Published online Sep 14, 2014. doi: 10.3748/wjg.v20.i34.12341
Revised: April 9, 2014
Accepted: April 21, 2014
Published online: September 14, 2014
Processing time: 221 Days and 22.6 Hours
Benign duodenal tumors are rare and less common than malignant tumors. Furthermore, vascular lesions of the duodenum, including hemangiomas, are rare causes of gastrointestinal bleeding. This report describes a case with bleeding hemangiomas in the third portion of the duodenum and jejunum and their successful treatment using a laparoscopic approach. There is no report of totally laparoscopic resection for tumor in the third portion of duodenum. After performing a laparoscopic Kocher maneuver, the location of the duodenal hemangioma was confirmed by endoscopic and laparoscopic observation. The lesion was excised using ultrasonic coagulating shears and the defect in the duodenal wall was sutured laparoscopically. The hemangioma of the jejunum was treated extracorporeally through a 3.0 cm umbilical incision. The operating time was 241 min and blood loss was negligible. The postoperative course was uneventful. For benign duodenal tumors in the third portion, if endoscopic resection is not adapted, this less invasive technique may be a standard treatment.
Core tip: This report describes a case with bleeding hemangiomas in the third portion of the duodenum and successful treatment using a laparoscopic approach. After performing a laparoscopic Kocher maneuver was performed, the location of the duodenal hemangioma was confirmed by endoscopic and laparoscopic observation. The lesion was excised using ultrasonic coagulating shears and the defect in the duodenal wall was sutured laparoscopically. This minimally invasive technique may be a valid alternative to open surgery for the treatment of benign duodenal tumors in the third portion.
- Citation: Kanaji S, Nakamura T, Nishi M, Yamamoto M, Kanemitu K, Yamashiita K, Imanishi T, Sumi Y, Suzuki S, Tanaka K, Kakeji Y. Laparoscopic partial resection for hemangioma in the third portion of the duodenum. World J Gastroenterol 2014; 20(34): 12341-12345
- URL: https://www.wjgnet.com/1007-9327/full/v20/i34/12341.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i34.12341
Vascular lesions of the duodenum, including hemangiomas, are rare causes of gastrointestinal bleeding. Indeed, there have been very few reports of hemangioma in the duodenum[1]. Considering that hemangiomas are benign tumors, a less invasive procedure, such as endoscopic or laparoscopic resection, is recommended if it is technically possible. The use of endoscopic mucosal resection (EMR) for intestinal tumors, including duodenal tumors, has increased. However, EMR of duodenal tumors is challenginge due to the presence of a thin duodenal wall and rich vascularity. Recently, laparoscopic treatments for duodenal tumors have been reported to reduce invasiveness[2-6]. However, most of these reports concerned tumors in the proximal side of duodenum. To the best of our knowledge, this is the first report of a patient undergoing total laparoscopic resection for a tumor in the third portion of the duodenum. In this paper, we present a minimally invasive surgical option for resection of a duodenal hemangioma: total laparoscopic resection without mini-laparotomy.
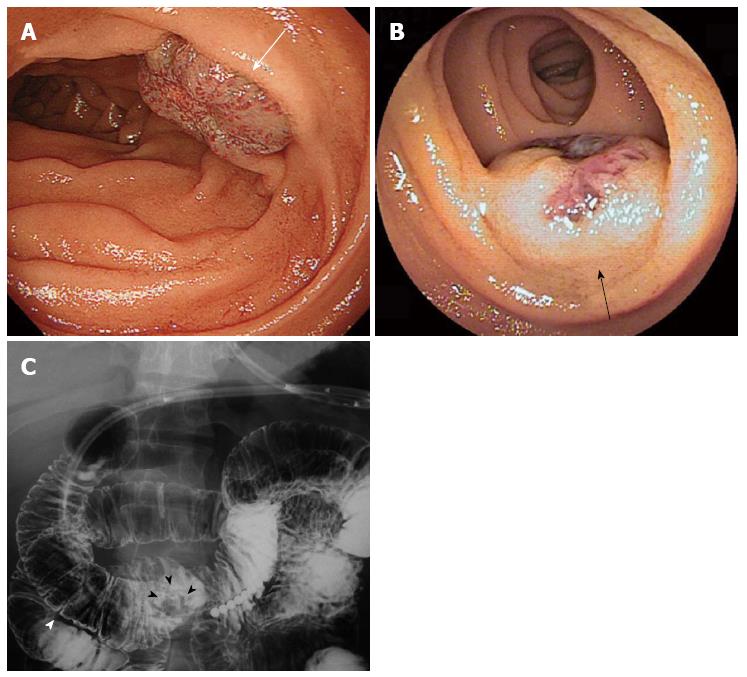
In 2013, a 43-year-old male presented with anemia and a hemoglobin level of 10.0 g/dL. He was diagnosed with a hemangioma in the third portion of the duodenum by upper gastrointestinal endoscopy (Figure 1A) and a hemangioma in the middle part of the jejunum by double balloon endoscopy (DBE) (Figure 1B). Despite the absence of active bleeding, these hemangiomas were suspected to be the cause of his anemia because they bled easily following light contact with the endoscope and no sign of any other cause of bleeding was found during further examination, including capsule endoscopy and colonoscopy. At the time of diagnosis, endoscopic examination showed the diameters of both tumors to be 20 mm. Because these suspected hemangiomas bled easily, a definite diagnosis was not made from biopsy specimens. The duodenal hemangioma was located in the third portion of the duodenum based on a barium study, approximately 4.0 cm to the anal side of the inferior flexure of the duodenum and approximately 7.0 cm away from the ampulla of Vater (Figure 1C). Computed tomography could not detect tumors in the duodenum or jejunum. Distant metastasis and regional lymph node swelling were absent. These tumors could not be subjected to EMR because of their locations, where endoscopic treatment posed technical difficulties. The patient was referred to surgery due to his desire for minimally invasive treatment rather than conservative observation. Finally, the patient decided to undergo laparoscopic resection of the tumor. To identify the location of the hemangioma in the jejunum during surgery, the jejunal submucosal layer against the side of the hemangioma was marked with black ink during DBE prior to the surgery.
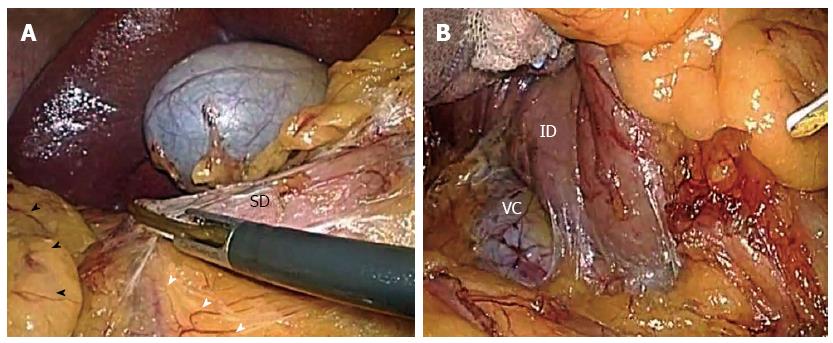
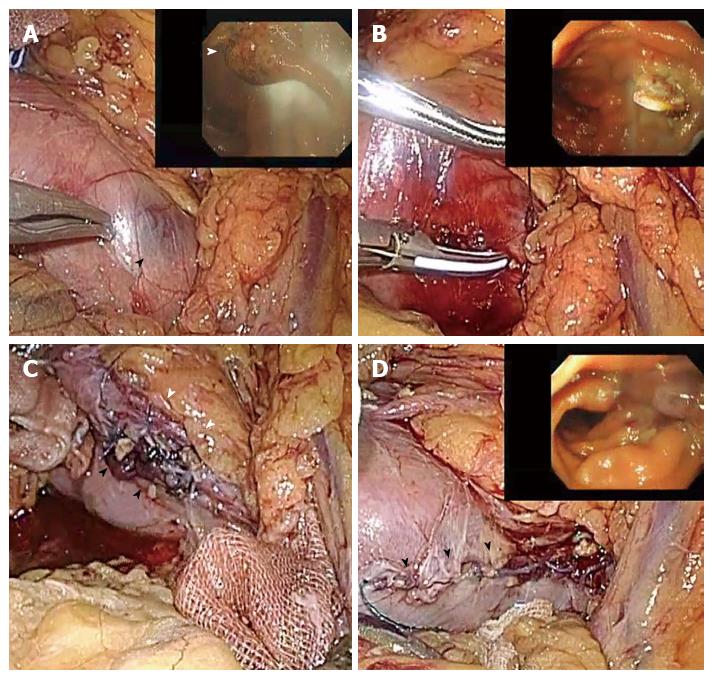
A laparoscopic operation was undertaken under general anesthesia with the patient in the supine position with his legs apart. The operator stood on the patient’s left side. Initially, the first trocar was placed using a standard umbilical cut down technique. Carbon dioxide was insufflated through this port with a pressure setting of 10 mmHg. A 30° laparoscope was introduced through the umbilical port and diagnostic laparoscopy was performed. Four additional trocars were inserted into the left upper, right upper, right lower, and left lower quadrants under laparoscopic guidance. Initially, we dissected the omentum from the right lateral side up to the front of duodenum and removed the mesocolon from the epigastric tissue. The procedure continued with dissection of the right hepatocolic ligament, with ultrasonic coagulating shears (SonoSurg, Olympus Medical System, Tokyo, Japan) being used to mobilize the right colic flexure (Figure 2A). A laparoscopic Kocher maneuver was then performed. The decision regarding the resection procedure was based on the preoperative imaging studies and on intraoperative visual inspection. The retroperitoneum was entered using the ultrasonic coagulating shears, and the dissection around the second portion of the duodenum was extended beyond the vena cava (Figure 2B). Next, the surgeon moved on the patient’s right side, and additional dissections of the mesocolon were performed around the duodenum without any management of the vessels, enabling exposure of the third portion of the duodenum. Because the serosal side of the hemangioma became dark red, we were able to identify the location of the hemangioma from the serosal side. The hemangioma was located in the third portion of the duodenum, approximately 4.0 cm from the anal side of the inferior flexure of the duodenum, as predicted by the preoperative findings. We performed an intraoperative gastroduodenal endoscopy and observed that the intraluminal location of the hemangioma corresponded with that identified by laparoscopy, based on the serosal color change of the duodenum (Figure 3A). Resection of the lesion was performed using ultrasonic coagulating shears. Next, we cut a full-thickness layer of the gastric wall using laparoscopic coagulating shears, while confirming the location of the tumor by endoscopy (Figure 3B). The duodenal wall was then closed with a manual intracorporeal running suture using a 3-0 vicryl suture (Erhicon GMbH, Norderstedt, Germany) in the full-thickness layer (Figure 3C) and 3-0 V-Loc (Covidien, Dublin, Ireland) in the seromuscular layer (Figure 3D).
The resected specimen was transferred into a pouch made from the finger tip of a rubber glove, and was removed through the left lower port. After the incision in the duodenum was repaired, the duodenum was reinflated to detect any bleeding or leakage from the suturing line of the laparoscopy and to confirm a patent lumen by intraluminal endoscopy.
Next, we extended the navel port from 1.5 to 3.0 cm to extracorporeally check the total jejunum through this port. We easily identified the location of the hemangioma in the jejunum, which had been detected preoperatively and marked with black ink before surgery; the hemangioma was also checked by palpation of the tumor through the serosal side. The jejunal hemangioma was located approximately 250 cm from the anal side of the Treitz’ ligament. No abnormal finding was observed elsewhere in the jejunum.
The duration of the procedure was 241 min, and blood loss was negligible. Postoperative pain was minimal, requiring no additional analgesia beyond the continuous epidural anesthesia. The patient was ambulatory the next day. He was started on a liquid diet, which proceeded to a soft diet. The resected specimens demonstrated a 15 mm × 8 mm duodenal tumor and a 15 mm × 11 mm jejunal tumor, both having a solid structure. Microscopic examination of both tumors also revealed hemangiomas, while no abnormal structure or dysplasia was observed. The patient was able to eat as well as he did before the operation and all symptoms, including the anemia, were resolved.
Recently, several investigators have reported the laparoscopic local excision of duodenal tumors[2,3,6-8]. Poultsides et al[8] reported hand-assisted laparoscopic local duodenal resection was associated with shorter operative time compared to the total laparoscopic approach. However, the hand-assisted approach necessitates that the mini-laparotomy incision reach a length of at least 60-70 mm. Furthermore, extracorporeal duodenal resection and closure is conducted in a limited working space with restricted vision, thus making it difficult especially on obese patients.
There is no report of a total laparoscopic resection performed for a tumor in the third portion of the duodenum. Because of the technical difficulty of the location of the tumor, which would be surrounded by the pancreas, transverse colon, and mesocolon, it seems that benign duodenal tumors in the third portion have been resected using laparoscope-assisted approaches or open laparotomy. Laparoscopic resection of tumors in the third portion of the duodenum requires special operative techniques, which are important in overcoming this difficult location.
First, the laparoscopic bilateral approach to the Kocher maneuver was useful in this study, that is, the dissection around the duodenum was performed for the second portion on the patient’s left side and for the third portion on his right side. We consider that the laparoscopic Kocher maneuver is an indispensable approach to achieving total laparoscopic resection of duodenal tumors in the second and third portion as it can mobilizes and exposes the duodenum prior to local excision and closure of the defect. The tumor, described in this study, located in the third portion of the duodenum, was approximately 4 cm to the anal side of the inferior flexure of the duodenum and was easily exposed by the laparoscopic Kocher maneuver with a bilateral approach.
Second, the laparo-endoscopic view was useful for identifying the tumor-free margin. During resection of the tumor, the ultrasonic coagulating shears were useful for coagulating and cutting the duodenal wall. The laparo-endoscopic view enabled resection of the duodenal tumor with suitable margins through observation of both the mucosal and serosal sides of the tumor. Furthermore, we placed an anchoring suture on the side of the duodenal tumor with greater curvature, which was then rolled caudally to facilitate resection.
Lastly, closing of the duodenal defect by laparoscopic suturing was necessary in this case, because the tumor was extremely closed (approximately 5 mm) to the pancreas, providing an unsuitable axis for the endolinear stapler to close the duodenal wall. Duodenal resection using an endolinear stapler has been reported by other investigators[2,3]. Toyonaga et al[3] used an endolinear stapler for wedge resection of a relatively small carcinoid tumor. Because this is a simple and safe procedure, laparoscopic intestinal resection using an endolinear stapler is useful. However, an unnecessarily large resection margin is a problem when using an endolinear stapler. In this case, it was quite straightforward to carry out intracorporeal suturing with a magnified laparoscopic view. Leakage from a duodenal defect may be critical because duodenal juice contains pancreatic secretions and bile. For increased safety, we sutured the duodenal defect with two layers using a laparo-endoscopic view, while paying close attention to avoiding any stenosis or deformity. This technique of laparoscopic suturing is widely applicable, such that a duodenal tumor in any location can be treated by a totally laparoscopic approach.
Here, we preoperatively detected two hemangiomas in the duodenum, and jejunum by endoscopic examination. Because no active bleeding from these hemangiomas was observed endoscopically, there was the possibility that another hemangioma was the cause of the bleeding in the digestive tract, which could not be detected preoperatively. Suzuki et al[9] reported that the diagnostic rate of DBE in identifying the source of bleeding (79%) was much higher than that of conventional methods (11%), such as upper gastrointestinal endoscopy, colonoscopy, or barium enema. Despite the preoperative DBE, we carefully checked the jejunum by both visual examination and palpation through the 3.0 cm navel wound. However, it was not possible for the resection of the duodenal hemangioma to be performed safely through this small, 3.0 cm opening. We consider that total laparoscopic partial resection is a viable approach for tumors in deep or fixed abdominal organs, such as the duodenum and stomach, but not for certain parts of the jejunum that can be accessed and resected easily through a 3.0 cm opening.
In conclusion, our technique of total laparoscopic resection with intracorporeal suturing under a laparo-endoscopic view constitutes a minimally invasive treatment for benign tumors in the third portion of the duodenum.
A 43-year-old male presented with anemia and a hemoglobin level of 10.0 g/dL.
Bleeding hemangioma in the third portion of the duodenum.
Other gastrointestinal bleeding.
He was diagnosed with a hemangioma in the third portion of the duodenum by upper gastrointestinal endoscopy.
Microscopic examination of the tumor revealed hemangiomas, and no abnormal structure or dysplasia was observed.
Totally laparoscopic partial resection for hemangioma in the third portion of the duodenum.
For the benign duodenal tumors in the third portion, if endoscopic resection is not adapted, this less invasive technique may be a standard treatment.
Authors described a clear technique for totally laparoscopic resection of duodenal tumor in the third portion.
P- Reviewer: Ciaccio EJ, Fernandez-Pineda I, Mais V, Richardson WS S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Nishiyama N, Mori H, Kobara H, Fujihara S, Nomura T, Kobayashi M, Masaki T. Bleeding duodenal hemangioma: morphological changes and endoscopic mucosal resection. World J Gastroenterol. 2012;18:2872-2876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Adell-Carceller R, Salvador-Sanchís JL, Navarro-Navarro J, Segarra-Soria M, García-Calvo R, Gibert-Gerez J, Colom-Costa J. Laparoscopically treated duodenal hamartoma of Brunner’s glands. Surg Laparosc Endosc. 1997;7:298-300. [PubMed] |
| 3. | Toyonaga T, Nakamura K, Araki Y, Shimura H, Tanaka M. Laparoscopic treatment of duodenal carcinoid tumor. Wedge resection of the duodenal bulb under endoscopic control. Surg Endosc. 1998;12:1085-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Cheah WK, Lenzi JE, Chong S, Goh PM. Laparoscopic excision of duodenal tumors. Surg Endosc. 2001;15:898. [PubMed] |
| 5. | Rosen M, Zuccaro G, Brody F. Laparoscopic resection of a periampullary villous adenoma. Surg Endosc. 2003;17:1322-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Orsenigo E, Di Palo S, Vignali A, Staudacher C. Laparoscopic excision of duodenal schwannoma. Surg Endosc. 2007;21:1454-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Lee JH, Han HS, Kim YW, Min SK, Lee HK. Laparoscopic wedge resection with handsewn closure for gastroduodenal tumors. J Laparoendosc Adv Surg Tech A. 2003;13:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Poultsides GA, Pappou EP, Bloom GP, Orlando R. Hybrid resection of duodenal tumors. J Laparoendosc Adv Surg Tech A. 2011;21:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Suzuki T, Matsushima M, Okita I, Ito H, Gocho S, Tajima H, Tokiwa K, Teraoka H, Watanabe K, Shirai T. Clinical utility of double-balloon enteroscopy for small intestinal bleeding. Dig Dis Sci. 2007;52:1914-1918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |