Severe metabolic acidosis and hypokalemia in a patient with enterovesical fistula. Clin Exp Nephrol. 2007;11:225-229. [PubMed] |
| 4. | Pillinger T, Abdelrahman M, Jones G, D’Souza F. Intractable metabolic acidosis in a patient with colovesical fistula. N Z Med J. 2012;125:74-76. [PubMed] |
| 5. | Castro JE, Ram MD. Electrolyte imbalance following ileal urinary diversion. Br J Urol. 1970;42:29-32. [PubMed] |
| 6. | Kunzelmann K, Mall M. Electrolyte transport in the mammalian colon: mechanisms and implications for disease. Physiol Rev. 2002;82:245-289. [PubMed] |
| 7. | Koff SA. Mechanism of electrolyte imbalance following urointestinal anastomosis. Urology. 1975;5:109-114. [PubMed] |
| 8. | Sarr MG, Fishman EK, Goldman SM, Siegelman SS, Cameron JL. Enterovesical fistula. Surg Gynecol Obstet. 1987;164:41-48. [PubMed] |
| 9. | Holroyd DJ, Banerjee S, Beavan M, Prentice R, Vijay V, Warren SJ. Colovaginal and colovesical fistulae: the diagnostic paradigm. Tech Coloproctol. 2012;16:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Shinojima T, Nakajima F, Koizumi J. Efficacy of 3-D computed tomographic reconstruction in evaluating anatomical relationships of colovesical fistula. Int J Urol. 2002;9:230-232. [PubMed] |
| 11. | Nadır I, Ozın Y, Kiliç ZM, Oğuz D, Ulker A, Arda K. Colovesical fistula as a complication of colonic diverticulosis: diagnosis with virtual colonoscopy. Turk J Gastroenterol. 2011;22:86-88. [PubMed] |
| 12. | Croitoru S, Moskovitz B, Nativ O, Barmeir E, Hiller N. Diagnostic potential of virtual pneumoendoscopy of the urinary tract. Abdom Imaging. 2008;33:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Lynn ET, Ranasinghe NE, Dallas KB, Divino CM. Management and outcomes of colovesical fistula repair. Am Surg. 2012;78:514-518. [PubMed] |
| 14. | Niebling M, van Nunspeet L, Zwaving H, Eddes EH, Bosker R, Eeftinck Schattenkerk M. Management of colovesical fistulae caused by diverticulitis: 12 years of experience in one medical centre. Acta Chir Belg. 2013;113:30-34. [PubMed] |
| 15. | Bouassida M, Mighri MM, Trigui K, Chtourou MF, Sassi S, Feidi B, Chebbi F, Bouzaidi K, Touinsi H, Sassi S. Meckel’s diverticulum: an exceptional cause of vesicoenteric fistula: case report and literature review. Pan Afr Med J. 2013;15:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Marney LA, Ho YH. Laparoscopic management of diverticular colovesical fistula: experience in 15 cases and review of the literature. Int Surg. 2013;98:101-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |