Published online Nov 7, 2014. doi: 10.3748/wjg.v20.i41.15153
Revised: January 10, 2014
Accepted: June 20, 2014
Published online: November 7, 2014
Processing time: 378 Days and 2.6 Hours
The use of minimally invasive surgery has become widely accepted in many gastrointestinal fields, even in patients with malignancy. However, performing laparoscopic resection for the treatment of hilar cholangiocarcinoma is still not universally accepted as an alternative approach to open surgery, and only a limited number of such procedures have been reported due to the difficulty of performing oncologic resection and the lack of consensus regarding the adequacy of this approach. Laparoscopy was initially limited to staging, biopsy and palliation. Recent technological developments and improvements in endoscopic procedures have greatly expanded the applications of laparoscopic liver resection and lymphadenectomy, and some reports have described the use of laparoscopic or robot-assisted laparoscopic resection for hilar cholangiocarcinoma as being feasible and safe in highly selected cases, with the ability to obtain an adequate surgical margin. However, the benefits of major laparoscopic surgery have yet to be conclusively proven, and carefully selecting patients is essential for successfully performing this procedure.
Core tip: Recent technological developments and improvements in endoscopic procedures have greatly expanded the applications of laparoscopic liver resection and lymphadenectomy, and some reports have described the use of laparoscopic or robot-assisted laparoscopic resection for hilar cholangiocarcinoma as being feasible and safe in highly selected cases, with the ability to obtain an adequate surgical margin. However, the benefits of major laparoscopic surgery have yet to be conclusively proven, and carefully selecting patients is essential for successfully performing this procedure.
- Citation: Cho A, Yamamoto H, Kainuma O, Muto Y, Yanagibashi H, Tonooka T, Masuda T. Laparoscopy in the management of hilar cholangiocarcinoma. World J Gastroenterol 2014; 20(41): 15153-15157
- URL: https://www.wjgnet.com/1007-9327/full/v20/i41/15153.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i41.15153
Hilar cholangiocarcinoma is the most common malignant neoplasm of the biliary tract. Only complete tumor resection enables the long-term survival of patients with hilar cholangiocarcinoma, and the use of major hepatic resection is often required to perform curative surgical resection[1-3]. However, major hepatic resection is reported to be closely associated with postoperative complications such as liver failure, sepsis and anastomotic leakage. Given the high surgical morbidity and mortality rates even at specialized high-volume centers[4], performing this procedure remains a formidable challenge for many surgeons. The recent rapid development of technological innovations, improvements in surgical skills and accumulation of extensive experience by surgeons have improved the feasibility and safety of laparoscopic surgery, and the applications for laparoscopic liver resection have therefore recently been greatly expanded[5-9]. Even major laparoscopic hepatectomy has been accepted to be a superior alternative to conventional open hepatectomy[10-13]. However, laparoscopic resection for hilar cholangiocarcinoma is still not universally accepted as an alternative approach to open surgery due to the difficulty in performing oncologic resection and the lack of consensus regarding the adequacy of this approach[14-16]. In the present paper, we review the current status of laparoscopic resection for hilar cholangiocarcinoma in the advanced laparoscopic era.
A computerized search of all the English literature cited in the PubMed database was performed using the search words “laparoscopy” and “hilar cholangiocarcinoma.” Relevant articles were retrieved and further references were obtained using manual cross-referencing.
Despite advances in preoperative imaging, a number of patients with hilar cholangiocarcinoma are found to have unresectable advanced tumors or occult metastases during surgical exploration. A few studies of staging laparoscopy in patients with hilar cholangiocarcinoma have reported an overall yield and accuracy of 14%-45% and 32%-71%, respectively (Table 1)[17-22]. The use of staging laparoscopy is recommended to avoid unnecessary laparotomy, particularly in patients with T2/3 disease on radiological imaging[17,18]. Although laparoscopic intraoperative ultrasonography is useful for detecting new liver nodules[23] and identifying locally advanced lesions, particularly when assessing vascular involvement, its accuracy is often limited by inflammation secondary to the placement of biliary stents[17]. In addition, the yield of laparoscopy for hilar cholangiocarcinoma has decreased due to improvements in the accuracy of imaging techniques, bringing into question its routine use in preoperative staging[21,24]. Clearly, prospective studies of larger series are needed to elucidate the appropriate indications and effects of staging laparoscopy in patients with hilar cholangiocarcinoma.
Portal vein embolization (PVE), a procedure devised by Makuuchi et al[25,26] and Kinoshita et al[27] is widely performed as a presurgical treatment in patients undergoing extended hepatectomy in order to minimize postoperative liver dysfunction. The use of staging laparoscopy prior to PVE is recommended to avoid unnecessary PVE[28]. Patients who are determined to be candidates for major hepatectomy at the time of staging laparoscopy, undergo PVE as an additional procedure at a later stage as PVE is usually performed through the ipsilateral or contralateral liver lobe via the transhepatic approach. The use of laparoscopic portal vein ligation (LPVL) can potentially avoid this additional procedure or unnecessary PVE[29,30]. Are et al[29] reported, according to the volumetric data for six patients treated with LPVL, a mean increase from 209.1 cc+/-97.76 to 495.83 cc+/-310.91 (an increase of 181.5%). Meanwhile, Ayiomamitis et al[30] reported that no intra- or postoperative complications in six patients, among whom all procedures were completed laparoscopically. In that study, repeat imaging of the liver resulted in a median (range) degree of hypertrophy of the future liver remnant of 24.5% (range, 20.7%-33.1%) in the six patients. In the hands of experienced laparoscopic hepatobiliary surgeons, LPVL is therefore considered to be a feasible and safe surgical modality in a select group of patients as an alternative to subsequent PVE.
In patients with hilar cholangiocarcinoma, the use of R1 resection is justified as a very efficient palliation[31]. Therefore, the laparoscopic approach may be accepted as palliative therapy, even if the surgical margins are not histologically clear. However, there are few reports regarding the use of laparoscopic palliation for hilar cholangiocarcinoma. Although the laparoscopic approach in biliary bypass surgery is safe and exhibits a high initial success rate, low reintervention rate, and low morbidity and mortality rates in patients with malignant distal biliary obstruction[32], non-surgical biliary stenting is the first choice for palliative biliary drainage in patients with hilar cholangiocarcinoma[31].
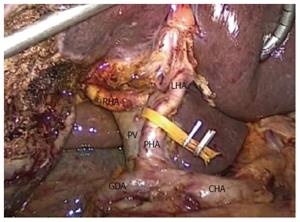
Although recent rapid developments in technological innovations, improvements in surgical techniques and the accumulation of extensive experience by surgeons have improved the feasibility and safety of laparoscopic major hepatectomy and extended the applications of lymphadenectomy (Figure 1), technical limitations and oncologic concerns have hindered the use of minimally invasive surgery in the treatment of hilar cholangiocarcinoma. Only a limited number of procedures have been reported (Table 2). Yu et al[33] performed laparoscopic local hilar resection and choledochojejunostomy in seven patients with Bismuth type I disease, laparoscopic combined partial liver resection and hepaticojejunostomy in five patients with type II disease, and palliative surgical bypass in two patients with more advanced hilar cholangiocarcinoma. The mean operative time and amount of blood loss were 305 min and 386 mL, respectively. Furthermore, the R0 resection rate was 100% and 60% in the patients with type I and II tumors, with in-hospital mortality and morbidity rates of 0% and 35.7%, respectively. Meanwhile, port-site recurrence was detected in two patients with type II tumors. The authors concluded that laparoscopy can be used as the first choice treatment for preoperative Bismuth type I cholangiocarcinoma. In contrast, Donati et al[34] reported that it was difficult to accept Yu’s assertion that laparoscopy is a potentially effective first choice therapy for preoperative Bismuth type I cholangiocarcinoma. In Yu’s article, no caudate resection was performed due to technical difficulties, thus resulting in a lack of radicality. In addition, it is very difficult for surgeons to assess the resectability and radicality (R0) of the hilar structures without using palpation to make important treatment decisions in patients with hilar cholangiocarcinoma. Therefore, the minimally invasive approach should be abandoned due to the lack of radicality and the unacceptable recurrence rate, including that of port-site recurrence. Gumbs et al[35] reported the use of a minimally invasive approach to treating extrapancreatic cholangiocarcinoma. In that study, five of 29 patients underwent laparoscopic resection for hilar cholangiocarcinoma. Three patients had Blumgart T1 lesions and two had T2 lesions, requiring concomitant laparoscopic right and left hepatectomy, respectively. One of the patients (20%) was converted to an open procedure due to concerns of portal vein involvement. The mean amount of blood loss was 240 mL (range, 0-400 mL) and the median length of stay was 15 d (range, 11-21 d). The patient with AJCC stage IV disease underwent R1 resection based on the final pathology, while all other patients received R0 resection. None of the five patients developed port-site recurrence. Machado et al[36] performed laparoscopic left hepatectomy with lymphadenectomy and extrahepatic bile duct resection in a 43-year-old female with left sided hilar cholangiocarcinoma. Biliary reconstruction was performed using the hybrid method. The operative time was 300 min with minimum blood loss, and the patient’s recovery was uneventful. While caudate resection was not performed, the patient received R0 resection and was found to be well without recurrence 18 mo after the surgery. The authors stressed that the use of a hybrid method for biliary reconstruction is needed. We performed pure laparoscopic hepato-pancreaticoduodenectomy, including left hepatectomy, caudate resection, and pylorus-preserving pancreaticoduodenectomy, in an 80-year-old female with hilar cholangiocarcinoma exhibiting widespread infiltration[37]. The procedure took 629 min, and the amount of operative bleeding was 200 mL. The patient was discharged on the 28th postoperative day due to the development of biliary leakage that later resolved spontaneously. A histological examination showed well differentiated tubular adenocarcinoma. Although the tumor had widely infiltrated to the extrahepatic bile duct, the surgical margins were histologically clear (R0 resection). No recurrence has been detected during the 24-mo follow-up.
| Ref. | n | Surgical approach | Surgical procedure BD, PR, HH, C | Operative Time (min) | Bleeding (g) | Complication | R0/R1 |
| Yu et al[33], 2011 | 14 | TL | 7, 5, 0, (-) | Mean 305 | Mean 386 | 35.7% | 10/2 |
| Gumbs et al[35], 2013 | 5 | TL | 0, 0, 5, NA | NA | Mean 240 | 0% | 4/1 |
| Machado et al[36], 2012 | 1 | H | 0, 0, 1, (-) | 300 | Minimum | 0% | 1/0 |
| Cho et al[37], 20131 | 1 | TL | TL 0, 0, 1, (+) | 629 | 200 | 100% | 1/0 |
| Giulianotti et al[38], 2010 | 1 | R | 0, 0, 1, (-) | 540 | 800 | 0% | 1/0 |
Giulianotti et al[38] reported performing robot-assisted laparoscopic resection for hilar cholangiocarcinoma using the da Vinci Robotic Surgical System (Intuitive Surgical, Sunnyvale, CA). Following percutaneous external biliary drainage and PVE, a 66-year-old male underwent extended right hepatectomy with left hepaticojejunostomy. The operative time and amount of blood loss were 540 min and 800 mL, respectively. One unit of red blood cells was transfused. Caudate resection was not performed. The histopathologic examination revealed a 22-mm moderately differentiated cholangiocarcinoma on the hilar bile duct confluence extending into the right hepatic duct without lymph node metastasis (T2N0). The surgical margins were free of tumor tissue. The patient’s postoperative course was uneventful, and was discharged on postoperative day 11.
The use of minimally invasive surgery for hilar cholangiocarcinoma is still not universally accepted as an alternative approach to open surgery. Aggressive surgery, including major hepatectomy with combined caudate resection, has become widely accepted as a standard treatment for hilar cholangiocarcinoma[39-43]. Better results have been obtained in terms of survival among patients with hilar cholangiocarcinoma by combining caudate resection. However, in previous reports of minimally invasive surgery for hilar cholangiocarcinoma, there were only a few descriptions concerning the decision to resect the caudate lobe. In experienced hands, laparoscopic caudate resection can be a safe and feasible procedure[37,44]. Despite concerns regarding technical feasibility and theoretical possibilities, the use of laparoscopic resection to treat hilar cholangiocarcinoma remains experimental. In fact, only 40%-50% of patients explored with curative intent are ultimately found to be resectable[45]. The intraoperative determination of resectability, which is usualy established by the surgeon following careful palpation and dissection of the liver hilum, is often crucial. Although the laparoscopic approach may favor an early safe discharge and prompt recovery in highly selected patients, the benefits of laparoscopic resection for hilar cholangiocarcinoma have yet to be conclusively proven, and carefully selecting patients is essential for successfully performing this procedure.
P- Reviewer: Guan YS, Klinge U S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535-543; discussion 544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 320] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, Katoh H. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 218] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 3. | Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, Yamasaki S, Takayama T, Makuuchi M. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005;137:396-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, Hayakawa N, Kanai M, Nimura Y. Complications of hepatectomy for hilar cholangiocarcinoma. World J Surg. 2001;25:1277-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009;250:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1249] [Cited by in RCA: 1155] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 6. | Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. Surgery. 1996;120:468-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 207] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 7. | Cho A, Asano T, Yamamoto H, Nagata M, Takiguchi N, Kainuma O, Souda H, Gunji H, Miyazaki A, Nojima H. Laparoscopy-assisted hepatic lobectomy using hilar Glissonean pedicle transection. Surg Endosc. 2007;21:1466-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Otsuka Y, Tsuchiya M, Maeda T, Katagiri T, Isii J, Tamura A, Yamazaki K, Kubota Y, Suzuki T, Suzuki T. Laparoscopic hepatectomy for liver tumors: proposals for standardization. J Hepatobiliary Pancreat Surg. 2009;16:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Nitta H, Sasaki A, Fujita T, Itabashi H, Hoshikawa K, Takahara T, Takahashi M, Nishizuka S, Wakabayashi G. Laparoscopy-assisted major liver resections employing a hanging technique: the original procedure. Ann Surg. 2010;251:450-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | O’Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg. 2004;8:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 177] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 11. | Gayet B, Cavaliere D, Vibert E, Perniceni T, Levard H, Denet C, Christidis C, Blain A, Mal F. Totally laparoscopic right hepatectomy. Am J Surg. 2007;194:685-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 141] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 12. | Dagher I, Di Giuro G, Lainas P, Franco D. Laparoscopic right hepatectomy with selective vascular exclusion. J Gastrointest Surg. 2009;13:148-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Cho A, Yamamoto H, Nagata M, Takiguchi N, Shimada H, Kainuma O, Souda H, Gunji H, Miyazaki A, Ikeda A. Laparoscopic major hepato-biliary-pancreatic surgery: formidable challenge to standardization. J Hepatobiliary Pancreat Surg. 2009;16:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Koffron AJ, Auffenberg G, Kung R, Abecassis M. Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg. 2007;246:385-392; discussion 392-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 15. | Bryant R, Laurent A, Tayar C, Cherqui D. Laparoscopic liver resection-understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg. 2009;250:103-111. [PubMed] |
| 16. | Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 875] [Article Influence: 54.7] [Reference Citation Analysis (0)] |
| 17. | Weber SM, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. Staging laparoscopy in patients with extrahepatic biliary carcinoma. Analysis of 100 patients. Ann Surg. 2002;235:392-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Tilleman EH, de Castro SM, Busch OR, Bemelman WA, van Gulik TM, Obertop H, Gouma DJ. Diagnostic laparoscopy and laparoscopic ultrasound for staging of patients with malignant proximal bile duct obstruction. J Gastrointest Surg. 2002;6:426-430; discussion 430-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Connor S, Barron E, Wigmore SJ, Madhavan KK, Parks RW, Garden OJ. The utility of laparoscopic assessment in the preoperative staging of suspected hilar cholangiocarcinoma. J Gastrointest Surg. 2005;9:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Goere D, Wagholikar GD, Pessaux P, Carrère N, Sibert A, Vilgrain V, Sauvanet A, Belghiti J. Utility of staging laparoscopy in subsets of biliary cancers: laparoscopy is a powerful diagnostic tool in patients with intrahepatic and gallbladder carcinoma. Surg Endosc. 2006;20:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 121] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Ruys AT, Busch OR, Gouma DJ, van Gulik TM. Staging laparoscopy for hilar cholangiocarcinoma: is it still worthwhile? Ann Surg Oncol. 2011;18:2647-2653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Barlow AD, Garcea G, Berry DP, Rajesh A, Patel R, Metcalfe MS, Dennison AR. Staging laparoscopy for hilar cholangiocarcinoma in 100 patients. Langenbecks Arch Surg. 2013;398:983-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Viganò L, Ferrero A, Amisano M, Russolillo N, Capussotti L. Comparison of laparoscopic and open intraoperative ultrasonography for staging liver tumours. Br J Surg. 2013;100:535-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Gaujoux S, Allen PJ. Role of staging laparoscopy in peri-pancreatic and hepatobiliary malignancy. World J Gastrointest Surg. 2010;2:283-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Makuuchi M, Takayasu K, Takuma T. Preoperative transcatheter embolization of the portal venous branch for patients receiving extended lobectomy due to the bile duct carcinoma [in Japanese]. J Jpn Soc Clin Surg. 1984;45:14-20. |
| 26. | Imamura H, Shimada R, Kubota M, Matsuyama Y, Nakayama A, Miyagawa S, Makuuchi M, Kawasaki S. Preoperative portal vein embolization: an audit of 84 patients. Hepatology. 1999;29:1099-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 249] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 27. | Kinoshita H, Sakai K, Hirohashi K, Igawa S, Yamasaki O, Kubo S. Preoperative portal vein embolization for hepatocellular carcinoma. World J Surg. 1986;10:803-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 310] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 28. | Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg. 2006;243:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 404] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 29. | Are C, Iacovitti S, Prete F, Crafa FM. Feasibility of laparoscopic portal vein ligation prior to major hepatectomy. HPB (Oxford). 2008;10:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Ayiomamitis GD, Low JK, Alkari B, Lee SH, Ammori BJ. Role of laparoscopic right portal vein ligation in planning staged or major liver resection. J Laparoendosc Adv Surg Tech A. 2009;19:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Witzigmann H, Lang H, Lauer H. Guidelines for palliative surgery of cholangiocarcinoma. HPB (Oxford). 2008;10:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Toumi Z, Aljarabah M, Ammori BJ. Role of the laparoscopic approach to biliary bypass for benign and malignant biliary diseases: a systematic review. Surg Endosc. 2011;25:2105-2116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Yu H, Wu SD, Chen DX, Zhu G. Laparoscopic resection of Bismuth type I and II hilar cholangiocarcinoma: an audit of 14 cases from two institutions. Dig Surg. 2011;28:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 34. | Donati M, Stavrou GA, Oldhafer KJ. Laparoscopic resections for hilar cholangiocarcinomas: a critical appraisal. Dig Surg. 2011;28:277-278; author reply 279-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 35. | Gumbs AA, Jarufe N, Gayet B. Minimally invasive approaches to extrapancreatic cholangiocarcinoma. Surg Endosc. 2013;27:406-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 36. | Machado MA, Makdissi FF, Surjan RC, Mochizuki M. Laparoscopic resection of hilar cholangiocarcinoma. J Laparoendosc Adv Surg Tech A. 2012;22:954-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 37. | Cho A, Yamamoto H, Kainuma O, Park SJ, Arimitsu H. Pure laparoscopic hepatopancreatoduodenectomy for cholangiocarcinoma. Videoscopy. 2013;23:1 Available from: http://online.liebertpub.com/doi/full/10.1089/vor.2012.0107. |
| 38. | Giulianotti PC, Sbrana F, Bianco FM, Addeo P. Robot-assisted laparoscopic extended right hepatectomy with biliary reconstruction. J Laparoendosc Adv Surg Tech A. 2010;20:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 39. | Hemming AW, Reed AI, Fujita S, Foley DP, Howard RJ. Surgical management of hilar cholangiocarcinoma. Ann Surg. 2005;241:693-699; discussion 699-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 250] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 40. | Sano T, Shimada K, Sakamoto Y, Yamamoto J, Yamasaki S, Kosuge T. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg. 2006;244:240-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 188] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 41. | Igami T, Nishio H, Ebata T, Yokoyama Y, Sugawara G, Nimura Y, Nagino M. Surgical treatment of hilar cholangiocarcinoma in the “new era”: the Nagoya University experience. J Hepatobiliary Pancreat Sci. 2010;17:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 142] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 42. | Unno M, Katayose Y, Rikiyama T, Yoshida H, Yamamoto K, Morikawa T, Hayashi H, Motoi F, Egawa S. Major hepatectomy for perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2010;17:463-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 43. | Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BS J, Youssef BA M, Klimstra D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507-517; discussion 517-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 973] [Cited by in RCA: 964] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 44. | Abu Hilal M, Badran A, Di Fabio F, Pearce NW. Pure laparoscopic en bloc left hemihepatectomy and caudate lobe resection in patients with intrahepatic cholangiocarcinoma. J Laparoendosc Adv Surg Tech A. 2011;21:845-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 45. | Ito F, Cho CS, Rikkers LF, Weber SM. Hilar cholangiocarcinoma: current management. Ann Surg. 2009;250:210-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 170] [Article Influence: 10.6] [Reference Citation Analysis (0)] |