Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14472
Revised: May 20, 2014
Accepted: June 26, 2014
Published online: October 21, 2014
Processing time: 200 Days and 23.3 Hours
AIM: To compare the current capsule and a new prototype at 2 and 4 frames-per-second, respectively, in terms of clinical and therapeutic impact.
METHODS: One hundred patients with an indication for capsule endoscopy were included in the study. All procedures were performed with the new device (SB24). After an exhaustive evaluation of the SB24 videos, they were then converted to “SB2-like” videos for their evaluation. Findings, frames per finding, and clinical and therapeutic impact derived from video visualization were analyzed. Kappa index for interobserver agreement and χ2 and Student’s t tests for qualitative/quantitative variables, respectively, were used. Values of P under 0.05 were considered statistically significant.
RESULTS: Eighty-nine out of 100 cases included in the study were ultimately included in the analysis. The SB24 videos detected the anatomical landmarks (Z-line and duodenal papilla) and lesions in more patients than the “SB2-like” videos. On the other hand, the SB24 videos detected more frames per landmark/lesion than the “SB2-like” videos. However, these differences were not statistically significant (P > 0.05). Both clinical and therapeutic impacts were similar between SB24 and “SB2-like” videos (K = 0.954). The time spent by readers was significantly higher for SB24 videos visualization (P < 0.05) than for “SB2-like” videos when all images captured by the capsule were considered. However, these differences become non-significant if we only take into account small bowel images (P > 0.05).
CONCLUSION: More frames-per-second detect more landmarks, lesions, and frames per landmark/lesion, but is time consuming and has a very low impact on clinical and therapeutic management.
Core tip: Capsule endoscopy has been demonstrated to be very accurate for small bowel lesions detection. Currently, most capsule endoscopes take 2 frames-per-second. Whether more frames-per-second could increase the diagnostic accuracy has not been previously investigated. The present study demonstrates that more frames per second is time consuming and has a very low impact in clinical and therapeutic management.
- Citation: Fernandez-Urien I, Carretero C, Borobio E, Borda A, Estevez E, Galter S, Gonzalez-Suarez B, Gonzalez B, Lujan M, Martinez JL, Martínez V, Menchén P, Navajas J, Pons V, Prieto C, Valle J. Capsule endoscopy capture rate: Has 4 frames-per-second any impact over 2 frames-per-second? World J Gastroenterol 2014; 20(39): 14472-14478
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14472.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14472
After 12 years of use, capsule endoscopy has demonstrated to be an accurate, painless, and safe procedure for patients with suspected small bowel diseases[1-3]. It has also been proven to be superior to other diagnostic modalities such as small bowel follow-through, CT-enterography, and push enteroscopy in obscure gastrointestinal bleeding, inflammatory bowel disease, and other clinical scenarios, and so is currently considered the new state-of-the-art procedure for small bowel visualization[4-8]. In fact, more than 2000000 capsule procedures have been performed worldwide (unpublished data). Due to its excellent acceptance by both patients and physicians, Given Imaging (Yoqneam, Israel) decided to introduce some modifications on the first generation of small bowel capsules (M2A) in order to improve its diagnostic accuracy. In 2004 the PillCam™ SB was developed, followed by the PillCam™ SB2 in 2007. However, capsule endoscopy is still not perfect and has some limitations. Firstly, some lesions are missed, probably due to the speed and/or orientation of the capsule in some segments of the gastrointestinal tract. In addition, some lesions are detected by the capsule in just one frame, leading to difficulties in their characterization that may have a negative impact on the final diagnosis. Despite a lack of available data to support it, one solution to these limitations could be increasing the frame rate detection of the capsule. Based on this hypothesis, the aims of this study were to evaluate the differences between a new prototype of capsule endoscopy that takes 4 images per second vs the current capsule endoscopy that takes 2 frames per second in terms of findings and diagnostic and therapeutic impact.
The present study was conducted at 10 Spanish institutions. Institutions and patients included per institution are shown in Table 1.
| Institution | n |
| Hospital de Navarra | 8 |
| Clinica Universidad de Navarra | 5 |
| Hospital Gregorio Marañon | 10 |
| Hospital Juan Canalejo | 10 |
| Hospital Puerta de Hierro | 9 |
| Hospital del Mar | 8 |
| Complejo Hospitalario de Toledo | 9 |
| Hospital La Fe | 10 |
| Hospital General de Valencia | 10 |
| Mutua de Tarrassa | 10 |
| Total | 89 |
One hundred (n = 100) consecutive patients who had indication and no contraindications for capsule endoscopy were prospectively included in the study. Before capsule ingestion all patients received a fully oral explanation of both the study and the capsule endoscopy procedure and were asked to sign an informed consent form. This study was designed under the principles of the Declaration of Helsinki and was approved by the institutional review boards.
After written consent to be included in the study, all patients swallowed the PillCam™ SB24 (Given Imaging Ltd, Yoqneam, Israel). The main difference between PillCam™ SB24 and PillCam™ SB2 is the rate of images per second taken by the capsule, 4 instead of 2, respectively. Other technical specifications of the PillCam™ SB24 are shown in Table 2. Capsule appearance, sensor arrays, data recorders, and software used in all procedures were exactly the same as those used in routine practice. The day before capsule ingestion, all patients were asked to have (1) a low fiber diet; (2) 2 liters of polyethylene glycol; and (3) a minimum of 8 hours fast prior to capsule ingestion. All patients then swallowed the capsule in the right supine position in order to obtain good images of the esophagus and Z-line. After capsule ingestion all patients were discharged from the hospital and asked to come back 10 h later. Laxatives and/or prokinetics were permitted, but the use of such products required that the study coordinator be notified. After downloading process had finished, 3 independent capsule endoscopy-experienced endoscopists reviewed the videos at 4 frames per second in order to detect all the lesions present in the videos. All readers were asked to review all the images of each one of the videos, including those obtained in the esophagus, stomach, and colon. An expert panel reviewed all findings and only clinically significant lesions were selected for the purpose of the study. Doubtful or minor lesions were not considered in the analysis. All videos were then labeled, recorded in portable hard discs, and sent to a technician in Israel who converted the videos from 4 frames per second to 2 frames per second to simulate conventional SB2 videos (“SB2-like videos”). Three independent readers unaware of the results derived from the first visualization reviewed all converted videos. Again, only clinically significant findings were considered and those doubtful findings were discussed by an expert panel. For each one of the videos reviewed the following variables were noted: patient baseline characteristics, procedure indication, Z-line, duodenal papilla and lesion visualization, number of frames per image/lesion selected, final diagnosis, need for more diagnostic procedures, final treatment, and reading times. The present study is a prospective, multicenter, and comparative study where quantitative data are shown as mean and range or standard deviation, with qualitative data as simple proportions. The interobserver agreement analysis was performed using the kappa index and the benchmarks considered by Fleiss[9] (< 0.40 poor agreement; 0.40-0.75 good agreement; > 0.75 excellent agreement). Comparative analysis was performed using the χ2 test for qualitative variables and the Student′s t test for quantitative variables. Values of P under 0.05 were considered statistically significant.
| Physical dimensions | 26 mm × 11 mm |
| Weight | 2.89 ± 0.15 g |
| Number of imaging heads | 1 |
| Imager type | CMOS |
| Image capture rate | 4 frames per second |
| Optical illumination | 4 white light emitting diodes with ALC |
| Field of view | 156° - working distance of 4.5 mm |
| Depth of field | 0-30 mm |
| Mucosa area images at 4.5 mm | Approximately 1100 mm2 |
| Magnification | 1.8 |
| Min. detectable object size | 0.1 mm |
| Min. operation time | 7 h and 58 min |
| Max. operation time | 9:00 h |
| Shelf life | 10 mo after manufacturing date |
| Transmitter frequency | 434.1 MHz |
| Battery type | Silver oxide, non-toxic |
| Storage temperature | 0°-30° |
| Activation | Magnetic, automatic from blister |
A total of 100 procedures were performed but only 89 (89%) were included in the analysis. Eleven procedures (11%) were withdrawn due to technical issues and protocol violations: one capsule was retained in the stomach, 6 SB24 videos were not converted to “SB2-like” videos because the raw data were not correctly downloaded and 4 patients did not ingested the PEG solution.
The mean age of patients included in the study was 51.6 years (range 21-84), with 35 (39.3%) males and 54 (60.7%) females. Procedure indications were as follows: obscure gastrointestinal bleeding in 55 (61.8%), inflammatory bowel disease in 19 (21.3%), malabsorption in 5 (5.6%), tumors in 5 (5.6%), and abdominal pain in 5 (5.6%) patients. The capsule was ingested by the patients in the right supine position in 74 (83%) of the cases and the cecum was achieved in 80 patients (90%).
Anatomy: The Z-line and duodenal papilla were detected in 53/89 (59.5%) and 7/89 (7.8%) patients and in 616 (11.6 frames per positive procedure on average) and 35 frames (5 frames per positive procedure on average), respectively.
A total of 257 different lesions and 3291 pathologic frames were detected. The distribution of lesions and pathologic frames dependent on their localization are shown in Table 3.
| Lesions | Frames | |
| Total | Total | |
| Esophagus | 17 (6.6) | 132 (4) |
| Stomach | 30 (11.6) | 617 (19.1) |
| Small bowel | 193 (75) | 2227 (69) |
| Colon | 17 (6.6) | 249 (7.7) |
| Total | 257 (100) | 3225 (100) |
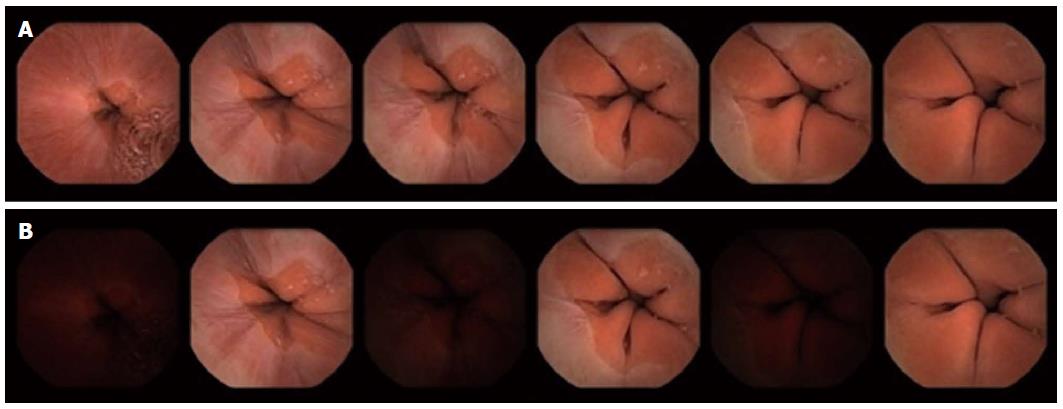
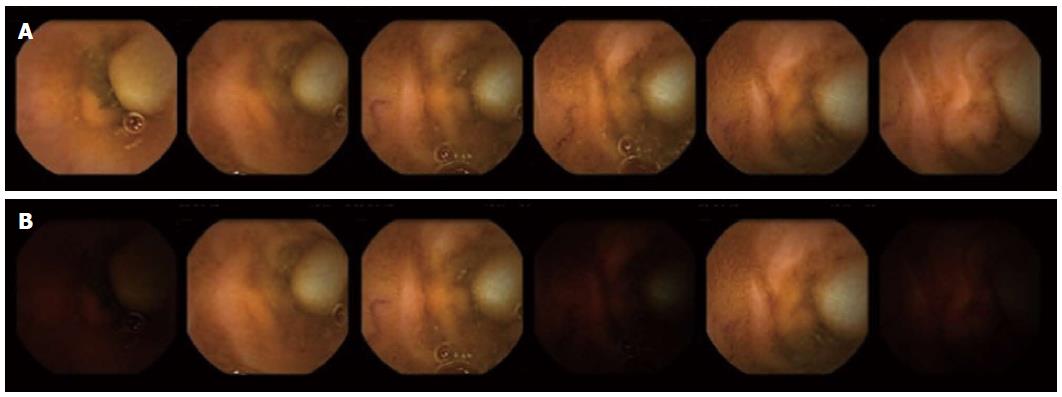
Comparative analysis has been summarized in Table 4, Table 5, Table 6, Table 7, Table 8, Table 9 and illustrated in Figures 1 and 2.
| SB24 patients | “SB2-like” patients | P value | K value | |
| Z-line | 53 (59.5) | 45 (50.6) | NS | 0.820 |
| Papilla | 7 (7.9) | 6 (6.7) | NS | 0.917 |
| SB24 | "SB2-like" | P value | |||
| Frames | Mean ± SD | Frames | Mean ± SD | ||
| Z-line | 616 | 11.6 ± 20.4 | 391 | 8.6 ± 10.6 | NS |
| Papilla | 35 | 5.0 ± 2.0 | 15 | 2.5 ± 1.4 | < 0.05 |
| Quality1 | SB24 | “SB2-like” | P value |
| Mean ± SD | Mean ± SD | ||
| 91.94 ± 21.82 | 88.01 ± 34.87 | NS |
| SB24 | “SB2-like” | P value | |||
| Lesions | Mean ± SD | Lesions | Mean ± SD | ||
| Esophagus | 17 | 0.2 ± 0.4 | 14 | 0.1 ± 0.4 | NS |
| Stomach | 30 | 0.3 ± 0.8 | 30 | 0.3 ± 0.8 | NS |
| Small bowel | 193 | 2.2 ± 3.1 | 183 | 2.1 ± 2.8 | NS |
| Colon | 17 | 0.2 ± 0.6 | 17 | 0.2 ± 0.6 | NS |
| Total | 257 | 2.9 ± 3.8 | 244 | 2.7 ± 3.5 | NS |
| SB24 | “SB2-like” | P value | |||
| Frames | Mean ± SD | Frames | Mean ± SD | ||
| Esophagus | 132 | 7.7 ± 9.0 | 91 | 6.5 ± 8.7 | NS |
| Stomach | 617 | 20.5 ± 34.2 | 403 | 13.4 ± 25.8 | NS |
| Small Bowel | 2227 | 11.5 ± 28.1 | 1490 | 8.1 ± 18.1 | NS |
| Colon | 249 | 14.6 ± 18.2 | 155 | 9.1 ± 12.4 | NS |
| Total | 3225 | 12.8 ± 15.2 | 2139 | 8.7 ± 15.6 | NS |
Anatomy: The SB24 detected both Z-line and duodenal papilla in more patients than the “SB2-like”: 53 (59.5%) vs 45 (50.6%) and 7 (7.9%) vs 6 (6.7%) out of 89 patients included in the analysis, respectively. However, these differences were not statistically significant (P > 0.05). Moreover, there was an excellent agreement between SB24 and “SB2-like” in selecting those patients with at least one image of the Z-line and duodenal papilla (kappa index 0.820 and 0.917, respectively). There were no cases with positive findings on “SB2-like” videos and negative on SB24. Furthermore, the SB24 captured more frames of both Z-line (overall 616 and average 11.6 ± 20.4 for SB24vs overall 391 and average 8.6 ± 10.6 for “SB2-like”; P > 0.05) and duodenal papilla (overall 35 and average 5.0 ± 2.0 for SB24vs overall 15 and average 2.5 ± 1.4 for “SB2-like”; P < 0.05). Focusing on the quality of the images detected of Z-line (percent of Z-line detected), there were not significant differences between the two capsules (P > 0.05).
Per-patient analysis: Almost all patients with lesions, despite their location, were detected by both methods, resulting in no significant differences between them (P > 0.05). Moreover there was an excellent agreement between the videos for detecting patients with lesions (kappa index from 0.9 to 1.0; excellent agreement). There were no positive cases in “SB2-like” videos that were negative in SB24 videos.
Per-lesion analysis: Most of the lesions detected in the videos at 4 frames per second were also detected in the “SB2-like” videos, resulting in no statistically significant differences. Moreover, there were no cases with positive findings on “SB2-like” videos and negative on SB24. In fact, the SB24 detected 257 lesions (2.9 ± 3.8 on average per patient) and the “SB2-like” 244 (2.7 ± 3.5 on average per patient). When only considering the esophagus and small bowel, the SB24 videos detected more lesions compared to “SB2-like” (17 vs 14 in the esophagus and 193 vs 183 in the small bowel). Furthermore, the SB24 captured more frames of each lesion despite its localization, but these differences were not statistically significant (P > 0.05). All lesions (100%) lost in the “SB2-like” videos were detected in 1-2 frames in the SB24 videos. There were no lesions detected in more than 2 frames in SB24 videos that were lost in “SB2-like” videos.
The time spent for video reading was higher for the SB24 videos. However, this differences were significant only in those cases where all the images (from mouth to the last procedure image) where reviewed (average time of 39.6 ± 15.8 for SB24vs 29.5 ± 12.4 for SB2-like; P < 0.05).
When clinical and therapeutic impact was analyzed, it was seen that the agreement between SB24 and “SB2-like” videos was excellent (K = 0.954). Only in one case (1.12%) did the use of SB24 instead of SB2 lead to a different diagnosis and management, as there was a single frame showing Barrett’s esophagus that was missed in the “SB2-like video”.
Capsule endoscopy has opened up a new era in small bowel examination. Its diagnostic accuracy is very high, particularly in those patients with obscure gastrointestinal bleeding and inflammatory bowel disease, and is currently the first line diagnostic tool for small bowel suspected diseases[1-8]. Despite its excellent performance, capsule endoscopy has some limitations. On one hand, it has been demonstrated that some lesions can be missed by capsule endoscopy[10-12]. Although these false negatives could be related to non-accurate readings, the presence of blind areas and fast transit times in some segments could be the main reasons in most cases. On the other hand, it is also known that false positive lesions could be detected during small bowel capsule endoscopy leading to unnecessary diagnostic and therapeutic procedures. Most false positives are due to doubtful images detected in a low number of frames, or even in just one frame. During most capsule endoscopy training programs, one general rule that is usually given to trainees is to avoid diagnoses based only on one frame. In these situations they are usually asked to use the mouse scroll in order to find more frames of the suspected image in order to make a more accurate diagnosis. However, sometimes this is not possible due to there being only one frame of the suspected lesion and the diagnosis has to be based on that. So, it makes sense that the number of frames of suspicious lesions is directly related to correct characterizations and diagnoses. Currently, there are 5 capsule endoscopes in the market: PillCam SB2 (Given Imaging Ltd., Yoqneam, Israel), EndoCapsule (Olympus Medical Systems Corp., Tokyo, Japan), OMOM (Jianshan Science and Technology Group Co., Ltd., Chongqing, China) small bowel capsule systems which capture 2 frames per second, Mirocam small bowel capsule system (Intromedic Ltd, Seoul, Korea) that can capture 3 frames per second, and the recently developed CapsoCam capsule (CapsoVision Inc., Silicon Valley, CA, United States) that captures 3-5 frames per second. Moreover, since 2007 there have been capsules designed for the study of the colon that have 2 optical heads taking 4 frames per second (PillCam™ COLON1; Given Imaging Ltd, Yoqneam, Israel), and recently from 4 to 35 frames per second (PillCam™ COLON2; Given Imaging Ltd, Yoqneam, Israel). It is well known that some physicians use the PillCam™ COLON/2 for the study of the small bowel, considering the higher number of frames per second captured. However, it is not still clear if it increases diagnostic accuracy[13,14]. Previous reports comparing the Mirocam and the PillCam SB capsules showed no benefits from 3 over 2 frames per second capture rate in terms of diagnostic accuracy[15,16]. To our knowledge, the present study is the first to compare the clinical and diagnostic impact of more frames per second capture rate using the same capsule endoscope. The present study compares a new prototype of small bowel capsule endoscopy by Given Imaging that takes 4 frames per second. One of the positive aspects of this study is that we could compare the number of frames of the same lesions captured in both videos. We did not perform examinations of each capsule in each patient, instead performing all procedures with the new prototype of the capsule (4 frames per second), with the videos then being sent to Given Imaging in order to be converted into conventional videos at 2 frames per second (“SB2-like”). We were then able to compare anatomic landmark visualization, lesions detection, and frames per lesion in the same images and in both 4 frames and 2 frames per second videos. The present study focused mainly on lesions but also on anatomic landmarks because, in daily practice, it is quite frequent to find lesions there, including GERD lesions, Barrett esophagus, hiatal hernia, and tumors[17-19]. In order to obtain the best images of the esophagus, all patients swallowed the capsule in the right supine position, as this has been demonstrated to be the best approach for this purpose[20,21]. Moreover, this study analyzed not only lesions located in the small bowel, but also in the esophagus, stomach, and colon. For that purpose, all patients underwent PEG administration prior to capsule ingestion and all readers were requested to read all the images contained in the videos from mouth to last video image. We did not find significant differences in the detection of anatomy and lesions between the two capsules. SB24 and “SB2-like” detected anatomical landmarks in a very similar number of patients. However, there were still differences in both number of frames per landmark and quality of images detected. In fact, the 4 frames per second capsule detected more frames of the Z-line and duodenal papilla, but these differences were not significant. On the other hand, the same situation was observed when lesions were analyzed. Again, the SB24 detected more patients with lesions and more frames per lesion, especially in those located in the small bowel. However, these differences were not statistically significant. All lesions lost in “SB2-like” videos were detected in 1-2 frames, which means that the benefits of 4 frames per second over 2 frames per second could be expected when small, isolated, and esophageal/duodenal (fast transits) lesions are present. Obviously, our analysis resulted in no great differences in clinical and therapeutic impact except for one patient where the SB24 detected a Barrett′s esophagus that was missed by the “SB2-like”. In fact, this lesion was only visualized in just one frame. Once the statistical analysis was completed it seemed that, although no significant differences between the capsules were found, the tendency (especially for small bowel lesions) was to reach statistically significant differences. This could be the main limitation of the study. This was a pilot study were, initially, 100 patients were included, but this sample size was not enough to reach statistical significant differences. Future studies should use larger populations in order to obtain solid conclusions of the benefit of using more frames per second in small bowel examinations. The use of more frames per second means more images to review and longer reading times. The present study demonstrates that the reading times were significantly longer when the videos were reviewed from mouth to the last video image. There were no significant differences when only the small bowel was read. Reading times are an important issue in capsule endoscopy. On one hand, physicians are usually working under pressure in public hospitals and there is no chance for time-consuming procedures. On the other hand, although it is not published, the time spent in video reading is inversely proportional to reader accuracy. It may be helpful to modify the software in order to delete similar images and consequently, decrease reading and video downloading times.
In summary, this study demonstrates that there is no clinical or therapeutic impact derived from the use of a 4-frame per second capsule over the conventional one. However, it is also shown that more frames per second, which takes more time to process for the readers, gives more images of the same lesion/image, especially in the small bowel, and this could be helpful in some situations. Future studies in larger series should be done in order to confirm our results.
Most capsule endoscopes take 2 frames per second during approximately 8-10 h. However, lesions are still missed.
Whether more frames-per-second could increase the diagnostic accuracy of capsule endoscopy has not been previously investigated.
The clinical and therapeutic impact of 4 frames-per-second over 2 frames-per-second is very low. Moreover, video reading takes more time as the frames-per-second increases.
Although more frames-per-second should not be recommended routinely, it could be helpful in fast transit segments such as the esophagus or duodenum.
Frames-per-second is the term used to describe the number of images taken by capsule endoscopy. Most small bowel capsule endoscopes take 2 images-per-second (i.e., 2 frames-per-second) during 8-10 h.
This article presents interesting data concerning an old issue about the need for more frames-per-second during small bowel capsule endoscopy.
P- Reviewer: Aurello P, Dietrich CF S- Editor: Qi Y L- Editor: Rutherford A E- Editor: Zhang DN
| 1. | Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405:417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1994] [Cited by in RCA: 1386] [Article Influence: 55.4] [Reference Citation Analysis (1)] |
| 2. | Appleyard M, Glukhovsky A, Swain P. Wireless-capsule diagnostic endoscopy for recurrent small-bowel bleeding. N Engl J Med. 2001;344:232-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 167] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: Results of a pilot study. Gastrointest Endosc. 2002;56:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 326] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 4. | Appleyard M, Fireman Z, Glukhovsky A, Jacob H, Shreiver R, Kadirkamanathan S, Lavy A, Lewkowicz S, Scapa E, Shofti R. A randomized trial comparing wireless capsule endoscopy with push enteroscopy for the detection of small-bowel lesions. Gastroenterology. 2000;119:1431-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 247] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 5. | Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi A, Marano P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology. 2002;123:999-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 565] [Cited by in RCA: 517] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 6. | Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34:685-689. [PubMed] |
| 7. | Eliakim R, Fischer D, Suissa A, Yassin K, Katz D, Guttman N, Migdal M. Wireless capsule video endoscopy is a superior diagnostic tool in comparison to barium follow-through and computerized tomography in patients with suspected Crohn’s disease. Eur J Gastroenterol Hepatol. 2003;15:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 169] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Carretero C, Fernandez-Urien I, Betes M, Muñoz-Navas M. Role of videocapsule endoscopy for gastrointestinal bleeding. World J Gastroenterol. 2008;14:5261-5264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Fleiss JL. Statistical methods for rates and proportions. 2nd ed. New York: John Wiley and Sons 1981; 225-332. |
| 10. | Chong AK, Chin BW, Meredith CG. Clinically significant small-bowel pathology identified by double-balloon enteroscopy but missed by capsule endoscopy. Gastrointest Endosc. 2006;64:445-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 97] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Postgate A, Despott E, Burling D, Gupta A, Phillips R, O’Beirne J, Patch D, Fraser C. Significant small-bowel lesions detected by alternative diagnostic modalities after negative capsule endoscopy. Gastrointest Endosc. 2008;68:1209-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Ross A, Mehdizadeh S, Tokar J, Leighton JA, Kamal A, Chen A, Schembre D, Chen G, Binmoeller K, Kozarek R. Double balloon enteroscopy detects small bowel mass lesions missed by capsule endoscopy. Dig Dis Sci. 2008;53:2140-2143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Karagiannis S, Dücker C, Dautel P, Strubenhoff J, Faiss S. Identification of the duodenal papilla by colon capsule endoscope. Z Gastroenterol. 2010;48:753-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Mateescu BR, Bengus A, Marinescu M, Staniceanu F, Micu G, Negreanu L. First Pillcam Colon 2 capsule images of Whipple’s disease: Case report and review of the literature. World J Gastrointest Endosc. 2012;4:575-578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Pioche M, Gaudin JL, Filoche B, Jacob P, Lamouliatte H, Lapalus MG, Duburque C, Chaput U, Ben Soussan E, Daudet J. Prospective, randomized comparison of two small-bowel capsule endoscopy systems in patients with obscure GI bleeding. Gastrointest Endosc. 2011;73:1181-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Choi EH, Mergener K, Semrad C, Fisher L, Cave DR, Dodig M, Burke C, Leighton JA, Kastenberg D, Simpson P. A multicenter, prospective, randomized comparison of a novel signal transmission capsule endoscope to an existing capsule endoscope. Gastrointest Endosc. 2013;78:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Schäfer C, Göke B. Do we underestimate capsule endoscopy in the upper gastrointestinal tract? Digestion. 2005;72:239-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Clarke JO, Giday SA, Magno P, Shin EJ, Buscaglia JM, Jagannath SB, Mullin GE. How good is capsule endoscopy for detection of periampullary lesions? Results of a tertiary-referral center. Gastrointest Endosc. 2008;68:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Borobio E, Fernández-Urién I, Elizalde I, Jiménez Pérez FJ. Hiatal hernia and lesions of gastroesophageal reflux disease diagnosed by capsule endoscopy. Rev Esp Enferm Dig. 2009;101:355-356. [PubMed] |
| 20. | Gralnek IM, Rabinovitz R, Afik D, Eliakim R. A simplified ingestion procedure for esophageal capsule endoscopy: initial evaluation in healthy volunteers. Endoscopy. 2006;38:913-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Fernandez-Urien I, Borobio E, Elizalde I, Irisarri R, Vila JJ, Urman JM, Jimenez J. Z-line examination by the PillCam SB: prospective comparison of three ingestion protocols. World J Gastroenterol. 2010;16:63-68. [PubMed] |