Published online Nov 7, 2014. doi: 10.3748/wjg.v20.i41.15448
Revised: May 7, 2014
Accepted: August 13, 2014
Published online: November 7, 2014
Processing time: 250 Days and 7.6 Hours
Primary giant-cell tumors rarely arise in the common bile duct. We herein report a case of primary giant-cell tumor of the common bile duct. The patient was an 81-year-old male who was diagnosed with a well-defined 1.2-cm mass projecting into the lumen of the middle common bile duct. Excision of the gallbladder and extrahepatic bile duct and a Roux-en-Y cholangiojejunostomy were performed. Histologically, the tumor had no association with carcinomas of epithelial origin and was similar to giant-cell tumors of the bone. The tumor consisted of a mixture of mononuclear and multinucleated osteoclast-like giant cells. The mononuclear cells showed no atypical features, and their nuclei were similar to those of the multinucleated giant cells. CD68 was expressed on the mononuclear and multinucleated osteoclast-like giant cells, whereas CD163 immunoreactivity was restricted to the mononuclear cells. Six months after the operation, the patient was still alive and had no recurrence. The interest of this case lies in the rarity of this entity, the difficulty of preoperative diagnosis, and this tumor’s possible confusion with other malignant tumors.
Core tip: In visceral organs, different types of carcinomas, such as anaplastic spindle- and giant-cell carcinomas of the gallbladder and extrahepatic bile duct, may contain a variable number of osteoclast-like giant cells. It is crucial to separate those carcinomas with osteoclast-like giant cells from giant-cell tumors because of their striking differences in prognosis. This case report represents the fifth case of a primary giant-cell tumor of the common bile duct in the English-language literature. We also review several reported cases to summarize clinical information about this rare tumor.
- Citation: Wang DD, Zheng YM, Teng LH, Sun YN, Gao W, Wang LM, Wang YH, Li F, Lu DH. Benign giant-cell tumor of the common bile duct: A case report. World J Gastroenterol 2014; 20(41): 15448-15453
- URL: https://www.wjgnet.com/1007-9327/full/v20/i41/15448.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i41.15448
Giant-cell tumors of the bone are a relatively common type of proliferative neoplasm. Extraosseous giant-cell tumors with histological features similar to those occurring in the bone are rare, and these tumors have been described at several sites including the soft tissues, mediastinum, larynx, thyroid, and skin[1-6]. Benign giant cell tumors of the extrahepatic biliary tree are extremely rare and under-recognized. A primary giant-cell tumor of the extrahepatic biliary tree was first recognized as a biologically benign neoplasm by Albores-Saavedra et al[7] in 2006. To our knowledge, the case that we are reporting is the fifth case of a primary giant-cell tumor of the common bile duct in the English-language literature. We also review several reported cases to summarize clinical information about this rare tumor.
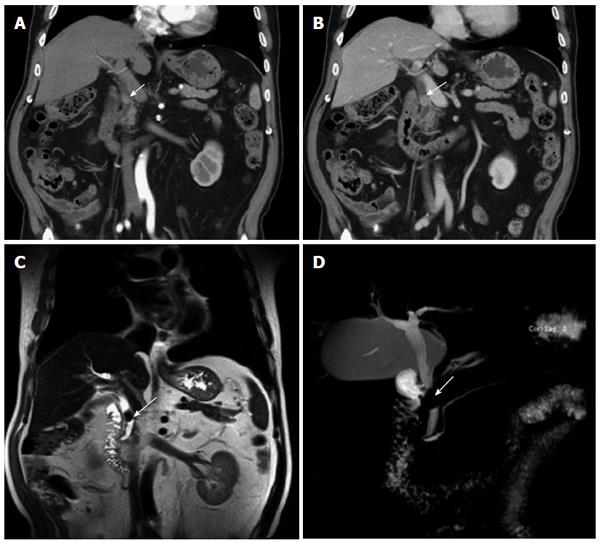
An 81-year-old male presented at our hospital with a complaint of general fatigue and abdominal dull pain for a month. His medical history included high blood pressure and cerebrovascular disease. Physical examination revealed slight jaundice and scleral icterus. His abdomen was flat and soft, and percussion pain was found in the hepatic region. The results of laboratory tests, including a complete blood count and measurements of serum amylase, glucose, electrolytes and liver and kidney function, were normal. The level of the tumor marker carbohydrate antigen 19-9 (CA19-9) was normal (13.87 U/mL). The level of alanine aminotransferase was 34 IU/L; total bilirubin, 14.76 μmol/L; direct bilirubin, 5.41 μmol/L; γ-glutamate transaminase, 56 IU/L; and carcinoembryonic antigen, 1.89 ng/mL. A computed tomography (CT) scan of the abdomen revealed a dilated common bile duct, with a 1.2-cm mass projecting into the lumen of the middle common bile duct, causing nearly complete obstruction (Figure 1A). Intravenous administration of contrast medium showing mild enhancement of the tumor (Figure 1B). Magnetic resonance imaging (MRI, Figure 1C) and magnetic resonance cholangiopancreatography (MRCP, Figure 1D) revealed stenosis of the common bile duct. The tumor had a relatively well-defined border. Additionally, the gallbladder was markedly distended. A clinical diagnosis of carcinoma was suspected.
After a multidisciplinary review, the patient was offered surgical resection of the lesion. Excision of the gallbladder and extrahepatic bile duct and a Roux-en-Y cholangiojejunostomy were performed. At laparotomy, gallbladder enlargement and widened proximal bile duct were found, and there was no evidence of an extraductal tumor or lymphadenopathy.
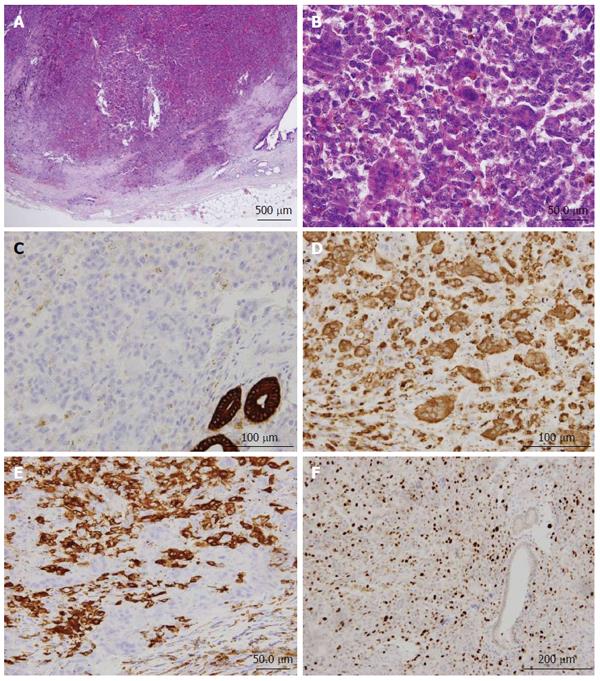
Postoperative gross pathology revealed a 1.5 cm × 0.6 cm × 0.6 cm polypoid lesion in the middle of the common bile duct. The tumor tissue was characterized as hemorrhage (Figure 2).
Microscopically, the tumor was polypoid, showed a vaguely nodular pattern and infiltrated into the wall (Figure 3A). The nodules consisted of conspicuous proliferation of two morphological components, including an abundance of multinucleated osteoclast-like giant cells and a relatively homogeneous population of round to polygonal mononuclear cells (Figure 3A and B). The quantity and quality of the giant cell component were similar to those identified in primary giant cell tumors of the bone. The mononuclear cells had oval or round vesicular nuclei with small and medium-sized nucleoli. No mitotic figures were found. The nuclei of the giant cells were similar to those of the mononuclear cells. The cytoplasm was slightly basophilic. Areas of red-cell extravasation were common, but there was no cystic degeneration, osteoid, or bone formation. Vascular invasion was not identified. A small amount of pancreatic tissue was found around the common bile duct.
Immunohistochemically, all cells except for the remaining epithelium of the bile duct were cytokeratin negative. No epithelial elements were observed in association with the mononuclear and multinucleated giant cells, as confirmed by negative immunostaining for epithelial markers, such as cytokeratins (including CK, CK7, CK20, and CK19) (Figure 3C) and EMA. CD68 (Figure 3D) and Vimentin showed strong granular immunoreactivity in both mononuclear and multinucleated osteoclast-like giant cells. In contrast, strong CD163 immunoreactivity was restricted to the mononuclear cells, not in the multinucleated giant cells (Figure 3E). Moreover, the mononuclear cells had an average Ki67 index of 10%-20% (Figure 3F). No vascular invasion was observed in the specimen. There were no adenoma-like structures. Based on these findings, the lesion was consistent with a diagnosis of a benign giant-cell tumor of the common bile duct. All margins were free of tumor.
There were no postoperative complications. The patient recovered smoothly and was discharged on postoperative day 8. No adjuvant chemotherapy was required. The tumor exhibited no signs of recurrence or metastatic spread after six months of follow-up.
Giant-cell tumors of the bone are distinct neoplasms with a characteristic histological appearance of mononuclear stromal cells and a varying number of multinucleated giant cells. Although uncertainty still exists as to the origin of the tumors, several authors have suggested a mesenchymal origin and have considered mononuclear cells to be the principal cell in these tumors. Multinucleated cells are thought to always be benign, whereas the presence of mononuclear giant cells is used to separate benign giant-cell tumors from malignant ones.
Extraosseous tumors containing osteoclast-like giant cells have been described at several sites in the body. Giant-cell tumors of the extrahepatic biliary tree are extremely rare and were first described by Albores-Saavedra et al[7] as biologically benign neoplasms. To the best of our knowledge, only six cases have been reported to date, among which four were located at the common bile duct, and the other two were located at the cystic duct and gallbladder, respectively[7-9]. In the extrahepatic bile duct, giant-cell tumors usually lead to obstruction and can be confused with carcinoma preoperatively based on clinical and imaging studies. In our case, carcinoma of the common bile duct was also suspected preoperatively. The vast majority of giant cell tumors of soft tissues have a benign clinical course[10], and the previous articles describing 4 patients with giant-cell tumors of the common bile duct suggested that they were benign tumors. None of the patients developed recurrence or metastatic disease. Thus, the best therapeutic option should be a conservative surgical resection with free surgical margins whenever possible.
Among those four previously reported giant-cell tumors of the common bile duct, three were treated using Whipple procedure, and the other one was treated by pylorus-preserving pancreas-head resection and pancreaticogastrostomy. In our case, the tumor was located in the middle of the common bile duct, and it had a relatively well-defined border, thus excision of the gallbladder and extrahepatic bile duct and a Roux-en-Y cholangiojejunostomy were adopted. Pathology analysis revealed that all margins were free of tumor, suggesting that the surgical treatment was enough for the patient. The clinical and pathological features of the cases of giant-cell tumors of the common bile duct published in the literature are shown in Table 1.
| PatientNo. | Ref. | Clinical presentation | Patient age (yr)/sex | Gross features | Treatment | Follow-up |
| 1 | Albores-Saavedra et al[7] | Jaundice, abdominal pain, CBD obstruction detected by CT and ERCP | 56/M | 1.6 cm polypoid nodule with invasion of the bile duct wall and obstruction of the lumen | Whipple procedure | Alive and disease-free 4 yr and 2 mo after surgery |
| 2 | Albores-Saavedra et al[7] | Obstructive jaundice, dilatation of CBD detected by CT | 60/M | 1 cm polypoid nodule without infiltration of the bile duct wall | Whipple procedure | No follow-up |
| 3 | Griglione et al[8] | Asymptomatic | 60/M | 1.5 cm polypoid lesion | Whipple procedure | Alive and disease-free 16 mo postoperatively |
| 4 | Kolokotronis et al[9] | Abdominal pain, high-grade stenosis of the distal bile duct, suspected distal common bile duct malignancy by ERCP | 73/F | 2.5 cm × 0.7 cm | Pylorus-preserving pancreas-head resection and pancreaticogastrostomy | No follow-up |
| 5 | Wang et al (this study) | Slight jaundice and scleral icterus | 81/M | 1.5 cm × 0.6 cm × 0.6 cm polypoid lesion | Excision of the gallbladder and extrahepatic bile duct and a Roux-en-Y cholangiojejunostomy | Alive and disease-free 6 mo after surgery |
The differential diagnosis of giant-cell tumor of the common bile duct includes metastatic giant cell tumor of the bone, anaplastic spindle- and giant-cell carcinomas with osteoclast-like giant cells, and malignant fibrous histiocytoma.
Grossly as well as histologically and immunohistochemically, giant cell tumor seems identical to its bony counterpart. Its characteristic brown color is described frequently in reports dealing with macroscopic features of giant cell tumor of the bone. Giant cell tumor of the soft tissue is devoid of atypia, pleomorphism, and atypical mitosis. This diagnosis of a giant-cell tumor of the common bile duct was considered primarily because no sign of another tumor could be found. In the reported cases of benign giant-cell tumors of the extrahepatic biliary tree, mononuclear cells have been described as uniform, with no atypia and a low mitosis rate, cytokeratin negativity, and CD163 expression[7]. In our patient, we found similar pathological findings. All of the tumor cells were completely negative for epithelial markers compared with the remaining normal bile duct while being positive for CD68 and CD163.
Anaplastic spindle and giant-cell carcinomas with osteoclast-like giant cells in the bile duct can also show numerous giant cells that may simulate giant-cell tumors[7]. However, anaplastic spindle and giant-cell carcinomas with osteoclast-like giant cells display marked atypia and mitotic figures and these carcinomas are focally cytokeratin positive and CD163 negative. The separation of giant-cell tumors from other malignant tumors is clinically relevant. To date, the tumor described here has shown no signs of recurrence or metastatic spread after 6 mo of follow-up.
The origin and nature of these giant cells are subjects of controversy. Three possibilities are usually considered: (1) the lesion is a carcinoma in which the tumor cells undergo a peculiar metaplasia; (2) the tumor arises from the mesenchyme with the capacity to differentiate into osseous tissues; or (3) the cells represent a host reaction to a primary tumor. That is, histiocytes may be recruited into the tumor by certain factors produced by the tumor and then may fuse to form multinucleated giant cells. In accordance with previous reports, the giant cells present in our patient showed immunohistochemical evidence of histiocytic derivation and lacked evidence of epithelial differentiation. These findings imply that the multinucleated giant cells and mononuclear stromal cells are a specialized form of macrophages.
In conclusion, giant-cell tumors of the common bile duct are rare but distinctive benign entities. It is crucial to differentiate benign giant-cell tumors of the common bile duct from other malignant tumors because of their different treatments and prognoses. Detailed cytologic analysis and immunohistochemical staining can help to clarify the diagnosis.
An 81-year-old male with an unremarkable medical history.
Slight jaundice and scleral icterus.
Carcinoma of the bile duct.
carbohydrate antigen 19-9, 13.87 U/mL; carcinoembryonic antigen, 1.89 ng/mL; alanine aminotransferase, 34 IU/L; total bilirubin, 14.76 μmol/L; direct bilirubin, 5.41 μmol/L; γ-glutamate transaminase, 56 IU/L.
A CT scan of the abdomen revealed a dilated common bile duct, with a 1.2-cm mass projecting into the lumen of the middle common bile duct, causing nearly complete obstruction.
Benign giant-cell tumor of the common bile duct, CD68/CD163 positive, CK/CK7/CK20/CK19 negative.
Excision of the gallbladder and extrahepatic bile duct and a Roux-en-Y cholangiojejunostomy were performed.
The giant cells present in our patient showed immunohistochemical evidence of histiocytic derivation and lacked evidence of epithelial differentiation.
This case report represents the fifth case of primary giant-cell tumor of the common bile duct in the English-language literature. It is crucial to differentiate this benign tumor from other carcinomas to avoid overtreatment.
This article reports a rare case of a benign giant-cell tumor of the common bile duct.
P- Reviewer: Miki K, Takumi K S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Liu XM
| 1. | Folpe AL, Morris RJ, Weiss SW. Soft tissue giant cell tumor of low malignant potential: a proposal for the reclassification of malignant giant cell tumor of soft parts. Mod Pathol. 1999;12:894-902. [PubMed] |
| 2. | Fu K, Moran CA, Suster S. Primary mediastinal giant cell tumors: a clinicopathologic and immunohistochemical study of two cases. Ann Diagn Pathol. 2002;6:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Hoang MP, Rogers BB, Albores-Saavedra J. Giant cell tumor of the skin: a morphologic and immunohistochemical study of five cases. Ann Diagn Pathol. 2002;6:288-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Maheswaran P, Addis BJ. Osteoclastoma-like giant cell tumour of the skin. Histopathology. 1990;16:604-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Wieneke JA, Gannon FH, Heffner DK, Thompson LD. Giant cell tumor of the larynx: a clinicopathologic series of eight cases and a review of the literature. Mod Pathol. 2001;14:1209-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Silverberg SG, DeGiorgi LS. Osteoclastoma-like giant cell tumor of the thyroid. Report of a case with prolonged survival following partial excision and radiotherapy. Cancer. 1973;31:621-625. [PubMed] |
| 7. | Albores-Saavedra J, Grider DJ, Wu J, Henson DE, Goodman ZD. Giant cell tumor of the extrahepatic biliary tree: a clinicopathologic study of 4 cases and comparison with anaplastic spindle and giant cell carcinoma with osteoclast-like giant cells. Am J Surg Pathol. 2006;30:495-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Griglione NM, Klapproth JM, Keilin SA. Giant cell tumor of the common bile duct. Clin Gastroenterol Hepatol. 2010;8:A30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Kolokotronis T, Glanemann M, Wagner M, Bohle RM, Grünhage F. Giant cell tumor of the distal common bile duct: report of a rare, benign entity that may mimic malignant biliary obstruction. Int J Colorectal Dis. 2014;29:413-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Oliveira AM, Dei Tos AP, Fletcher CD, Nascimento AG. Primary giant cell tumor of soft tissues: a study of 22 cases. Am J Surg Pathol. 2000;24:248-256. [PubMed] |