Published online Sep 7, 2014. doi: 10.3748/wjg.v20.i33.11910
Revised: March 19, 2014
Accepted: April 21, 2014
Published online: September 7, 2014
Processing time: 220 Days and 16 Hours
Endoscopic submucosal dissection (ESD) of large gastric lesions often leads to severe gastric strictures, especially in cases of large ESD in the antrum of the stomach. It has recently been reported that balloon dilation, mucosal incision, and local steroid injections can successfully treat gastric strictures. However, there are some complications with existing methods and decreasing the quality of life. We have developed a novel method to prevent severe gastric strictures that does not involve balloon dilation, mucosal incision, or steroid injections after circumferential ESD. Our original method involves the submucosal injection of a mixed solution composed of triamcinolone acetonide and a general solution of glycerol, hyaluronic acid, and a small amount of indigo carmine and epinephrine during the ESD procedure; this mixture is called a mixed solution of triamcinolone (MST). According to standard ESD procedures, several milliliters of MST are injected into the submucosal layer for the purpose of elevating the submucosa during ESD resulting in prevention of severe strictures. Our method using MST take several advantages such as MST method suppress inflammation in ulcer from initial phase, prevention of stricture without obstructive symptoms, and does not require several ballooning. Therefore, MST method is safe and gentle, shorten the hospitalization duration. Here, we described two cases in which we prevented severe strictures of the gastric antrum after completing a circumferential ESD using MST without any complications.
Core tip: Endoscopic submucosal dissection (ESD) leads to severe gastric strictures, especially in cases of large ESD in the antrum of the stomach. It has recently been reported that some methods can treat gastric strictures, however there are some limitations. We have developed a novel method to prevent severe gastric strictures that does not involve previous methods. Our original method involves the submucosal injection of a mixed solution composed of triamcinolone acetonide and a general solution during the ESD procedure. Here, we described two cases in which we prevented severe strictures of the gastric antrum after ESD using our original method without any complications.
- Citation: Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Matsunaga T, Ayaki M, Yachida T, Oryu M, Masaki T. Novel method to prevent gastric antral strictures after endoscopic submucosal dissection: Using triamcinolone. World J Gastroenterol 2014; 20(33): 11910-11915
- URL: https://www.wjgnet.com/1007-9327/full/v20/i33/11910.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i33.11910
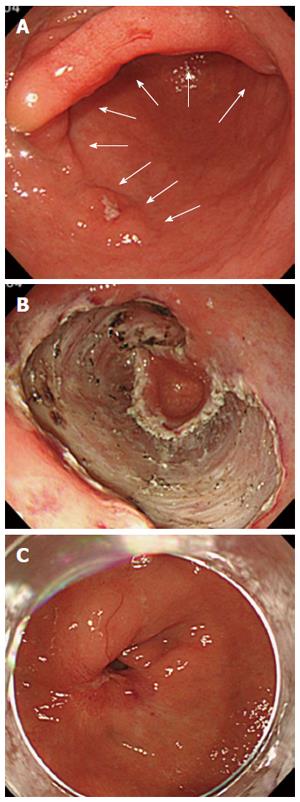
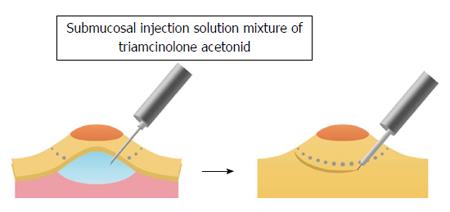
Endoscopic submucosal dissection (ESD) was developed to enable the en bloc removal of large gastric cancers while decreasing the risk of local recurrences and allowing the collection of sufficient specimens for an accurate histopathological evaluation. The ESD procedure is associated with a high incidence of stenosis in both the esophagus and stomach. In addition, strictures after ESD have frequently been described in esophageal lesions[1,2]. However, so far, there have been only a few reports of strictures after ESD in the stomach[3-8]. Previous it has been reported that the extent of a circumferential mucosal defect of > 3/4 in both the antrum and cardia is a relevant factor for gastric stenosis after ESD[6-8]. We have treated the cases of severe stenosis in the antrum after ESD, and the circumferential extents of the mucosal defects were > 3/4 (Figure 1A-C). In such cases, we have had to rely upon endoscopic balloon dilation[3,6-8] and local steroid injection[4,5]. Recently, the efficacy of balloon dilation and local steroid injection for the prevention and treatment of post-ESD strictures has been described for the esophagus and stomach[1-8]. However, several additional endoscopic procedures after ESD were required when using such methods resulting in additional costs, patient inconveniences, and increased rates of perforation[3]. Therefore, we considered a new method involving submucosal injection of a mixed solution composed of triamcinolone acetonide (Kenacort: 50 mg/5 mL; Bristol-Meyers Squibb Co. Tokyo, Japan) 8 mL, glycerol 16 mL, hyaluronic acid 16 mL, and a small amount of indigo carmine and epinephrine: this mixture is to be administered during the ESD procedure. This mixture is called a mixed solution of triamcinolone (MST). The lesions were treated with standard ESD procedure using a dual knife (KD-650L; Olympus Co., Tokyo, Japan) and an IT2 knife (KD-611L; Olympus Co., Tokyo, Japan). According to the standard ESD procedure, several milliliters of MST was injected into the submucosal layer just beneath the lesion for the purpose of elevating the submucosa. Thus, we were able to equally permeate the steroids into the remaining submucosa of the dissected ulcer defect (Figure 2).
This mixed steroid injection method was able to suppress inflammation at early phase immediately after ESD procedure. We treated two patients with mucosal gastric cancer using circumferential ESD in the antrum. The circumferential extents of the mucosal defects were > 3/4 in the antrum of the stomach. We administered MST injections into the submucosal layer as treatment. Two months later, there were no severe strictures or gastric outlet obstructions after ESD procedure, even in the absence of balloon dilation or further steroid injections.
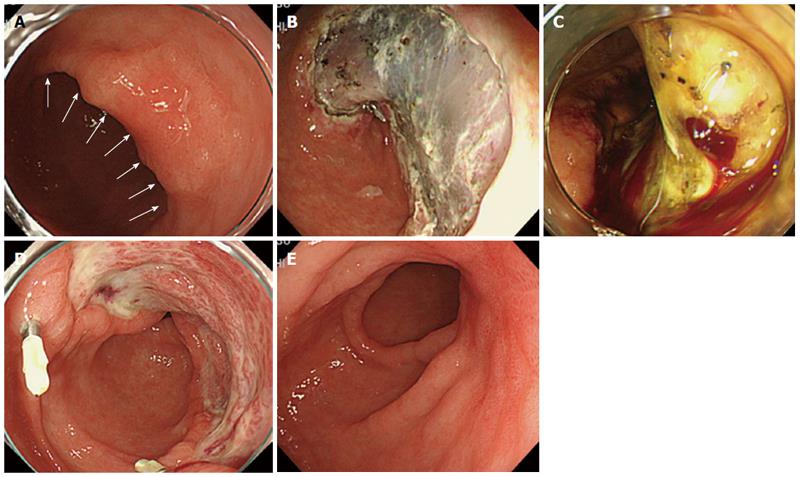
A 63-year-old man was admitted to our hospital for early gastric cancer diagnosed by a previous esophagogastroduodenoscopy (EGD) examination. The lesion was a semi-circumferential, laterally spreading type 0-IIc early gastric cancer on the posterior wall of the antrum (Figure 3A). We assumed that the circumferential extent of the mucosal defect would be > 3/4 in the antrum of the stomach after ESD. Informed consent was obtained from the patient before ESD operation as required by our Hospital Clinical Ethics Committee. The lesion was initially treated by the standard ESD procedures. During ESD, a mixture of triamcinolone acetonide 8 mL, glycerol 16 mL, hyaluronic acid 16 mL, and a small amount of indigo carmine and epinephrine was injected into the submucosal layer just beneath the lesion.
The total dose of triamcinolone acetonide injection was 60 mg. Three-fourths circumferential section of mucosa in the antrum was removed (Figure 3B). The day after the ESD operation, there was abundant vascularization in the ulcer area more than in patients with a normal ESD procedure without MST injection (Figure 3C). Two weeks after the ESD operation, there was more granulation tissue than usual in ESD ulcers site (Figure 3D). Three months after the ESD operation, the ulcer entered into a healing stage, and no strictures developed concomitant with the healing process near the ESD ulcer site (Figure 3E). No complications, including nausea or vomiting developed following the ESD procedure.
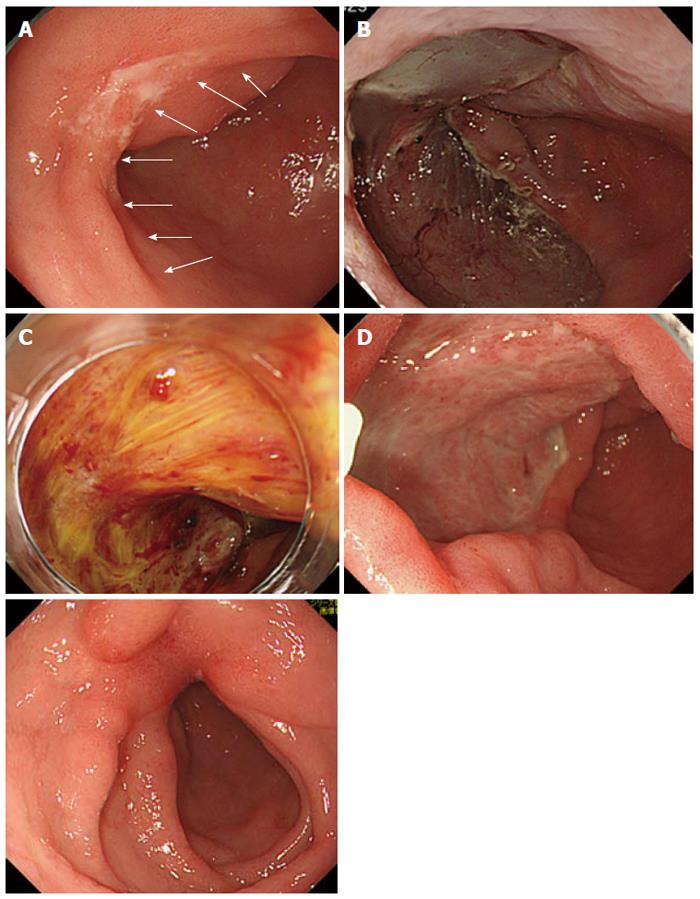
A 61-year-old man was admitted to our hospital for early gastric cancer diagnosed by a previous EGD examination. The lesion was a one-third circumferential, laterally spreading type 0-IIc early gastric cancer on the anterior wall of the antrum (Figure 4A). We predicted that the circumferential extent of the mucosal defect would be > 3/4 in the antrum of the stomach after ESD. After obtaining informed consent, we used the same steroids as those used in Case 1 during the ESD. The total injected dose of triamcinolone acetonide was 40 mg. A three-fourths circumferential mucosa in the antrum was removed (Figure 4B). The day after the ESD, there was more abundant vascularization in the ulcer than usual (Figure 4C). Two weeks after the ESD operation, there was also more granulation tissue than usual in ESD ulcers site (Figure 4D). Three months after the ESD operation, the ulcer had entered a healing stage, and there were no strictures concomitant with the healing process near the ESD ulcer (Figure 4E). No nausea or vomiting occurred during these three months, and no other complications occurred following the ESD procedure.
Based on our initial experience with injecting MST during ESD procedure, this method appears to be effective for preventing severe gastric strictures without balloon dilation, mucosal incision, or steroid injections after circumferential ESD treatment.
It has been reported that steroid injections can prevent strictures after ESD for esophageal cancer and can lower the number of endoscopic balloon dilation sessions[1]. ESD scar formation is thought to be an integral part of wound healing, a process that involves inflammation, proliferation, and remodeling. Strictures develop due to the crosslinking of collagen. Steroid injections can induce the regression of scars by suppressing inflammation and reducing collagen and fibroblast proliferation. Because the inflammatory process starts immediately after the ESD procedure, it is necessary to use steroids as soon as possible to suppress excess inflammation[1,2,5,9,10].
One advantage of our novel method is that it allows us to inject steroids into the submucosal layer just beneath the lesion during the ESD procedure. This direct application reduces the level of inflammation resulting from the initial phase. Previous reports have indicated that balloon dilation can treat strictures of the gastric antrum that develop after circumferential ESD treatment is performed[3,6-8]. However, out of four patients who underwent a step-series endoscopic balloon dilatation, two of them experienced gastric perforation (50% incidence of perforation)[3]. Therefore, balloon dilation may be one option, but its use should be limited due to its associated complications. Moreover, ballooning methods must be performed several times after the ESD, resulting in a longer hospitalization time due to the serial endoscopies that must be performed and decreasing the patient’s quality of life. As our MST method does not require ballooning, therefore it is safer and gentler than the ballooning method. In fact, our two patients were only hospitalized for 7 d following the ESD procedure, a length similar to that for standard ESDs. We also summarized possible advantages and disadvantages of MST method with other existing methods in Table 1.
| Methods | Advantages | Disadvantages |
| Balloon dilatation | Technical easy | Perforation |
| Longer hospitalization | ||
| Require several endoscopies | ||
| Treatable after obstructive symptoms | ||
| Incision and steroid injection | Suppress inflammation of ulcer | Technical difficult |
| Safe | Longer hospitalization | |
| Treatable after obstructive symptoms | ||
| Mixed solution of triamcinolone method | Suppress inflammation of ulcer from initial phase | Delayed bleeding (abundant vascular) |
| Shorter hospitalization | ||
| Safe and gentle | ||
| Prevention of stricture |
Recently, our colleague reported that mucosal incisions and local steroid injections were effective in treating stenosis of the gastric antrum after circumferential ESD[4]; we also consider this approach effective. However, this method has challenges associated with the injection of triamcinolone into the submucosal layer within the ulcer after the ESD and is also accompanied by the possibility of perforations, similar to esophageal cases[11]. Thus, to address these issues, we developed the present MST procedure, which is more gentle and convenient than previous methods.
Furthermore, previous methods have been able to treat strictures only after complaints of obstructive symptoms or after severe stricture have occurred, while our MST can prevent strictures in the antrum after circumferential ESD. Although the use of steroids delays the healing of ulcers after ESD, they minimize severe deformities and strictures. However, due to the induction of abundant vascularization, as shown in our two cases (Figures 3C, 4C); care must be taken to detect any delayed bleeding for at least 7 d after ESD procedure.
Additional experience with our method is still needed. Currently, a comparative prospective study including a large number of cases is on-going at our hospital.
If the circumferential extent of a mucosal defect is > 3/4 at the antrum of the stomach after ESD procedure, MST injection during ESD procedure is to be an effective and convenient method to prevent strictures without steroid injection alone and performance of ballooning.
Case-1 was a 63-year-old man was admitted to our hospital for early gastric cancer, who had a semi-circumferential, laterally spreading type 0-IIc early gastric cancer on the posterior wall of the antrum. Case-2 was a 61-year-old man was admitted to our hospital for early gastric cancer, who had a one-third circumferential, laterally spreading type 0-IIc early gastric cancer on the anterior wall of the antrum.
Authors have developed a novel method to prevent severe gastric strictures that does not involve previous methods. Their original method involves the submucosal injection of a mixed solution composed of triamcinolone acetonide and a general solution during the Endoscopic submucosal dissection (ESD) procedure.
It has recently been reported that balloon dilation, mucosal incision, and local steroid injections can successfully treat gastric strictures. However, there are some complications with existing methods and decreasing the quality of life.
Their original method involves the submucosal injection of a mixed solution composed of triamcinolone acetonide and a general solution of glycerol, hyaluronic acid, and a small amount of indigo carmine and epinephrine during the ESD procedure; this mixture is called a mixed solution of triamcinolone (MST).
If the circumferential extent of a mucosal defect is > 3/4 at the antrum of the stomach after ESD procedure, we consider MST to be an effective and convenient method to prevent strictures without steroid injection alone and performance of ballooning.
Additional experience with this method would be needed to find out any severe side-effects in clinic.
P- Reviewer: Ji JF, Li QQ S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Hanaoka N, Ishihara R, Takeuchi Y, Uedo N, Higashino K, Ohta T, Kanzaki H, Hanafusa M, Nagai K, Matsui F. Intralesional steroid injection to prevent stricture after endoscopic submucosal dissection for esophageal cancer: a controlled prospective study. Endoscopy. 2012;44:1007-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 195] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 2. | Hashimoto S, Kobayashi M, Takeuchi M, Sato Y, Narisawa R, Aoyagi Y. The efficacy of endoscopic triamcinolone injection for the prevention of esophageal stricture after endoscopic submucosal dissection. Gastrointest Endosc. 2011;74:1389-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Tsunada S, Ogata S, Mannen K, Arima S, Sakata Y, Shiraishi R, Shimoda R, Ootani H, Yamaguchi K, Fujise T. Case series of endoscopic balloon dilation to treat a stricture caused by circumferential resection of the gastric antrum by endoscopic submucosal dissection. Gastrointest Endosc. 2008;67:979-983. [PubMed] |
| 4. | Mori H, Kobara H, Fujihara S, Nishiyama N, Rafiq K, Masaki T. Recanalization of severe gastric antral stricture after large endoscopic submucosal dissection: mucosal incision and local steroid injection. J Gastrointestin Liver Dis. 2012;21:435-437. [PubMed] |
| 5. | Mori H, Rafiq K, Kobara H, Fujihara S, Nishiyama N, Kobayashi M, Himoto T, Haba R, Hagiike M, Izuishi K. Local steroid injection into the artificial ulcer created by endoscopic submucosal dissection for gastric cancer: prevention of gastric deformity. Endoscopy. 2012;44:641-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Hagiwara S, Onozato Y, Iizuka H, Sohara N, Ishihara H, Kakizaki S, Ogawa T, Tomizawa N, Itoh H. Gastric stricture after endoscopic submucosal dissection for early gastric cancers. Progress Digest Endosc. 2010;77:35-39. |
| 7. | Iizuka H, Kakizaki S, Sohara N, Onozato Y, Ishihara H, Okamura S, Itoh H, Mori M. Stricture after endoscopic submucosal dissection for early gastric cancers and adenomas. Dig Endosc. 2010;22:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 8. | Coda S, Oda I, Gotoda T, Yokoi C, Kikuchi T, Ono H. Risk factors for cardiac and pyloric stenosis after endoscopic submucosal dissection, and efficacy of endoscopic balloon dilation treatment. Endoscopy. 2009;41:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835-870. [PubMed] |
| 10. | Carrico TJ, Mehrhof AL, Cohen IK. Biology of wound healing. Surg Clin North Am. 1984;64:721-733. |