Published online Oct 7, 2014. doi: 10.3748/wjg.v20.i37.13620
Revised: May 29, 2014
Accepted: June 25, 2014
Published online: October 7, 2014
Processing time: 175 Days and 21.1 Hours
A diverticulum is a bulging sack in any portion of the gastrointestinal tract. Small intestine diverticular disease is much less common than colonic diverticular disease. The most common symptoms include non-specific epigastric pain and a bloating sensation. Major complications include diverticulitis, gastrointestinal bleeding, acute perforation, intestinal obstruction, intestinal perforation, localized abscess, malabsorption, anemia, volvulus and bacterial overgrowth. We report one case of massive jejunal diverticula bleeding and one case of massive colonic diverticula bleeding, both diagnosed by acute abdominal computed tomography angiography and treated successfully by surgery.
Core tip: Gastrointestinal diverticular disease is common and asymptomatic in most cases; however, massive gastrointestinal bleeding caused by diverticular disease is rare. This article describes the diagnosis and management of these diseases through acute abdominal computed tomography angiography.
- Citation: Xu XQ, Hong T, Li BL, Liu W. Active gastrointestinal diverticulum bleeding diagnosed by computed tomography angiography. World J Gastroenterol 2014; 20(37): 13620-13624
- URL: https://www.wjgnet.com/1007-9327/full/v20/i37/13620.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i37.13620
A diverticulum is a bulging sack in any part of the gastrointestinal tract. The large intestine is the most common site for the formation of diverticula. The diverticulum forms a pouch in a weakness of the intestine, which generally corresponds to the site where an artery enters into the muscle layer. It is thought that spasms increase pressure in the intestine, creating more diverticula and enlarging existing ones. Diverticula are classified as real or false: real diverticula are composed of all of the intestine’s layers, while false diverticula consist of the uncus of the mucosa and the submucosa[1].
Diverticular disease is actually uncommon in people under the age of 40. By the age of 50, about 1/3 of the population has diverticulosis; the prevalence increases to 60% in people over 80 years of age[2].
Colonic diverticular disease is much more common than small intestine diverticular disease. It is believed that diverticula develop as a result of abnormalities in intestinal peristalsis, intestinal dyskinesis and very high intraluminal pressure, such as in the colon[3].
Most gastrointestinal diverticula are asymptomatic; however, they are usually complicated by diverticulitis with or without bowel perforation, intestinal obstruction and bleeding once they become symptomatic. Massive upper gastrointestinal bleeding secondary to gastrointestinal diverticulosis is extremely rare. Most of them present with obscure gastrointestinal bleeding[4-6]. However, colonic diverticular bleeding is a common cause of hematochezia. It accounts for approximately 40% of the episodes of massive lower gastrointestinal bleeding and often results in hospitalization. Severe hemorrhage can occur in 3%-5% of patients with diverticula[7]. Diverticula are predominantly observed in the left colon in Western countries, while right-sided diverticula are more commonly found in Asian countries[8].
Computed tomography (CT) angiography, colonoscopy and angiography are essential for the diagnosis and treatment of gastrointestinal diverticular bleeding[1-8]. However, a precise location and definite hemostasis are often difficult because diverticula are usually numerous and bleeding is intermittent[6-8]. Blind segmental resection in the cases of undiagnosed bleeding site is responsible for the high re-bleeding rate of 42% and mortality of 57%[9]. Therefore, precise localization is essential for the treatment in patients with a life-threatening diverticular bleeding. We herein describe two patients with massive jejunal and colonic diverticular bleeding, respectively, whose bleeding sites were located precisely and successfully by CT angiography and then treated by surgery.
An 86-year-old male presented to the emergency department with recurrent massive hematochezia. His past medical history was significant for hypertension for 20 years without any history of gastrointestinal bleeding. On physical examination, the abdomen was soft without tenderness. His hemodynamic status was unstable, with a hemoglobin of 6.5 g/dL. An acute abdominal CT angiography revealed contrast extravasation in a jejunal diverticulum (Figure 1A, arrow). The superior mesenteric artery was reconstructed, which indicated the blood supply for the jejunal diverticulum source was from a branch of the superior mesenteric artery (Figure 1B, arrow). Once the diagnosis of jejunal diverticular bleeding was made, a laparotomy was performed. Multiple diverticula in a 30 cm segment of jejunum were found, beginning 50 cm distal to the Treitz’s ligament (Figure 1C). The involved segment was resected. The patient had no further postoperative episodes of gastrointestinal bleeding.
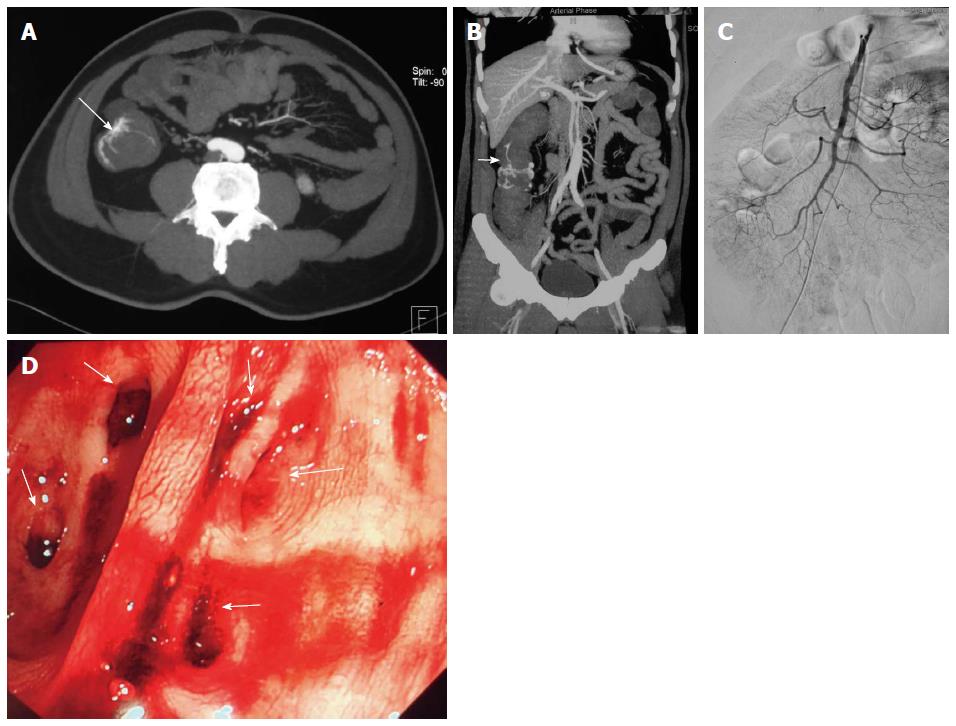
A 56-year-old male presented to the emergency with recurrent massive hematochezia. His past medical history was non-significant, with no history of gastrointestinal bleeding. On physical examination, the abdomen was soft without tenderness. His hemodynamic status was unstable (BP 85/50 mmHg, HR 110/min) with a hemoglobin of 5.4 g/dL. The acute abdominal CT angiography revealed contrast extravasation in the ascending colon (Figure 2A, arrow) and bleeding from the intramural branches of the marginal artery supplying the ascending colon (Figure 2B). Angiography failed to reveal the precise location of the bleeding (Figure 2C). Emergent colonoscopy was performed, which revealed multiple diverticula in the middle part of ascending colon (Figure 2D, arrows), but no definite bleeding vessels were identified. When the conservative treatment for colonic diverticular hemorrhage was unsuccessful after three episodes of hemorrhage, a laparotomy was performed. Partial colectomy for most of the ascending colon was then performed. The patient had no further post-operative episodes of gastrointestinal bleeding.
Gastrointestinal diverticular disease is asymptomatic in up to 70% of cases and patients may suffer from acute complications such as bleeding, perforation, diverticulitis or intestinal obstruction[4-6]. Bleeding is uncommon and constitutes only 5%-33% of all cases[10]. Both upper and lower gastrointestinal diverticular usually involve elderly patients[2]. A significant number of patients also present with life-threatening bleeding. Based on these facts, clinicians should keep in mind with this uncommon but dangerous situation while managing elderly patients with massive gastrointestinal bleeding.
Preoperative diagnosis of gastrointestinal diverticular bleeding is sometimes difficult[11,12]. Many modalities have been introduced to evaluate gastrointestinal diverticular bleeding, including barium contrast study, Technetium99m (99mTc) RBC scan, CT scan, angiography, CT angiography, capsule endoscopy, etc.
The upper gastrointestinal diverticular bleeding is much less common than the lower gastrointestinal diverticular bleeding (colonic diverticular disease). The duodenum is the second most common location for gastrointestinal tract diverticula after the colon. Other less common locations include the third and fourth portions of the duodenum and the jejunum[13].
Colonic diverticula are the most common source of life-threatening lower gastrointestinal bleeding. Most diverticula are located in the descending or sigmoid colon; however, spontaneous bleeding is common in diverticula of the ascending colon[14].
Emergent endoscopy is the standard diagnostic and therapeutic technique for gastrointestinal bleeding, but it can be difficult when the typical gastrointestinal bleeding involves fast and massive bleeding into an unprepared bowel. As a matter of fact, no exact explanation is found in up to 20% in such cases of gastrointestinal bleeding. Arteriography is reserved for patients for whom endoscopy is unfeasible or inconclusive, and for whom bleeding persists after localization; however, it risks ischemic damage to the bowel wall and failure to detect all bleeding sources. CT angiography can be useful in locating the obscure source of bleeding. CT angiography showed pooled sensitivity of 86% and specificity of 95%, respectively in the diagnosis of acute gastrointestinal bleeding[15]. When massive gastrointestinal bleeding occurs in patients with unstable hemodynamic status, CT angiography is essential, it could show sac-like collections of extravasation, so that details of its arterial supply can be clearly ascertained in order to optimize treatment decisions[16].
CT angiography is accurate in the diagnosis of acute gastrointestinal bleeding and can show the precise location and etiology of bleeding. Thus, CT angiography could be used for the first line diagnostic method for most of the patients with active gastrointestinal bleeding without relative absolute contraindications[15].
The management of gastrointestinal diverticular bleeding is mainly by surgical intervention, although there are some reports of spontaneous recovery. The mortality rate has dropped in recent years. The decrease in mortality may be attributed to the advance of diagnostic modalities that allow clinicians to stratify patients for endoscopic therapy, conservative treatment, or surgery[17]. For those with less severe bleeding, endoscopic diagnosis and treatment are good options[18]. A significant number of patients are expected to bleed again during the follow-up period, although such a non-surgical approach does control the bleeding. For those presented with massive bleeding, emergency surgery still remains one of the options to control the bleeding. Whether these patients should receive surgery after initial medical management remains unclear. This approach may be suggested only when they suffer from recurrent bleeding. Surgery is indicated in patients with ongoing recurrent bleeding when therapeutic endoscopy or angiography is not available or feasible. Patients with recurrent gastrointestinal bleeding should certainly be treated with surgery because the risk of further episodes may increase with time[19]. Approximately 10%-25% of patients require emergency surgery for hemodynamic instability[20].
In conclusion, CT angiography is a noninvasive, rapid, reproducible and widely available technique that can be performed successfully upon the majority of patients presenting with an acute episode of gastrointestinal diverticula bleeding. Positive contrast-enhanced multidetector CT can define the bleeding sites with high accuracy. Occasionally, this technique can even define the cause of active gastrointestinal bleeding, which, if combined with anatomical information, can effectively inform subsequent angiography or surgery. Multiphasic imaging enables direct visualization of active bleeding into the bowel. CT angiography could serve as a first diagnostic modality in the evaluation of patients with substantial bleeding[21].
Active gastrointestinal diverticulum bleeding diagnosed by computed tomography (CT) angiography.
It should be considered in the differential diagnosis of patients with gastrointestinal bleeding caused by any other reasons.
Diagnostic imaging mainly by CT angiography.
Angiography or surgery may be performed when definite bleeding sites are identified by CT angiography.
This is a well written and well-documented report of two cases of active gastrointestinal diverticular bleeding.
P- Reviewer: Manguso F, Miller LE, Singhal S S- Editor: Nan J L- Editor: Stewart G E- Editor: Liu XM
| 1. | Chow DC, Babaian M, Taubin HL. Jejunoileal diverticula. Gastroenterologist. 1997;5:78-84. [PubMed] |
| 2. | Cheskin LJ, Bohlman M, Schuster MM. Diverticular disease in the elderly. Gastroenterol Clin North Am. 1990;19:391-403. [PubMed] |
| 3. | Almy TP, Howell DA. Medical progress. Diverticular disease of the colon. N Engl J Med. 1980;302:324-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 176] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Chiu EJ, Shyr YM, Su CH, Wu CW, Lui WY. Diverticular disease of the small bowel. Hepatogastroenterology. 2000;47:181-184. [PubMed] |
| 5. | Liu CY, Chang WH, Lin SC, Chu CH, Wang TE, Shih SC. Analysis of clinical manifestations of symptomatic acquired jejunoileal diverticular disease. World J Gastroenterol. 2005;11:5557-5560. [PubMed] |
| 6. | Rodriguez HE, Ziauddin MF, Quiros ED, Brown AM, Podbielski FJ. Jejunal diverticulosis and gastrointestinal bleeding. J Clin Gastroenterol. 2001;33:412-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997;92:419-424. [PubMed] |
| 8. | Kang JY, Melville D, Maxwell JD. Epidemiology and management of diverticular disease of the colon. Drugs Aging. 2004;21:211-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 62] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Parkes BM, Obeid FN, Sorensen VJ, Horst HM, Fath JJ. The management of massive lower gastrointestinal bleeding. Am Surg. 1993;59:676-678. [PubMed] |
| 10. | Makris K, Tsiotos GG, Stafyla V, Sakorafas GH. Small intestinal nonmeckelian diverticulosis. J Clin Gastroenterol. 2009;43:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 56] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Forcione DG, Alam HB, Kalva SP, Misdraji J. Case records of the Massachusetts General Hospital. Case 9-2009. An 81-year-old man with massive rectal bleeding. N Engl J Med. 2009;360:1239-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Balkissoon J, Balkissoon B, Leffall LD, Posey DA. Massive upper gastrointestinal bleeding in a patient with a duodenal diverticulum: a case report and review of the literature. J Natl Med Assoc. 1992;84:365-367. [PubMed] |
| 14. | Lewis M. Bleeding colonic diverticula. J Clin Gastroenterol. 2008;42:1156-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Chua AE, Ridley LJ. Diagnostic accuracy of CT angiography in acute gastrointestinal bleeding. J Med Imaging Radiat Oncol. 2008;52:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Tsurukiri J, Ueno M, Kaneko N. Bleeding at the hepatic flexure of the colon secondary to diverticulosis. Clin Gastroenterol Hepatol. 2012;10:e11-e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Yen HH, Chen YY, Yang CW, Soon MS. Diagnosis and management of jejunoileal diverticular hemorrhage: a decade of experience. J Dig Dis. 2012;13:316-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Chen TH, Chiu CT, Lin WP, Su MY, Hsu CM, Chen PC. Application of double-balloon enteroscopy in jejunal diverticular bleeding. World J Gastroenterol. 2010;16:5616-5620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | McGuire HH. Bleeding colonic diverticula. A reappraisal of natural history and management. Ann Surg. 1994;220:653-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 198] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 20. | Zuccaro G. Management of the adult patient with acute lower gastrointestinal bleeding. American College of Gastroenterology. Practice Parameters Committee. Am J Gastroenterol. 1998;93:1202-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 125] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Laing CJ, Tobias T, Rosenblum DI, Banker WL, Tseng L, Tamarkin SW. Acute gastrointestinal bleeding: emerging role of multidetector CT angiography and review of current imaging techniques. Radiographics. 2007;27:1055-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |