Published online Oct 7, 2014. doi: 10.3748/wjg.v20.i37.13615
Revised: April 1, 2014
Accepted: May 19, 2014
Published online: October 7, 2014
Processing time: 256 Days and 17.1 Hours
Intestinal obstruction is a common complication associated with Meckel’s diverticulum in adults. The diverticulum itself or its fibrous band can lead to an intestinal volvulus, intussusceptions, or closed-loop obstructions, which require surgery. The incarceration of Meckel’s diverticulum in either inguinal or femoral hernia sacs (Littre’s hernia) is another, less common, etiology underlying intestinal obstruction. This case report describes a 45-year-old man who had an obstruction associated with a Meckel’s diverticulum that passed through a congenital defect in the mesocolon into the right subphrenic space. The patient, who had not undergone abdominal surgery previously, came to the emergency room with acute onset of intermittent epigastric pain and abdominal distention. Computed tomography images showed the presence of a segment of the small bowel and a diverticulum in the right subphrenic space and paracolic gutter. The twisted mesentery and the dilated loops of the proximal small bowel were indicative of an intestinal volvulus and obstruction. Meckel’s diverticulum complicated by a transmesocolic internal hernia was diagnosed, and this condition was confirmed during emergency surgery. The patient’s postoperative recovery was uneventful. This case report highlights another presentation of Meckel’s diverticulum, that is, in combination with a transmesocolic internal hernia. This etiology may lead to an intestinal volvulus and necessitate early surgery.
Core tip: Intestinal obstruction is a common complication associated with Meckel’s diverticulum in adults. It can also be complicated with transmesocolic internal hernia, which had not been reported before. Early surgery is necessary since it could result in intestinal volvulus and closed-loop obstruction. High clinical suspicion in acute abdomen is important while computed tomography scans helps preoperative diagnosis.
- Citation: Wu SY, Ho MH, Hsu SD. Meckel's diverticulum incarcerated in a transmesocolic internal hernia. World J Gastroenterol 2014; 20(37): 13615-13619
- URL: https://www.wjgnet.com/1007-9327/full/v20/i37/13615.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i37.13615
Obstruction of the small bowel originating from congenital abnormalities is uncommon among adults. The correct diagnosis of obstructions of the small bowel requires differentiation of normal anatomy from pathologic findings using radiography, and the presence of a high index of clinical suspicion. Meckel’s diverticulum is the most common congenital anomaly of the gastrointestinal tract. Adult patients affected by Meckel’s diverticulum may be asymptomatic until they experience acute small-bowel obstruction, which may be caused by either the fibrous band of the diverticulum or a volvulus of the small bowel around the diverticulum[1]. However, incarceration of Meckel’s diverticulum within a transmesocolic internal hernia is an unusual etiology. Here, we describe the case of a patient who had an acute obstruction of the small bowel. An incarcerated Meckel’s diverticulum in the right subphrenic space with an intestinal volvulus was found on computed tomography (CT) images. In addition, a transmesocolic internal hernia was found during radiography, and this finding was confirmed during surgery.
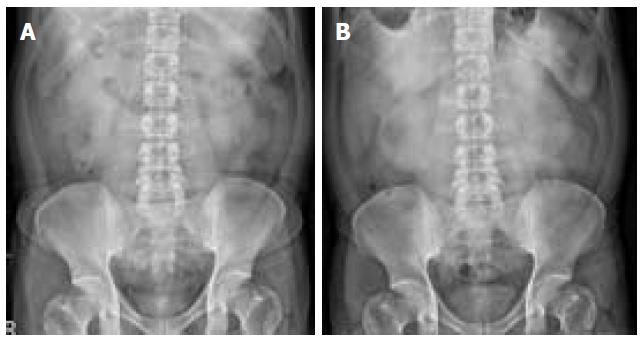
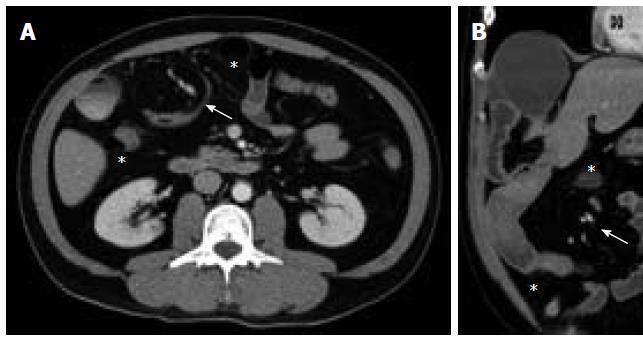
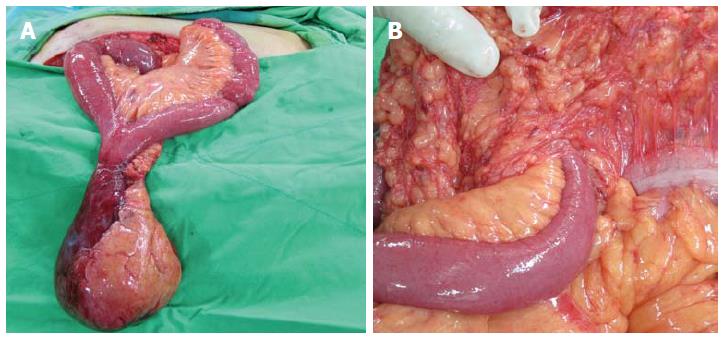
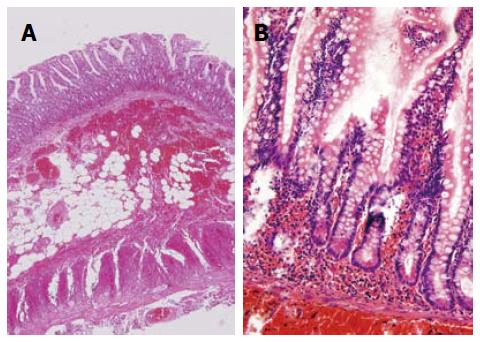
A 45-year-old man who did not have a history of systemic diseases and had no history of abdominal surgery was admitted to our emergency room (ER). On the day before he came to the ER, he had experienced acute onset of intermittent epigastric pain and abdominal distention, with nausea, vomiting, and diarrhea. Several years before being admitted to the ER, the patient had experienced episodes of dull epigastric pain, accompanied by bloating and constipation. However, the patient had ignored the pain because the intensity of the pain fluctuated and the pain appeared to be self-limiting. Initial physical examinations showed increased level of bowel sounds, no abdominal tenderness, and no palpable masses. Results from the patient’s blood tests were normal. Plain-film radiographic images of the abdomen did not show the ileus, but revealed relative radiolucencies lateral to the liver. Compared with a plain film obtained in the outpatient department 5 mo previously, these images showed more prominent presence of bowel gas between the liver and diaphragm (Figure 1). Eight hours after being admitted to the ER, the patient’s colic became increasingly severe and more frequent, and diffuse abdominal tenderness was apparent on physical examination. Emergency CT scans showed incarceration of one segment of the intestine in the right subphrenic space where the mesenteric vessels and the soft tissues twisted around each other in the prehepatic space, which is known as a “whirl sign” (Figure 2). Furthermore, a segment of the strangulated intestine or a diverticulum of the intestine depressed the liver surface and displaced the hepatic flexure of the colon medially. However, free air and ascites were not present within the subphrenic space. We suspected a volvulus and bowel ischemia, and we performed a diagnostic laparoscopy, which was converted to a laparotomy after confirmation of the ischemic bowel. A 20-cm segment of the ileum passed through a 10-cm defect in the transverse mesocolon into the subphrenic space, 30 cm proximal to the ileocecal valve. Within this, a 6-cm antimesenteric diverticulum was trapped in the subphrenic space (Figure 3). The diverticulum served as the lead point of mesenteric twisting, causing bowel ischemia. After clamping the mesenteric vessels, segmental resection and end-to-end anastomosis of the ileum were performed. The histopathology of the diverticulum showed mucosal infarction and excessive submucosal hemorrhage, with neutrophil infiltration in the ileum tissue. The bowel wall contained all layers without metaplasia of gastric or pancreatic mucosa (Figure 4). These findings were more suggestive of bowel ischemia rather than acute diverticulitis since no dense lymphocyte infiltration was observed in the lamina propria. These findings are compatible with those of a true congenital diverticulum, namely, Meckel’s diverticulum. The patient recovered well after surgery. He was discharged from hospital, without complications, after 9 d.
Meckel’s diverticulum, a true diverticulum arising from the antimesenteric side, is the most common congenital anomaly of the gastrointestinal tract. While most patients with Meckel’s diverticula do not experience complications, between 4% and 16% of patients experience complications[1]. Bleeding in association with ectopic gastric mucosa is the most common complication in children, whereas obstructions caused by intussusceptions or adhesion bands are more common in adults. Furthermore, a Meckel’s diverticulum may protrude through an abdominal opening. In Littre’s hernia, a Meckel’s diverticulum can enter the inguinal canal, umbilical canal, or femoral canal, causing incarceration or strangulation[2]. Sometimes, the adhesion band of the diverticulum forms a space that may cause the internal herniation of the small intestine[3]. However, the protrusion of a Meckel’s diverticulum through a congenital defect in the mesocolon is extremely rare. Indeed, when we searched the medical literature published in English, we could not find a case that was similar to the one that is reported here.
During the development of internal abdominal hernias, the intestines intrude into a cavity or defect in the peritoneal cavity. Internal hernias comprise up to 5.8% of intestinal obstructions[4]. Most internal hernias involve intestines passing through physiologic openings, and they may be categorized as paraduodenal hernias, pericecal hernias, foramen of Winslow’s hernias, or inter-sigmoid hernias. Other internal hernias are associated with congenital or acquired defects, and they are categorized as transmesenteric, transmesocolic hernias, and transomental hernias[5,6]. Without intestinal strangulation, patients may have no symptoms or insidious, vague, postprandial abdominal pains, which are often ignored. Most patients are not given a diagnosis until the nausea, vomiting, and the acute, cramping, periumbilical pain, become suggestive of an intestinal obstruction, and CT images are critical in these diagnoses. The location of the herniated loops of the small bowel is anatomically abnormal, and they may displace adjacent organs and cause the engorgement, crowding, twisting, or stretching of the mesenteric vessels[7]. The location of the loops of the small bowel helps determine etiology. For left paraduodenal hernias, the small bowel enters a congenital fossa behind the ascending duodenum, and bowel loops are present between the stomach and pancreas. In contrast, in right paraduodenal hernias, bowel loops are present just lateral and inferior to the descending duodenum. In paracecal hernias, the bowel loops are located posterior and lateral to the cecum in the right paracolic gutter. In intersigmoid hernias, the incarcerated small bowel is posterior and lateral to the sigmoid colon. In transmesenteric hernia, the small bowel travels through a mesenteric defect to the lateral side of the colon and displaces the overlying omentum, creating a directly abutting abdominal wall. Most transmesenteric hernias in adults are acquired and are secondary to previous abdominal surgery such as Roux-en-Y anastomoses for gastric bypass or hepaticojejunostomies. In contrast, congenital defects are more frequent in children. Since our patient had none of the etiologies that would have led to the acquisition of an internal hernia, including previous abdominal surgery, trauma, or peritonitis, the defect in the mesocolon was probably congenital. CT scans showed the entrapped intestinal diverticulum in the right subphrenic space depressing the liver’s surface. Furthermore, the small intestine was located lateral to the ascending colon and displaced the hepatic flexure of the colon downwards, indicating a possible internal hernia. While an intestinal volvulus was also suggested by the twisted mesenteric vessels and the proximal dilation of the incarcerated small intestine, the incarcerated small intestine and the diverticulum may have also served as a leading point. The emergency surgery warranted by this closed-loop intestinal obstruction confirmed that the Meckel’s diverticulum passed through a congenital defect in the mesocolon and into the right subphrenic space with an intestinal volvulus.
As the images illustrate, the intestines were in the right subphrenic space, and in these instances Chilaiditi’s sign, an indication of colonic interposition between the liver and the diaphragm, should always be considered. Chilaiditi’s sign is usually an incidental finding on abdominal radiographs and it tends to exist without any symptoms. Relaxation of the suspensory ligaments mobilizes the right colic flexure, making interposition possible. When this is accompanied by symptoms associated with bowel obstruction, including abdominal pain, nausea, vomiting, bloating, and anorexia, it is called Chilaiditi’s syndrome[8]. However, a diagnosis of Chilaiditi’s syndrome should be differentiated from diseases associated with acute abdomen, which include pneumoperitoneum, subphrenic abscess, obstructions of the small bowel, volvulus, intussusceptions, ischemic bowel, and inflammatory conditions, for example, appendicitis or diverticulitis, all of which require prompt surgical intervention. In contrast, Chilaiditi’s syndrome is managed by medical treatment initially, rather than surgery. Surgical intervention, in the form of cecopexy or colonic resection, is indicated when medical treatment fails, or if there is evidence of bowel ischemia, for example, volvulus of the transverse colon or cecum. Our patient had an acute abdomen, and CT scans showed a small-bowel volvulus and a closed-loop obstruction. The normal proximal ascending colon, cecum, and terminal ileum excluded the colonic obstruction that characterizes Chilaiditi’s syndrome. Our patient’s radiologic findings were confirmed by diagnostic laparoscopy.
A radiologic finding of a small bowel trapped between the diaphragm and the liver requires careful evaluation. A patient who presents with an acute abdomen requires emergency diagnostic laparoscopy or laparotomy. Furthermore, it is important to exclude internal hernias by identifying the relative anatomic locations of the intra-abdominal organs on CT images in patients who have incidental findings. If congenital anomalies such as Meckel’s diverticulum are apparent on CT images, we suggest prompt surgical investigation, because of risk of an intestinal volvulus.
A 45-year-old man with acute intermittent epigastric pain, abdominal distention, nausea, vomiting, and diarrhea.
increased level of bowel sounds, no abdominal tenderness initially then progression to diffuse tenderness , no palpable masses.
Intestinal obstruction related to congenital anomaly or neoplasm, Chilaiditi syndrome.
White blood cell: 13560/uL; C-reactive protein: 0.14 mg/dL; metabolic panel and liver function test were within normal limits.
CT scans showed incarceration of one segment of the intestine in the right subphrenic space where the mesenteric vessels and the soft tissues twisted around each other in the prehepatic space.
Meckel’s diverticulum with ischemic change secondary to volvulus.
Laparotomy with reduction of transmesenteric internal hernia and resection of incarcerated ileum including Meckel’s diverticulum.
Others reported the adhesion band of the diverticulum forms a space that may cause the internal herniation of the small intestine. But we could not find a case like ours with Meckel’s diverticulum passing through a congenital defect in the mesocolon.
In patient with clinical diagnosis of intestinal obstruction, internal hernias are differentiated by identifying the relative anatomic locations of the intra-abdominal organs on CT scans. Combination of Meckel’s diverticulum and transmesenteric internal hernia is possible, and we suggest prompt surgical investigation even in asymptomatic patients because of risk of an intestinal volvulus.
This is a well written case report of surgical interest. On histology the authors should comment on the presence of acute inflammation indicating if there was also acute diverticulitis as now they only describe absence of metaplasia.
P- Reviewer: Sakakima Y, Tiniakos D S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Sagar J, Kumar V, Shah DK. Meckel’s diverticulum: a systematic review. J R Soc Med. 2006;99:501-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 196] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 2. | Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Littre hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72:238-243. [PubMed] |
| 3. | Ko SF, Tiao MM, Huang FC, Hsieh CS, Huang CC, Ng SH, Wan YL, Lee TY. Internal hernia associated with Meckel’s diverticulum in 2 pediatric patients. Am J Emerg Med. 2008;26:86-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Stern LE, Warner BW. Congenital internal abdominal hernias: incidence and management. Fitzgibbons RJ Jr, Greenburgs AG Nyhus and Condon’s Hernia. 5th ed. Philadelphia: Lippincott 2002; 453-465. |
| 6. | Meyers MA. Dynamic radiology of the abdomen: normal and pathologic anatomy. New York: Springer 2000; . |
| 7. | Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186:703-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 371] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 8. | Moaven O, Hodin RA. Chilaiditi syndrome: a rare entity with important differential diagnoses. Gastroenterol Hepatol (N Y). 2012;8:276-278. [PubMed] |