Published online Sep 14, 2014. doi: 10.3748/wjg.v20.i34.12363
Revised: February 22, 2014
Accepted: April 30, 2014
Published online: September 14, 2014
Processing time: 273 Days and 13.3 Hours
Bile duct injuries (BDIs) are difficult to avoid absolutely when the biliary tract has a malformation, such as accessory hepatic duct. Here, we investigated the management strategies for BDI combined with accessory hepatic duct during laparoscopic cholecystectomy.
Core tip: We reviewed the management strategies of four cases of bile duct injuries during laparoscopic cholecystectomy because of accessory hepatic duct. The results will help surgeons select the appropriate treatment strategy.
- Citation: Ren PT, Lu BC, Yu JH, Zhu X. Management of bile duct injuries combined with accessory hepatic duct during laparoscopic cholecystectomy. World J Gastroenterol 2014; 20(34): 12363-12366
- URL: https://www.wjgnet.com/1007-9327/full/v20/i34/12363.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i34.12363
Laparoscopic cholecystectomy (LC) is always considered as the gold standard for cure of benign gallbladder disease. However, the widespread adoption of LC has led to an increased frequency of bile duct injuries (BDIs), which are difficult to manage and may induce a series of serious complications[1-3]. Accessory hepatic duct, a malformation of high-location biliary tract, is infrequently found but often induces BDI during LC[4,5]. BDI combined with accessory hepatic duct is still seldom reported and the treatment is controversial. Therefore, we investigated the management strategies for BDI combined with accessory hepatic duct during LC through case studies.
Eleven cases of BDI (0.23% in all 4820 cases with LC) occurred during LC from January 2001 to December 2008 in our institution. Four cases combined with accessory hepatic duct were enrolled in our study, and the incidence of accessory hepatic duct was 36.4% in all BDI cases (4/11).
BDI was recognized during the operation and management was performed by LC. Right hepatic duct and accessory hepatic duct were transected close to the liver tissue, and the left hepatic duct was torn about 10 mm from the liver tissue. Common hepatic duct injury was also confirmed in this case.
After dissociation of connective tissue from the porta hepatis, we inserted a 2.5-mm silicone tube into the left hepatic duct and fixed it with an absorbable ligature. One of the transverse arms of a 12Fr T tube was inserted into the right hepatic duct with internal fixation. The injured accessory hepatic duct was sheared at the level of the hepatic capsule. A Roux-en-Y hepatojejunostomy was performed among the jejunum, fascia of the porta hepatis, and portal vein sheath. The silicone tube and T tube (the other arm was inserted into the jejunum) were led out of the jejunum about 15 cm from the anastomosis. Eleven weeks after the operation, the silicon tube was slipped off by self-motion. Eighteen weeks after the operation, the T tube was removed, and liver function was normal. Postoperative recovery was uneventful and the patient recovered well during 4 years follow-up.
BDI was recognized during the operation and management was performed by LC. The right hepatic duct and accessory hepatic duct that arose from the left branch of the bifurcation of the hepatic duct were transected. Left hepatic duct and common hepatic duct were torn.
The management was similar to Case 1, except for a 3-mm silicon tube instead of the T tube. The two silicon tubes drained well after the operation. However, the patient suffered from bile leakage from 3 d after surgery. At 16 d after the operation, the abdominal drain became clear. Six months post-surgery, both the silicon tubes were removed, and liver function became normal. The patient recovered well during 2 years follow-up.
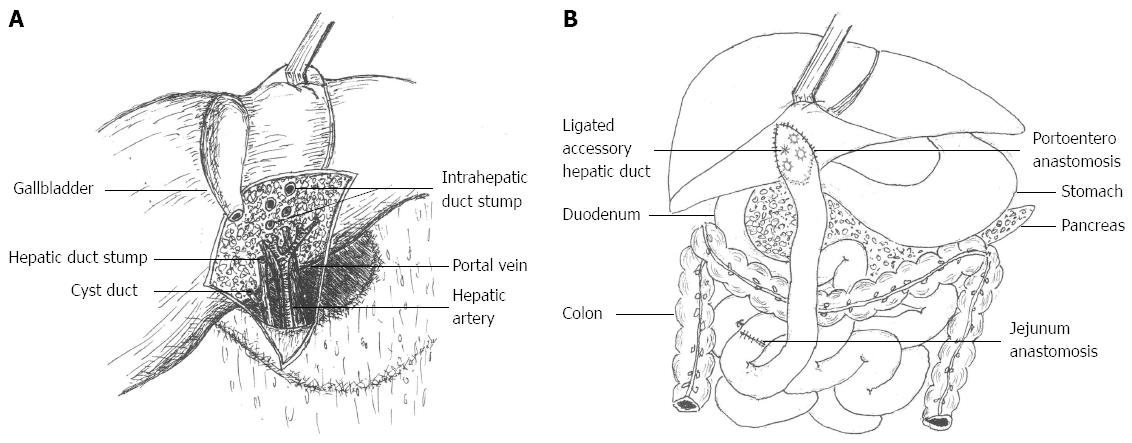
BDI was recognized during the operation and management was performed by converting to laparotomy. The right hepatic duct and two accessory hepatic ducts were transected respectively. The common bile duct, common hepatic duct and left hepatic duct were all torn (Figure 1A).
In this case, the injured bile ducts were slim around the porta hepatis and one of the accessory hepatic ducts arose from the hepatic duct bifurcation. The posterior wall of the left hepatic duct and common bile duct were repaired and an accessory bile duct was ligated (Figure 1B). Three silicon tubes (2-2.5 mm) were inserted into the left hepatic duct, right hepatic duct, and another accessory bile duct as stents (Figure 1B). The anterior wall was repaired using a round ligament. Recovery of the patient was uneventful. Cholangiography demonstrated a dilated left hepatic duct with a narrow right hepatic duct, but without bile leakage. Liver function tests revealed slightly elevated enzyme levels and bilirubin during 20 mo follow-up, therefore, bile duct stricture was diagnosed. The patient underwent a Roux-en-Y hepatojejunostomy instead of cholangioenterostomy because of conglutination after laparotomy. At 12 mo after the operation, liver function became normal, without any symptoms.
BDI was diagnosed at 5 d postoperatively and a second operation was performed. The right hepatic duct and accessory hepatic duct were transected. The common bile duct, common hepatic duct and left hepatic duct were all torn.
The posterior wall of the common bile duct, common hepatic duct, left hepatic duct and right hepatic duct were repaired in the second operation. A 3.5-mm silicon tube was inserted into the left hepatic duct, and two arms of a 12Fr T tube were inserted into the right hepatic duct and accessory bile duct as a stent. Both drainage tubes were led out of the common bile duct. The anterior wall of the bile duct was repaired with a round ligament and enfolded with epiploon. Bile leakage was diagnosed at 5 d after the second operation, improved at 23 d, and the abdominal drain was removed at 36 d after the second operation. Ten months later, postoperative cholangiography showed no serious problem except for mild stricture of the right hepatic duct. Alkaline phosphatase, γ-glutamyltransferase and bilirubin were slightly elevated and returned to normal at 2 years post-surgery.
High-location BDI is a serious complication of LC and anatomic malformation is an important risk factor for it. In our experience, BDI combined with accessory bile duct were seen in 4/11 (36.4%) bile duct ligation cases and 4/4820 (0.083%) of all LC cases, which is similar to other reports[6,7]. Anatomic abnormality of the bile ducts, acute or chronic cholecystitis, and lack of experience were important causes in all our cases. The hepatic ducts of patients who have accessory hepatic ducts are always thinner and longer than those of patients who have a typical anatomical structure. It is always difficult for surgeons to identify cystic ducts, hepatic ducts and accessory hepatic ducts. Moreover, changes in anatomical structure, tissue adhesion and hemorrhage during surgery, which were induced by acute cholecystitis (Cases 1 and 2), or chronic but repeating cholecystitis (Case 4), were other key causes of bile duct dissociation and injury. Even more remarkably, the high-location BDI combined with accessory bile duct is always difficult to repair and reoperation is unavoidable if early repair fails.
No doubt, experience and adept practice are effective approaches to avoid BDI, but are they enough? Accessory hepatic duct is always ignored when Calot’s triangle is difficult to divide, especially in cases with severe adhesion, stone impact, atrophy, and Mirrizzi syndrome[6]. Furthermore, the right and left hepatic ducts are usually narrower but longer when accessory bile ducts arise (as in Case 3). Therefore, it is important to establish a standard management for BDI combined with accessory hepatic duct during LC.
Early diagnosis is the first step of management for BDI[7]. It is necessary for surgery to exam if there is bile escaping from the fossa of the gallbladder, and if there is another duct in the excision apart from the cystic duct. Intraoperative cholangiography is another effective method for early detection of BDI. After surgery, some symptoms must be paid attention, such as obstructive jaundice excluded residual stones in the bile duct, bile leakage from the abdominal drain, severe abdominal pain, and postoperative bile peritonitis is diagnosed by peritoneocentesis. All of these demonstrate BDI and require treatment.
Routine end-to-end hepatoenterostomy or other similar methods may not be enough for cure of BDI combined with accessory bile duct, because of postoperative bile duct narrowing and technical difficulty[8]. In our opinion, a Roux-en-Y hepatojejunostomy with internal drainage performed in one-stage is the preferred management strategy (Cases 1 and 2). The advantage of this procedure is that repair of proximal BDI is possible regardless of the accessory bile duct and the size or site of the injured bile duct.
Round ligament was recognized as an ideal method to repair biliary tract wall in our study (Cases 3 and 4). Although bile duct stricture occurred after 20 mo because of scarring around the anastomosis in Case 3, the problem was resolved by hepatoenterostomy and achieved a good outcome. Some studies have suggested the use of a stent in the bile duct stump[9]. Proponents of this method state that the drainage tube can support the bile duct and reduce the incidence of stricture. We assume it is more important to operate carefully, shear clear of the bile duct stump, and remove the injured bile duct. The healthy bile duct stump can be preserved in the bowel cavity, thus scarring or inflammation around the anastomosis has only a mild influence on it. Experienced hepatobiliary surgeons appear to be necessary to ensure optimal results. Bile duct stumps surrounded with hepatic tissue ensure that the anastomosis is tension free.
BDI with accessory hepatic duct is difficult to avoid absolutely, but it can be managed with appropriate treatment. We have described four cases of BDI combined with accessory hepatic duct in an 8-year period in a total of 4820 cases, which suggest management strategies for this special high-location BDI. We conclude that hepatoenterostomy combined with morioplasty with round ligament, may be an option to consider in life-threatening injuries involving the hepatic duct bifurcation and accessory hepatic duct.
Bile duct injuries (BDIs) are difficult to avoid absolutely when the biliary tract has a malformation, such as an accessory hepatic duct.
Symptomatic cases may be diagnosed in which abnormal bile flow is found during the operation, and abdominal pain, jaundice, and abnormal liver function are found after surgery.
With the aid of magnetic resonance cholangiopancreatography (MRCP), BDIs can be distinguished from bile duct truncation.
Abnormal liver function may be found after surgery.
MRCP revealed bile duct truncation.
Hepatoenterostomy combined with morioplasty with a round ligament, may be an option to consider in injuries involving the hepatic duct bifurcation and accessory hepatic duct.
High-location BDI is difficult to avoid absolutely, but it can be managed with appropriate treatment. Hepatoenterostomy combined with morioplasty with round ligament, may be an option to consider in life-threatening injuries involving the hepatic duct bifurcation and accessory hepatic duct.
High-location BDIs are difficult to avoid absolutely, and experience is needed for hepatobiliary surgeons.
P- Reviewer: Noguera J, Rangarajan M S- Editor: Ma YJ L- Editor: Kerr C E- Editor: Ma S
| 1. | Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9-14. [PubMed] |
| 2. | Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290:2168-2173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 316] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 3. | Wu YV, Linehan DC. Bile duct injuries in the era of laparoscopic cholecystectomies. Surg Clin North Am. 2010;90:787-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Cannon RM, Brock G, Buell JF. A novel classification system to address financial impact and referral decisions for bile duct injury in laparoscopic cholecystectomy. HPB Surg. 2011;2011:371245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Lau WY, Lai EC. Classification of iatrogenic bile duct injury. Hepatobiliary Pancreat Dis Int. 2007;6:459-463. [PubMed] |
| 6. | Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101-125. [PubMed] |
| 7. | Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, Talamini MA, Pitt HA, Coleman J, Sauter PA. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005;241:786-92; discussion 793-5. [PubMed] |
| 8. | Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM. “Sideways”: results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg. 2009;249:426-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |