Published online Oct 14, 2014. doi: 10.3748/wjg.v20.i38.14068
Revised: May 7, 2014
Accepted: June 13, 2014
Published online: October 14, 2014
Processing time: 231 Days and 17.2 Hours
Gallbladder torsion is a rare, acute abdominal disease. It was first reported by Wendell in 1898. Since then, only 500 cases have been reported. Gallbladder torsion occurs in all age groups, although it usually appears in the latter stages of life. The occurrence ratio between women and men is 3:1. Most cases are diagnosed during surgery. The main treatment is surgical detorsion and cholecystectomy. Despite progress in radiologic imaging diagnosis, it is not easy to obtain a precise preoperative diagnosis of gallbladder torsion. In previous reports, only 9.8% of all gallbladder torsion cases were diagnosed preoperatively. We present a case of acute body-neck gallbladder torsion in an elderly man, and we review the radiologic findings of magnetic resonance imaging, computed tomography, and ultrasonography. The radiologic findings in the present case were helpful in obtaining a preoperative diagnosis of gallbladder torsion. The diagnosis was confirmed by T2-weighted magnetic resonance images, which showed an intra-gallbladder segment located between the body and neck of the gallbladder, with a notable crease within this segment.
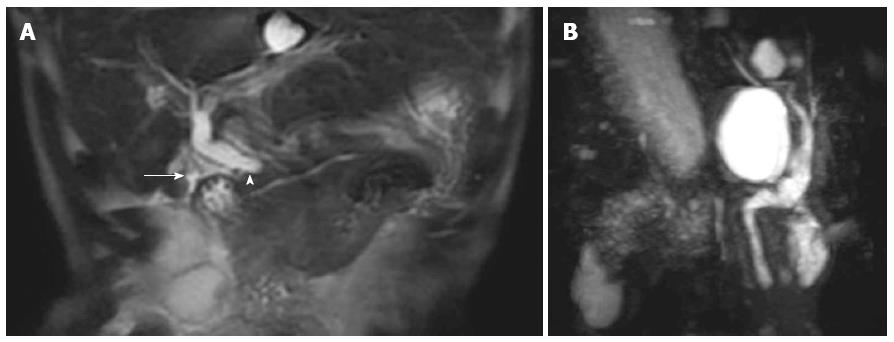
Core tip: Torsion of the gallbladder is a rare condition and is very difficult to diagnose preoperatively, despite advances in diagnostic imaging. This diagnosis should be considered in all elderly patients presenting with acute or non-resolving symptoms and signs suggestive of cholecystitis, particularly in the absence of gallstones. Early diagnostic imaging and prompt cholecystectomy are crucial. In this case of gross type 1 floating gallbladder, T2-weighted magnetic resonance imaging showed an intra-gallbladder segment located between the body and neck of the gallbladder. Magnetic resonance cholangiopancreatography indicated V-shaped distortion of the extrahepatic bile duct and a tapered cyst duct.
- Citation: Pu TW, Fu CY, Lu HE, Cheng WT. Complete body-neck torsion of the gallbladder: A case report. World J Gastroenterol 2014; 20(38): 14068-14072
- URL: https://www.wjgnet.com/1007-9327/full/v20/i38/14068.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i38.14068
Gallbladder torsion was first reported by Wendell in 1898[1]. Since then, only 500 cases have been reported[2-6]. Gallbladder torsion is a rare, extremely acute abdominal disease, and it is treated by emergency surgery. Gallbladder torsion occurs in all age groups, although it usually appears in the later stages of life[7]. The occurrence ratio between women and men is 3:1[6,8-11]. This diagnosis should be considered in all elderly patients presenting with acute or non-resolving symptoms and signs suggestive of cholecystitis, particularly in the absence of gallstones. The disease leads to obstruction of biliary drainage and blood flow. Therefore, a delay in diagnosis and treatment can be life threatening. An accurate preoperative diagnosis of gallbladder torsion has only rarely been obtained[2-4,12,13]. Laboratory evaluations often provide nonspecific results. White blood cell count and C-reactive protein levels are frequently elevated. However, the results of liver function tests and biliary enzymes are often normal[2,4,14].
We report here a case of gross type 1 floating gallbladder, in which T2-weighted magnetic resonance imaging (MRI) showed an intra-gallbladder segment located between the body and neck of the gallbladder. The results of magnetic resonance cholangiopancreatography (MRCP) indicated V-shaped distortion of the extrahepatic bile duct and a tapered cyst duct.
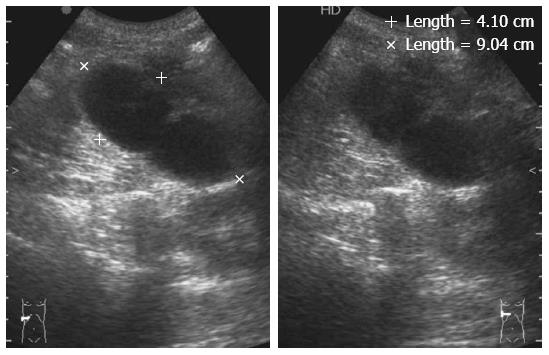
A 73-year-old man arrived in our hospital’s emergency department with severe pain in the upper-right quadrant. He reported that the pain had persisted progressively since the previous day. He had no history of previous abdominal surgery or trauma. Upon physical examination, his body temperature and vital signs were all within the normal ranges. An abdominal examination revealed no palpable mass or Murphy’s sign. Laboratory data indicated that his white cell count was 5.25 × 103/μL, with a neutrophil count of 53.7% and a lymphocyte count of 36.8%. His C-reactive protein level was < 0.03 mg/dL. The results of liver function tests were normal, including aspartate aminotransferase, alanine aminotransferase, and total bilirubin with values of 16 U/L, 10 U/L, and 0.75 mg/dL, respectively. Abdominal ultrasonography indicated thickening of the gallbladder wall. However, gallstones were not present, and there was no intra- or extrahepatic biliary duct dilatation (Figure 1).
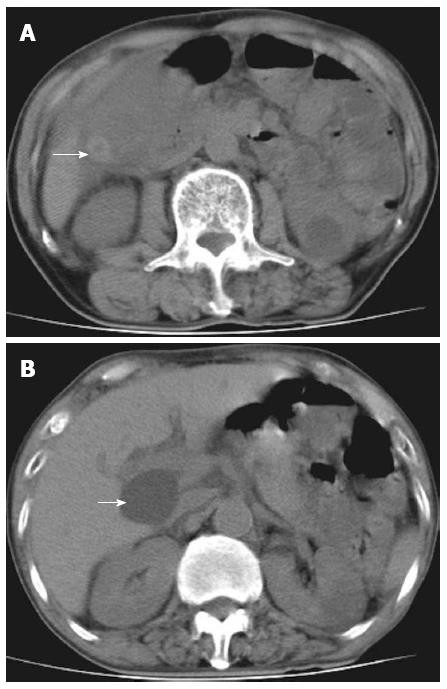
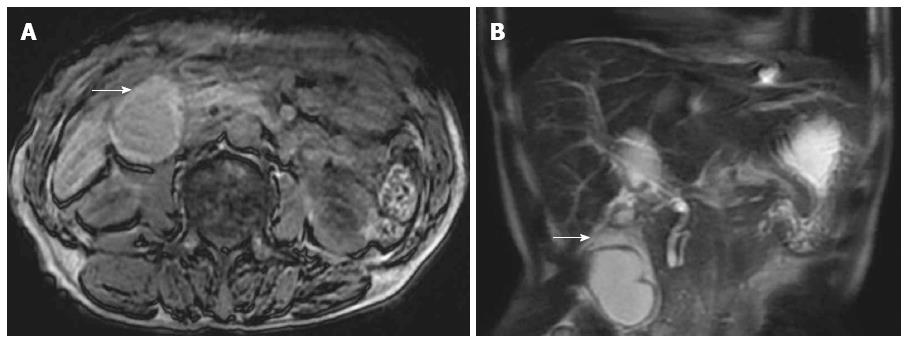
Computed tomography (CT) of the abdomen without contrast revealed a hyperdense lesion (Figure 2A) and a cyst in the hilar region (Figure 2B). Because of suspected intra-gallbladder hemorrhage and considering that a choledochal cyst could not be excluded, we conducted an MRI examination of the abdomen and MRCP. T1-weighted images revealed gallbladder wall thickening (Figure 3A). T2-weighted images showed an intra-gallbladder crease between the body and neck of the gallbladder.
These results indicated a twisting at the junction of the gallbladder body and neck (Figure 3B). The MRCP results indicated V-shaped distortion of the extrahepatic bile duct and a tapered cyst duct (Figure 4A). A choledochal cyst was excluded because the hepatic cyst was not connected to the biliary tract, as revealed by further examination (Figure 4B).
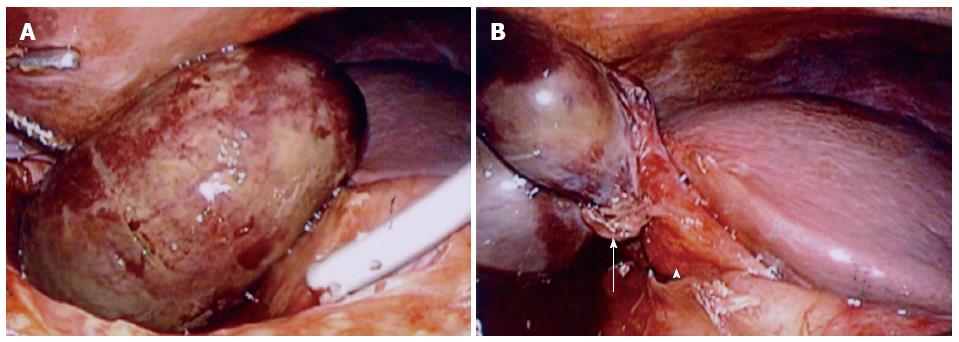
These physical and radiographic findings indicated the presence of gallbladder torsion. We then performed laparoscopy to diagnose and treat the gallbladder torsion. Closer inspection showed that the gallbladder was not adhered to the liver bed and had rotated approximately 180° in the clockwise direction (Figure 5). After detorsion, cholecystectomy was performed. Histological examination of the specimen revealed acute gangrenous cholecystitis. The patient recovered without incident and was discharged from the hospital within 1 wk.
Gallbladder torsion occurs when the gallbladder rotates within its mesentery. This rotation follows the axis of the cystic duct and cystic artery, resulting in a compromised blood supply and obstructed biliary drainage. A preoperative diagnosis is unlikely, typically necessitating prompt surgery to avoid death, because a high mortality rate is associated with gallbladder torsion. This high mortality rate is increased because of concomitant gangrene and perforation[4-6].
Torsion is believed to occur more often in the elderly because of the loss of visceral fat and elasticity of the viscera. With aging, the gallbladder becomes more predisposed to hang free and undergo torsion. The torsion can be complete or incomplete. In complete torsion, the rotation is greater than 180°, whereas in incomplete torsion, the rotation is less than 180°[4,5,7,9,11,12].
Several signs accompany the preoperative diagnosis of gallbladder torsion by MRCP. First, because of cystic duct traction, V-shaped distortion of extrahepatic bile might be noted[7,10]. Second, twisting interruption and tapering of the cystic duct might be observed. Third, the gallbladder might deviate to the midline, with distention and enlargement. Fourth, the gallbladder, extrahepatic bile ducts, and cystic duct might display different intensities[6,15].
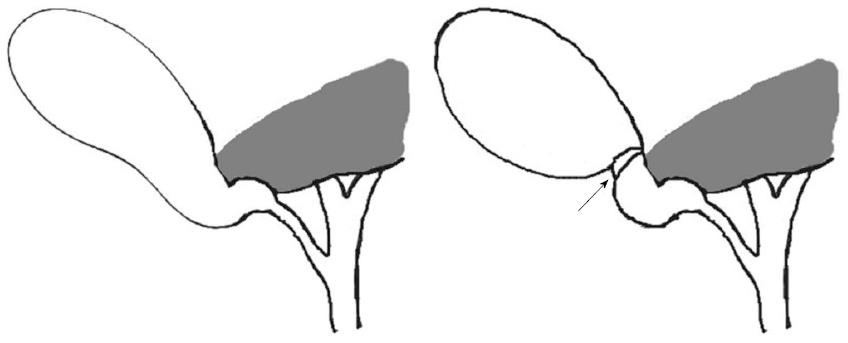
There are two gross congenital types of free-floating gallbladders. Type 1, as illustrated in the present case, is represented by the attachment of the gallbladder and cystic duct to the inferior surface of the liver via the mesentery (Figure 6). Type 2 involves attachment of only the cystic duct to the liver[2,13]. Anatomical anomalies, such as an abnormally long mesentery, can result in a suspended gallbladder, allowing it to float freely from the liver bed. This suspension consequently increases susceptibility to rotational instability. Additional factors that can contribute to gallbladder torsion are peristalsis of the surrounding stomach, duodenum, or transverse colon, spinal deformities, and tortuous atherosclerotic cystic arteries. Gallstones are unlikely to cause torsion because they are only present in 25%-50% of affected patients[4,7,13].
In incomplete torsion, patients frequently present with symptoms similar to those of recurrent biliary colic, but in complete torsion, patients generally present with a short history of sudden-onset, severe upper-right quadrant pain and vomiting. An abdominal mass might or might not be palpable, and there are usually no signs of toxemia or jaundice[8]. Laboratory investigations reveal a normal or high white cell count and normal results on liver function tests because the common bile duct is usually unobstructed[4,11].
Preoperative diagnosis of gallbladder torsion remains difficult because the symptoms and signs are similar to those of acute cholecystitis[3,5,13,16]. In previous reports, only 9.8% of all gallbladder torsion cases have been diagnosed preoperatively[13]. Laboratory evaluations are often nonspecific. White blood cell count and C-reactive protein levels are frequently elevated. However, the results of liver function tests and biliary enzyme are often normal[2,4,14]. On ultrasonography, 3 features are suggestive of gallbladder torsion: a diffusely thickened and hypoechoic gallbladder wall that displays gangrene and/or inflammation[3]; a floating gallbladder, in which the major part of the organ is not adhered to the liver bed; and a conical structure at the gallbladder neck, consisting of multiple linear echoes converging toward the tip of the “cone”.
In advanced stages, ultrasonography and CT are the main imaging approaches used for diagnosis. Ultrasonography and CT can reveal a ‘floating gallbladder’, with gallbladder wall thickening. The present results indicate that a precise comparison of radiologic imaging findings is crucial in diagnosing gallbladder torsion[7,12]. Our experiences have indicated that T2-weighted MRI images are very useful for evaluating necrosis of the gallbladder wall in cases of gallbladder torsion. Early diagnosis of gallbladder torsion can help to prevent life-threatening complications, such as gallbladder gangrene, perforations causing bilious peritonitis, and other infections. Preventing these complications reduces the mortality and morbidity rates, as well as the cost and days of hospitalization[2,9].
In summary, torsion of the gallbladder is a rare condition and is very difficult to diagnose preoperatively, despite advances in diagnostic imaging. However, this diagnosis should be considered in all elderly patients presenting with symptoms suggestive of acute or non-resolving symptoms and signs of cholecystitis, particularly in the absence of gallstones. To achieve the best patient outcome, early diagnostic imaging investigation and prompt cholecystectomy are crucial.
A 73-year-old male presented with severe pain that persisted and increased progressively since the previous day in the upper-right quadrant.
Physical examination demonstrated no palpable mass or Murphy’s sign.
Acute cholecystitis, acute cholangitis, or gallstones.
Routine blood tests, including tests for liver function, biliary enzyme, and inflammatory markers, showed no abnormalities.
T2-weighted magnetic resonance imaging (MRI) showed an intra-gallbladder segment located between the body and neck of the gallbladder, and magnetic resonance cholangiopancreatography indicated V-shaped distortion of the extrahepatic bile duct and a tapered cyst duct.
Histological examination of the specimen revealed acute gangrenous cholecystitis.
Torsion of the gallbladder should be considered in all elderly patients presenting with symptoms suggestive of acute or non-resolving symptoms and signs of cholecystitis, particularly in the absence of gallstones. To achieve the best patient outcome, early diagnostic imaging investigation and prompt cholecystectomy are crucial.
The authors are reporting a case of complete body-neck torsion of the gallbladder concluding that T2-weighted MRI images are not only helpful to confirm the diagnosis, but also in evaluating necrosis of the gallbladder wall in such situations. The report is well written with excellent documentation and demonstration of the images taken for the case.
P- Reviewer: Beltran MA, Elpek GO, Nagem RG, Sira MM S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Wendel AV. VI. A Case of Floating Gall-Bladder and Kidney complicated by Cholelithiasis, with Perforation of the Gall-Bladder. Ann Surg. 1898;27:199-202. [PubMed] |
| 2. | Chung JC, Song OP, Kim HC. Gallbladder torsion diagnosed by MDCT and MRCP. Abdom Imaging. 2010;35:462-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Aibe H, Honda H, Kuroiwa T, Yoshimitsu K, Irie H, Shinozaki K, Mizumoto K, Nishiyama K, Yamagata N, Masuda K. Gallbladder torsion: case report. Abdom Imaging. 2002;27:51-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Janakan G, Ayantunde AA, Hoque H. Acute gallbladder torsion: an unexpected intraoperative finding. World J Emerg Surg. 2008;3:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Pottorf BJ, Alfaro L, Hollis HW. A Clinician’s Guide to the Diagnosis and Management of Gallbladder Volvulus. Perm J. 2013;17:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Tarhan OR, Barut I, Dinelek H. Gallbladder volvulus: review of the literature and report of a case. Turk J Gastroenterol. 2006;17:209-211. [PubMed] |
| 7. | Ijaz S, Sritharan K, Russell N, Dar M, Bhatti T, Ormiston M. Torsion of the gallbladder: a case report. J Med Case Rep. 2008;2:237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Chou CT, Chen RC, Yang AD, Wu HK. Gallbladder torsion: preoperative diagnosis by MDCT. Abdom Imaging. 2007;32:657-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Reddy PK, Muralidharan M, Venkatasubramanian R, Yuvaraja S. Laparoscopic derotation and cholecystectomy for torsion gallbladder. JSLS. 2005;9:238-240. [PubMed] |
| 10. | Gupta V, Singh V, Sewkani A, Purohit D, Varshney R, Varshney S. Torsion of gall bladder, a rare entity: a case report and review article. Cases J. 2009;2:193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Garciavilla PC, Alvarez JF, Uzqueda GV. Diagnosis and laparoscopic approach to gallbladder torsion and cholelithiasis. JSLS. 2010;14:147-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Koyanagi T, Sato K. Complete gallbladder torsion diagnosed with sequential computed tomography scans: a case report. J Med Case Rep. 2012;6:289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Matsuda A, Sasajima K, Miyamoto M, Maruyama H, Yokoyama T, Suzuki S, Matsutani T, Sugiura A, Yanagi K, Matsushita A. Laparoscopic treatment for torsion of the gallbladder in a 7-year-old female. JSLS. 2009;13:441-444. [PubMed] |
| 14. | Shaikh AA, Charles A, Domingo S, Schaub G. Gallbladder volvulus: report of two original cases and review of the literature. Am Surg. 2005;71:87-89. [PubMed] |
| 15. | Usui M, Matsuda S, Suzuki H, Ogura Y. Preoperative diagnosis of gallbladder torsion by magnetic resonance cholangiopancreatography. Scand J Gastroenterol. 2000;35:218-222. [PubMed] |
| 16. | Boonstra EA, van Etten B, Prins TR, Sieders E, van Leeuwen BL. Torsion of the gallbladder. J Gastrointest Surg. 2012;16:882-884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |