Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14500
Revised: June 25, 2014
Accepted: July 24, 2014
Published online: October 21, 2014
Processing time: 342 Days and 2.2 Hours
We report the case of a 46-year-old woman who presented with chronic intermittent abdominal pain without jaundice; abdominal ultrasonography showed thickening of the gallbladder wall and dilatation of the bile duct. Endoscopic retrograde cholangiopancreaticography showed pancreatobiliary maljunction with proximal common bile duct dilatation. Pancreatobiliary maljunction was diagnosed. A computed tomography scan of the abdomen showed suspected gallbladder cancer and distal common bile duct obstruction. A pancreatic head mass was incidentally found intraoperative. Radical cholecystectomy with pancreatoduodenectomy was performed. The pathological report showed gallbladder cancer that was synchronous with pancreatic head cancer. In the pancreatobiliary maljunction with pancreatobiliary reflux condition, double primary cancer of the pancreatobiliary system should be awared.
Core tip: We reported a case of 46-year-old women presented with chronic intermittent abdominal pain without jaundice. Endoscopic retrograde cholangiopancreaticography revealed pancreatobiliary maljunction. Radical cholecystectomy with pancreatoduodenectomy was performed. Pathological report showed gallbladder cancer synchronous with pancreatic head cancer. In the pancreatobiliary maljunction with pancreatobiliary reflux condition double primary cancer of pancreatobiliary system should be kept in mind.
- Citation: Rungsakulkij N, Boonsakan P. Synchronous gallbladder and pancreatic cancer associated with pancreaticobiliary maljunction. World J Gastroenterol 2014; 20(39): 14500-14504
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14500.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14500
Gallbladder cancer is a rare malignancy in Thailand, but it is the most common biliary tract cancer. A report from the United States noted that there are 9000 new cases of gallbladder cancer per year[1]. The incidence is 1.2 cases/100000 population/year[2]. This cancer has a dismal prognosis because patients mostly have advanced-stage cancer when they are diagnosed. Early gallbladder cancer stages are rarely ever symptomatic. The most common presented symptom is abdominal pain[3]. Overall, 0.3%-1.0% of the patients are diagnosed from cholecystectomy specimens in other indications, especially from gallstones[4].
One of the known risk factors for gallbladder cancer is pancreaticobiliary maljunction, which is a congenital anomaly in which the pancreatic and bile ducts meet anatomically outside the duodenal wall, causing abnormal flow of the pancreatic juice and bile due to the absence of control of the sphincter of Oddi[5]. This rare condition is commonly reported in Asia and particularly in Japan. This condition causes bile duct irritation from pancreatic juice and dysplastic changes in the bile duct mucosa[6]. Pancreaticobiliary maljunction with or without bile duct dilatation is associated with carcinoma of the pancreaticobiliary tract.
Gallbladder cancer is commonly associated with bile duct cancer. However, synchronous gallbladder and pancreatic cancer is extremely rare. To date, we have reported only 3 cases of gallbladder cancer[7,8]. This is the first case report of this condition in Thailand.
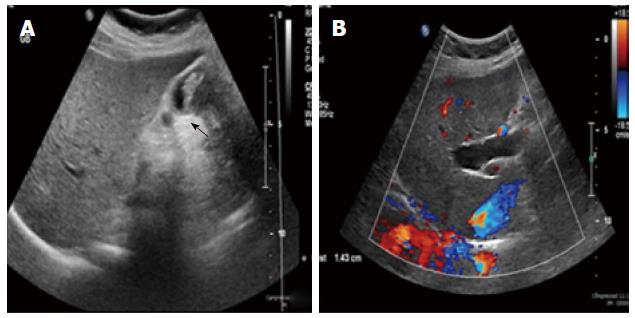
A 46-year-old Thai woman presented at the clinic with chronic intermittent abdominal pain for 2 mo, and ultrasound of her abdomen showed multiple hepatic cysts involving the right lobe and periportal areas with a relatively ill-defined mixed echoic lesion in the gallbladder lumen that was approximately 3.4 cm × 2.5 cm. She did not have a stone but had abnormal gallbladder wall thickening and bile duct dilatation (Figure 1A, B).
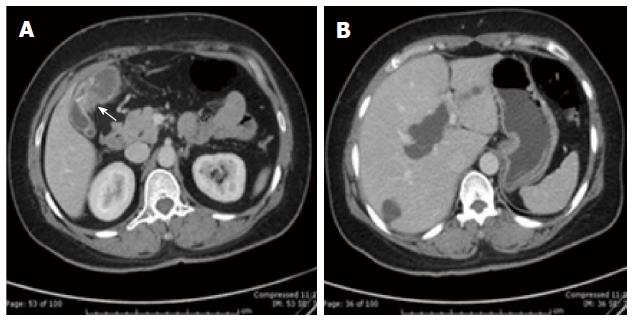
Her laboratory tests revealed a normal complete blood count and normal liver function with an alkaline phosphatase level of 71 U/L, a total bilirubin level of 0.5 mg/dL, a direct bilirubin level of 0.2 mg/dL, and an aspartate transaminase-alanine transaminase ratio of 22/31. She was sent for a computed tomography (CT) scan of her abdomen, which showed cystic dilatation of both the intrahepatic bile duct and proximal common bile duct with smooth narrowing of the proximal to mid common bile duct and no obvious masses. Asymmetric gallbladder wall thickening is observed at the transverse septum (Figure 2A, B).
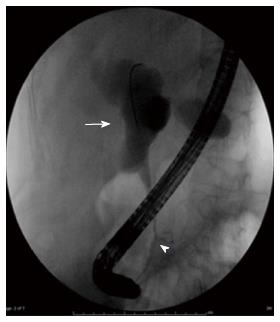
Then, endoscopic retrograde cholangiopancraticography was performed and revealed proximal common hepatic duct dilatation and long segment smooth stenosis of the distal common bile duct as well as abnormal insertion of the pancreatic duct into the common bile duct at approximately 3.0 cm above the ampulla. Sphincterotomy was performed, and a 7 Fr, 5-cm Amsterdam plastic biliary stent was inserted. Bile duct biopsy was performed and showed only inflammatory cells without evidence of malignancy. She suffered from severe pancreatitis after the endoscopic retrograde cholangiopancraticography that required percutaneous drainage for peripancreatic fluid collection (Figure 3).
Two months later, she underwent an operation for radical cholecystectomy with bile duct resection. Unfortunately, the intraoperative finding showed periportal lymphadenopathy and a hard nodule at the peripancreatic head area that suggested synchronous pancreatic head cancer, which was not visible in the preoperative CT scan. So, we decided to perform a radical cholecystectomy, including partial hepatectomy of liver segments V and IVb with pancreatoduodenectomy. The operation was uneventful. The total operation time was 8 h, and intraoperative blood loss was 1000 cc.
Postoperatively, she had pancreatic leakage and intraabdominal collection that required percutaneous drainage. Ultimately, she had to be re-operated on to remove the collection fluid after the percutaneous drainage failed. Finally, she was well when she was discharged from the hospital and did not have a drainage catheter.
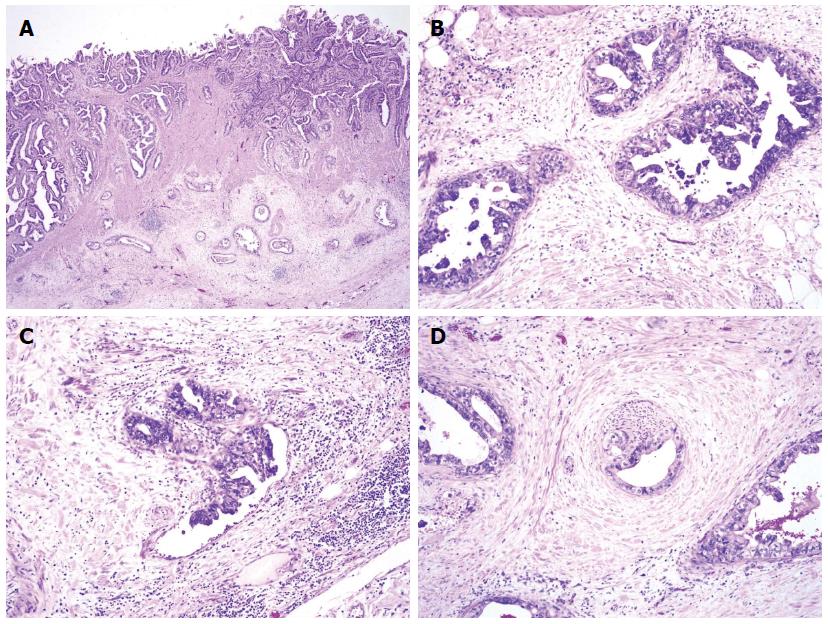
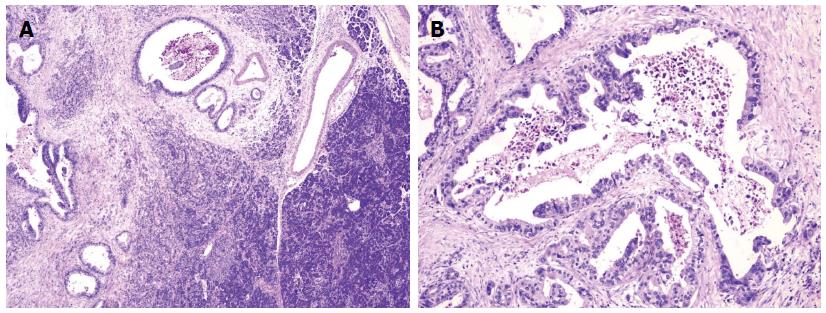
Pathological report of the gallbladder: Adenocarcinoma, well-differentiated, biliary type at the fundus, perforated serosa into the peri-gallbladder soft tissue, and presence of perineural invasion (pT3).
Pancreas: Adenocarcinoma, well-differentiated, ductal type, 2.8 cm in the greatest dimension, and presence of perineural and lymphovascular space invasions. Metastatic adenocarcinoma in all 6 peripancreatic lymph nodes and in one metastatic lymph node at the common hepatic duct (Figures 4 and 5). She received adjuvant chemotherapy with gemcitabine.
Approximately 10 mo postoperatively, she is still alive and has no tumor recurrence.
Pancreaticobiliary maljunction is more common in the Asian population and especially in Japan than in Western populations[9]. This condition includes abnormal connection of the pancreatic duct and common bile duct outside the duodenal wall. A report shows that there were 2561 cases of pancreaticobiliary maljunction in Japan between 1990 and 2007[10]. This condition is considered a risk factor for gallbladder cancer. There are many reports of synchronous and metachronous gallbladder cancer and other biliary tract cancers[5,11]. In this patient, cholangiogram from the endoscopic retrograde cholangiopancreaticography showed abnormal junction of the common bile duct and pancreatic duct and a long segment of common bile duct stricture from the pancreaticobiliary maljunction rather than distal common bile duct obstruction from pancreatic head cancer because the level of obstruction was high.
Synchronous gallbladder and pancreatic cancer is extremely rare. To the best of our knowledge, there have been only 3 cases reported worldwide in English and 5 cases reported in Japanese (Table 1)[7,8,12]. This is the first case reported from Thailand.
| Ref. | Gender/age | Diagnosis | Location(pancreas) | Operation | Survival (mo) | Bile duct dilation |
| Ueda et al[12], 1992 | Male/58 | Synchronous (GBC, PC, BDC) | Diffuse | Total pancreatectomy and extended cholecystectomy | Alive 30 | - |
| Minami et al[8], 2008 | Female/50 | Metachronous (GBC then PC) | Tail | Distal pancreatectomy | Alive 78 | + |
| Lahmar et al[7], 2010 | Female/68 | Metachronous (GBC then PC) | Head | Pancreatoduodenectomy | Alive > 12 | + |
| Our patient, 2013 | Female/46 | Synchronous (GBC, PC) | Head | Pancreatoduodenectomy and extended cholecystectomy | Alive > 12 | + |
Carcinogenesis of pancreatic cancer in this condition is unclear, but pancreaticobiliary maljunction can cause reciprocal reflux of pancreatic juices and bile due to the inability of the sphincter of Oddi to control normal flow. Pancreatobiliary reflux is confirmed with high levels of amylase and lipase in bile specimens from endoscopic retrograde cholangiopancraticography[5,6]. However, proof of bile in the pancreatic juice is difficult to obtain. In cases of acute pancreatitis, one hypothesis for the etiology explains the common channel hypothesis of distal common bile duct obstruction from gallstones and bile that is refluxed into the pancreatic duct causes acute pancreatitis[5,11,13].
Owing to reflux of pancreatic juice into the bile duct, there is a proliferation of the bile duct epithelium from normal epithelium to hyperplasia, metaplasia and dysplasia. Furthermore, there is evidence that gene mutations are associated with carcinogenesis, such as in the K-ras and p53 genes, which are involved in carcinogenesis of gallbladder cancer in this condition[14-16]. This is different from the general principle of carcinogenesis that arises from the adenoma-carcinoma sequence[5].
Although, the evidence of carcinogenesis of pancreatic carcinoma in pancreaticobiliary maljunction is still lacking, the reflux of bile into the pancreatic duct may cause chronic inflammation of the pancreas and may give rise to cancer of the pancreas[11].
The management of pancreaticobiliary maljunction with or without bile duct dilatation at that time of diagnosis and without cancer evidence involves cholecystectomy with or without bile duct resection and biliary reconstruction according to dilatation of the bile duct to divert flow and prevent future cancer development[5,17]. The cancer treatment at the time of diagnosis depends on the stage of gallbladder cancer and synchronous lesion.
In summary, a patient with pancreaticobiliary maljunction should be made aware of synchronous cancer of the pancreaticobiliary system.
A 46-year-old Thai woman presented at the clinic with chronic intermittent abdominal pain for 2 mo.
The Thai woman presented at the clinic with chronic intermittent abdominal pain for 2 mo and ultrasound of her abdomen showed multiple hepatic cysts involving the right lobe.
Her laboratory tests revealed a normal complete blood count and normal liver function with an alkaline phosphatase level of 71 U/L, a total bilirubin level of 0.5 mg/dL, a direct bilirubin level of 0.2 mg/dL, and an aspartate transaminase-alanine transaminase ratio of 22/31.
Ultrasound of her abdomen showed multiple hepatic cysts involving the right lobe and periportal areas with a relatively ill-defined mixed echoic lesion in the gallbladder lumen that was approximately 3.4 cm × 2.5 cm.
Pancreatobiliary reflux is confirmed with high levels of amylase and lipase in bile specimens from endoscopic retrograde cholangiopancraticography.
This manuscript presented the case of pancreaticobiliary maljunction complicated with synchronous gallbladder and pancreatic cancer. The present case report will provide useful information for the management of pancreaticobiliary maljunction.
P- Reviewer: Kawa S, Symeonidis NG, Triantopoulou C S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
| 1. | Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7953] [Cited by in RCA: 8102] [Article Influence: 506.4] [Reference Citation Analysis (2)] |
| 2. | Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer. 1995;75:171-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Batra Y, Pal S, Dutta U, Desai P, Garg PK, Makharia G, Ahuja V, Pande GK, Sahni P, Chattopadhyay TK. Gallbladder cancer in India: a dismal picture. J Gastroenterol Hepatol. 2005;20:309-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 80] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Hueman MT, Vollmer CM, Pawlik TM. Evolving treatment strategies for gallbladder cancer. Ann Surg Oncol. 2009;16:2101-2115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 130] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 5. | Kamisawa T, Ando H, Suyama M, Shimada M, Morine Y, Shimada H. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. 2012;47:731-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 134] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 6. | Kamisawa T, Okamoto A. Biliopancreatic and pancreatobiliary refluxes in cases with and without pancreaticobiliary maljunction: diagnosis and clinical implications. Digestion. 2006;73:228-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Lahmar A, Abid SB, Arfa MN, Bayar R, Khalfallah MT, Mzabi-Regaya S. Metachronous cancer of gallbladder and pancreas with pancreatobiliary maljunction. World J Gastrointest Surg. 2010;2:143-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Minami Y, Hasuike Y, Takeda Y, Tsujinaka T. Metachronous double cancer of the gallbladder and pancreas associated with pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg. 2008;15:330-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Roukounakis N, Manolakopoulos S, Tzourmakliotis D, Bethanis S, McCarty TM, Cuhn J. Biliary tract malignancy and abnormal pancreaticobiliary junction in a Western population. J Gastroenterol Hepatol. 2007;22:1949-1952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Morine Y, Shimada M, Takamatsu H, Araida T, Endo I, Kubota M, Toki A, Noda T, Matsumura T, Miyakawa S. Clinical features of pancreaticobiliary maljunction: update analysis of 2nd Japan-nationwide survey. J Hepatobiliary Pancreat Sci. 2013;20:472-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 108] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 11. | Funabiki T, Matsubara T, Miyakawa S, Ishihara S. Pancreaticobiliary maljunction and carcinogenesis to biliary and pancreatic malignancy. Langenbecks Arch Surg. 2009;394:159-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 12. | Ueda N, Nagakawa T, Ohta T, Kayahara M, Ueno K, Konishi I, Izumi R, Miyazaki I. Synchronous cancer of the biliary tract and pancreas associated with anomalous arrangement of the pancreaticobiliary ductal system. J Clin Gastroenterol. 1992;15:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Kamisawa T, Honda G, Kurata M, Tokura M, Tsuruta K. Pancreatobiliary disorders associated with pancreaticobiliary maljunction. Dig Surg. 2010;27:100-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Hanada K, Itoh M, Fujii K, Tsuchida A, Hirata M, Ishimaru S, Iwao T, Eguchi N, Kajiyama G. Pathology and cellular kinetics of gallbladder with an anomalous junction of the pancreaticobiliary duct. Am J Gastroenterol. 1996;91:1007-1011. [PubMed] |
| 15. | Matsubara T, Sakurai Y, Sasayama Y, Hori H, Ochiai M, Funabiki T, Matsumoto K, Hirono I. K-ras point mutations in cancerous and noncancerous biliary epithelium in patients with pancreaticobiliary maljunction. Cancer. 1996;77:1752-1757. [PubMed] |
| 16. | Noda Y, Fujita N, Kobayashi G, Ito K, Horaguchi J, Takasawa O, Obana T, Ishida K, Senoo S, Yonechi M. Histological study of gallbladder and bile duct epithelia in patients with anomalous arrangement of the pancreaticobiliary ductal system: comparison between those with and without a dilated common bile duct. J Gastroenterol. 2007;42:211-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Takeshita N, Ota T, Yamamoto M. Forty-year experience with flow-diversion surgery for patients with congenital choledochal cysts with pancreaticobiliary maljunction at a single institution. Ann Surg. 2011;254:1050-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |