Published online Sep 14, 2014. doi: 10.3748/wjg.v20.i34.12359
Revised: April 2, 2014
Accepted: April 21, 2014
Published online: September 14, 2014
Processing time: 222 Days and 4.2 Hours
Liver transplantations were performed on two patients with hepatic failure caused by liver cirrhosis. Hard obsolete thrombi and portal venous sclerosis were observed in the major portal veins of both patients. The arteria colica media of one recipient and the portal vein of the donor were anastomosed end-to-end. The hepatic artery of the first donor was anastomosed end-to end with the gastroduodenal artery of the first recipient; meanwhile, the portal vein of the second donor was simultaneously anastomosed end- to-end with the common hepatic artery of the second recipient. The blood flow of the portal vein, the perfusion of the donor liver and liver function were satisfactory after surgery. Portal vein arterialization might be an effective treatment for patients whose portal vein reconstruction was difficult.
Core tip: Portal vein arterializations of patients with portal vein reconstruction difficulties (e.g., extensive portal thrombosis, portal venous cavernous transformation and decreased portal vein perfusion) suggest that this technique is an effective treatment for liver transplantation patients; however, we should also pay close attention to preventing postoperative complications.
- Citation: Zhang K, Jiang Y, Lv LZ, Cai QC, Yang F, Hu HZ, Zhang XJ. Portal vein arterialization technique for liver transplantation patients. World J Gastroenterol 2014; 20(34): 12359-12362
- URL: https://www.wjgnet.com/1007-9327/full/v20/i34/12359.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i34.12359
Portal vein thrombosis (PVT) occurs at a rate of 2%-19% among patients before liver transplantation. This complication can impede portal vein reconstruction during transplantation. In the past, portal vein thrombosis was considered a contraindication for liver transplantation. Using portal vein arterialization, however, the portal vein or its branches are connected with the arterial blood, which can increase or substitute for portal vein perfusion into the new liver. This method was previously usually used among patients with portal vein hypertension or hilar cholangiocarcinoma. We used this liver transplantation method for patients whose portal vein could not be reconstructed because of severe portal vein thrombi. The therapeutic effects were positive.
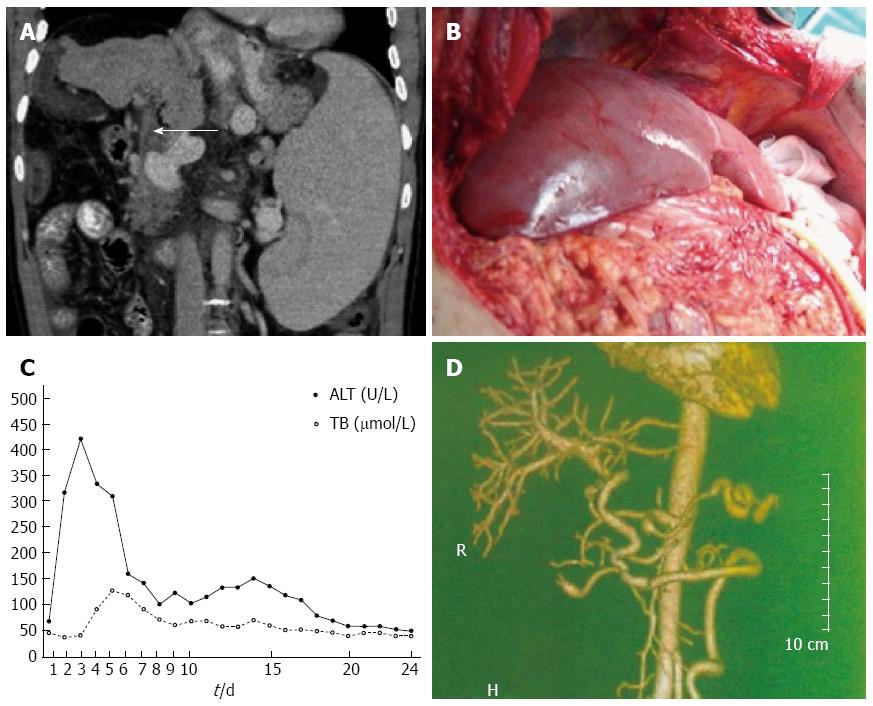
Patient one was a fifty-year-old male with a 5-year history of fatigue, abdominal distension and ascites. Furthermore, he experienced hematemesis more than twice and had a 15-year history of hepatitis B. Color Doppler and computed tomography (CT) tests both indicated that thrombi existed in the portal vein (Figure 1A). This patient was diagnosed with decompensated cirrhosis, portal vein hypertension complicated with upper gastrointestinal hemorrhage, portal vein thrombi (Genotype-IV) and hypersplenism. Moreover, hepatatrophy, megalosplenia, portacaval collateral, portal venous sclerosis and portal vein thrombi were observed during surgery. The patient’s enlarged spleen and sclerotic liver were removed; his portal vein was reconstructed via a donor portal vein/recipient arteria colica media end-to-end anastomosis after the thrombi were removed. During surgery, we found that the blood flow of the portal vein was insufficient, and the portal vein showed poor elasticity. After the portal vein stoma was removed, we found a new thrombus in the portal vein. Thus, we decided to ligate the recipient’s portal vein and anastomose the recipient’s colica media and the donor’s portal vein end-to-end. The transplanted liver received sufficient blood perfusion after the stoma opened, and the donor’s portal vein had sufficient elasticity (Figure 1B). The patient’s liver function became normal one week after surgery (Figure 1C), and he left the hospital 40 d later in a healthy condition. The stoma of the recipient’s colica media and the donor’s portal vein were slightly stenotic, and blood flow remained sufficient three months after surgery, according to a CT scan (Figure 1D). The patient has remained healthy for three years, and his liver functions are all normal.
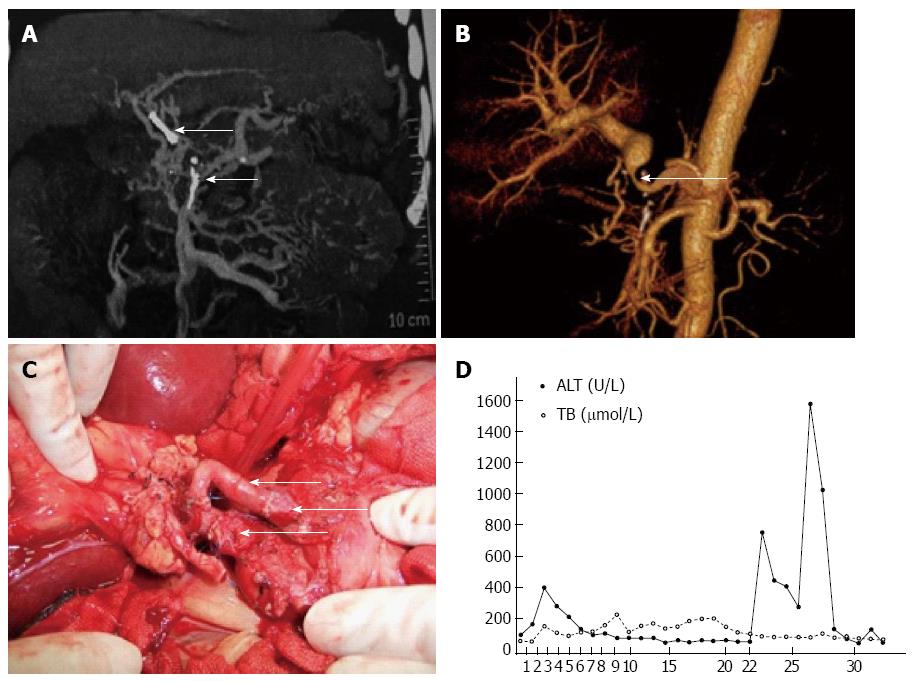
Patient two was a forty-one-year-old male with a history of multiple events of obnubilation over seven years, although the severity of this disease increased over the ten days before surgery. In addition, he had a history of hepatitis B for approximately twenty years. A splenectomy and devascularization around the cardia were performed ten years ago; a hemostasis treatment with a hardener injection under gastroscopy was performed twice after the operation because of upper gastrointestinal hemorrhaging. A CT scan revealed liver cirrhosis with esophageal and gastric varices, as well as widespread thrombi in the superior mesenteric and portal veins (Figure 2A). Patient Two was diagnosed with hepatitis B with liver cirrhosis (decompensation stage), hypertension of the portal vein with upper gastrointestinal hemorrhaging and thrombosis in the portal vein (Type IV). During the operation, we observed severe liver cirrhosis and that the widespread portal vein thrombosis was hard: the latter was difficult to remove. At that point, we decided to treat this patient via primary liver transplantation and portal vein arterialization. The common hepatic artery of the recipient and the portal vein of the donor were anastomosed end-to-end (Figure 2B), and successful liver perfusion was accomplished after the anastomosis was opened. Liver function gradually became normal one week after the operation (Figure 2C); the diameter of the graft portal vein enlarged and the anastomosis was kept smooth according to a CT scan one month after the operation (Figure 2D). Acute rejection occurred with regard to the transplanted liver twenty-five days after the operation, which was cured using a hormone impact treatment (urbason, 300 mg/d for three days). Unfortunately, the patient was unable to continue the therapy sixty days after transplantation because of a severe pulmonary infection and acute renal failure; he died of these diseases shortly thereafter.
The portal vein plays an important role in maintaining the blood perfusion and function of the liver. If portal vein thrombi cannot be removed or if blood perfusion does not recover even after their removal, then the portal vein of liver transplantation patients cannot be reconstructed as usual. The portal vein arterialization technique might bring new hope to these patients.
For liver transplantation patients whose portal vein could not be reconstructed because of the severe portal vein thrombi, the techniques most often used have been portal vein and inferior vena cava end-to-end or side-to-side anastomosis or portal vein arterialization. The former was first reported by Tzakis et al[1], and it has been widely used and reported in our country. The latter technique was first reported by Charco et al[2] with regard to three patients in 2001; however, few reports of liver transplantations using this method exist after that study. In the current research, the thrombus was removed from one patient; however, the blood flow through the portal vein decreased. Moreover, the portal vein thrombi could not be removed from the other patient. Portal vein arterialization was then used on these patients, and the operations were successful. The patients’ liver functions recovered smoothly; one patient survived for three years after the operation, and no abnormal findings were detected at the follow-up liver function evaluation.
Portal vein arterialization might maintain normal liver blood perfusion in liver transplantations. Animal research has verified that liver functions, blood ammonia level, blood bile acid level and liver cell morphology remain normal after portal vein arterialization. Alanine aminotransferase (ALT), AKBR and the oxygen partial pressure of the portal and hepatic veins were significantly improved. Increasing the oxygen supply after portal vein arterialization might effectively prevent acute hepatic failure[3], and the energy metabolism of liver cells might also be improved. Compared with the non-arterialization group, the serum aspartate aminotransferase (AST) and ALT of the arterialization group did not show significant differences during the 2nd hour after the operation (P > 0.05); however, the serum AST and ALT levels were significantly decreased during the 12th hour among the arterialization group (P < 0.01 and P < 0.05, respectively). Compared with the non-arterialization group, the adenosine triphosphate (ATP) content of the liver tissue and the EC value were significantly increased at the 2nd, 6th and 12th hour in the arterialization group (P < 0.01 and P < 0.05, respectively). Hepatic pathological changes were progressively exacerbated with the prolonged duration of ischemia in the non-arterialization group, whereas the injury of hepatic cells in the arterialization group was mild[4]. These results provided the theoretical foundations for the clinical use of portal vein arterialization. However, we should also keep in mind that this technique is a type of non-physiological condition. This technique might increase the blood perfusion through the portal vein, blood pressure and oxygenation oxyhydrase; furthermore, it might decrease the trophic factors of the hepatic inflows[5]. Hepatic microcirculation turbulence and the hepatocellular apoptosis ratio might both be increased because of overperfusion after portal vein arterialization[6]. The overperfusion of arterial blood into the liver via the portal vein might cause certain harmful effects; in particular, increased risk of liver cirrhosis[7]. Partial portal vein arterialization or blood flow restriction after total portal vein arterialization might be used as prophylaxes, and these techniques play important roles in maintaining the normal physiological function of transplanted livers[8]. Portal vein arterializations might also cause portal venous system blood stasis. This effect might increase upper gastrointestinal bleeding after transplantation. Portacaval or mesocaval shunts might be able to remit this condition. Portal vein arterializations result in acceptable survival rates with regard to spontaneous outcomes among patients with completely de-arterialized livers. Managing complications (especially pulmonary hypertension) after the procedure is challenging. Portal vein arterialization might represent a salvage option or a bridge to liver re-transplantation, thereby enabling curative resections for locally advanced HPB cancers with vascular involvement[9].
Generally, the results of portal vein arterialization performed on the current patients suggested that this technique is an effective treatment for liver transplantation patients with portal vein reconstruction difficulties (e.g., extensive portal thrombosis, portal venous cavernous transformation and decreased portal vein perfusion); however, we should also pay close attention to preventing postoperative complications.
Liver transplantations were performed on two patients with hepatic failure caused by liver cirrhosis.
Please summarize pathological methods and major findings in one sentence.
The hepatic artery of the first donor was anastomosed end-to-end with the gastroduodenal artery of the first recipient; meanwhile, the portal vein of the second donor was simultaneously anastomosed end-to-end with the common hepatic artery of the second recipient.
The blood flow of the portal vein, the perfusion of the donor liver and liver function were satisfactory after surgery. Portal vein arterialization might be an effective treatment for patients whose portal vein reconstruction was difficult.
This is an important contribution to the literature. It adds two more case reports to the literature of a rarely done procedure. The authors have included caval portal hemianastomosis and vein interpositions.
P- Reviewer: Juntermanns B, Sugawara Y, Ramsay M S- Editor: Gou SX L- Editor: Stewart G E- Editor: Liu XM
| 1. | Tzakis AG, Kirkegaard P, Pinna AD, Jovine E, Misiakos EP, Maziotti A, Dodson F, Khan F, Nery J, Rasmussen A. Liver transplantation with cavoportal hemitransposition in the presence of diffuse portal vein thrombosis. Transplantation. 1998;65:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 129] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Charco R, Margarit C, López-Talavera JC, Hidalgo E, Castells L, Allende H, Segarra A, Moreíras M, Bilbao I. Outcome and hepatic hemodynamics in liver transplant patients with portal vein arterialization. Am J Transplant. 2001;1:146-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Shen S, Zhang X, Wang W, Yu K, Wang Z, Yan J. Study on partial portal arterializations in hepatectomy. Zhonghua Shiyan Waike Zazhi. 2000;17:235-236. |
| 4. | Yin Q, Miao X, Tang K. An experimental study on the effects of partial arterialization of portal vein on the liver of rats after partial hepatectomy. Zhonghua Putong Waike Zazhi. 2006;15:23-25. |
| 5. | Schleimer K, Stippel DL, Kasper HU, Prenzel K, Gaudig C, Tawadros S, Hoelscher AH, Beckurts KT. Portal vein arterialization increases hepatocellular apoptosis and inhibits liver regeneration. J Surg Res. 2008;149:250-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Schleimer K, Stippel DL, Kasper HU, Tawadros S, Allwissner R, Gaudig C, Greiner T, Hölscher AH, Beckurts KT. Portal hyperperfusion causes disturbance of microcirculation and increased rate of hepatocellular apoptosis: investigations in heterotopic rat liver transplantation with portal vein arterialization. Transplant Proc. 2006;38:725-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Chen Y, Huang Z, Huang J, Wang Y, Zhao J. An experimental study on hilar en bloc resection and reconstruction of hepatic blood flow with arterializations of portal vein in rats with obstructive jaundicre. Zhonghua Putong Waike Zazhi. 2001;16:94-96. |
| 8. | Li W, Li B, Gao L, Zhang A, Wan T, Chen Y, Huang Z. Long-term effect of flow-restricted portal vein Arterialization on rat’s liver structures and function. Zhonghu Putong Waike Zazhi. 2006;21:55-58. |
| 9. | Bhangui P, Salloum C, Lim C, Andreani P, Ariche A, Adam R, Castaing D, Kerba T, Azoulay D. Portal vein arterialization: a salvage procedure for a totally de-arterialized liver. The Paul Brousse Hospital experience. HPB (Oxford). 2014;16:723-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |