Published online Jul 14, 2014. doi: 10.3748/wjg.v20.i26.8717
Revised: April 23, 2013
Accepted: May 18, 2013
Published online: July 14, 2014
Processing time: 527 Days and 23.2 Hours
Xanthogranulomatous inflammation (XGI) is a disease of unknown origin, most frequently described in the kidney and gallbladder; its localization in the colorectal tract is extremely rare. The extension of the typical inflammatory process to the surrounding tissues may lead to misdiagnosis as cancer. We report the case of a 56-year-old woman presenting to the Emergency Department with pain, increased levels of α1 and α2 proteins and C-reactive protein (17.5 mg/dL; normal value 0-0.5), and a palpable mass, localized in the right lower quadrant of the abdomen. A computed tomography scan showed a large right cecal mass with necrotic areas, local inflammation of retroperitoneal fat, and enlargement of local lymph nodes. Because of the high suspicion of colic abscess as well as malignancy and worsening of the clinical condition, the patient underwent right colectomy after 4 d of antibiotic treatment. Pathology revealed xanthogranulomatous inflammation involving the ileocecal valve. We review the reports of large bowel tract XGI in the international literature.
Core tip: Xanthogranulomatous inflammation (XGI) is a disease of unknown origin, most frequently described in the kidney and gallbladder, and extremely rare in the colon. The extension of inflammation to the surrounding tissues may lead to misdiagnosis as cancer. We report the case of a 56-year-old woman presenting to the Emergency Department with pain, increased levels of acute-phase proteins, and a palpable mass in the right lower abdominal quadrant. Computed tomography showed a large cecal mass with necrotic areas and enlarged lymph nodes. Due to suspicion of malignancy and worsening of the clinical conditions, she underwent right colectomy. Pathology revealed XGI of the ileocecal valve.
- Citation: Chieco PA, Antolino L, Giaccaglia V, Centanini F, Cunsolo GV, Sparagna A, Uccini S, Ziparo V. Acute abdomen: Rare and unusual presentation of right colic xanthogranulomatosis. World J Gastroenterol 2014; 20(26): 8717-8721
- URL: https://www.wjgnet.com/1007-9327/full/v20/i26/8717.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i26.8717
Xanthogranulomatous inflammation (XGI) is a rare pathologic entity with characteristic macroscopic and microscopic features. Typical histologic findings are: aggregation of lipid-laden foamy macrophages accompanied by giant cells, few plasma cells and lymphocytes leading to parenchymal destruction[1]. XGI is an uncommon entity that can involve any organ, and the most common reported sites are the kidney and gallbladder. Other described rare localizations are: epididymis, ovary, fallopian tube, endometrium, thyroid, adrenal gland, appendix, lymph nodes, lung, bone, soft tissue, and skin[2]. The large bowel has rarely been involved in the xantogranulomatous process, with only a few reports in the international literature[2-6]. It is often difficult to differentiate the lesion from an infiltrative cancer because XGI frequently presents as a mass-like lesion with an extension of fibrosis and inflammation to the surrounding tissues mimicking an advanced neoplasia. We report the case of a middle-aged woman suffering from a right colic XGI mimicking a malignant tumor or an abscess mass.
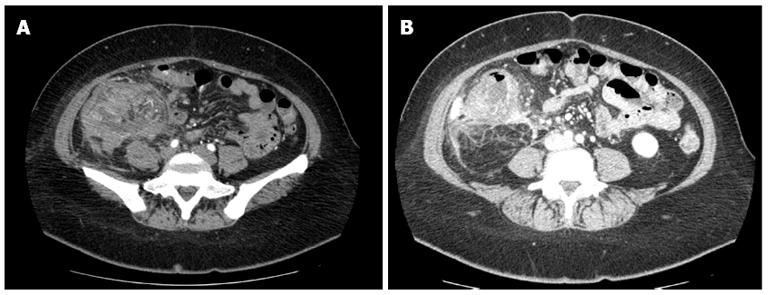
A 56-year-old female presented to our Emergency Department with severe abdominal pain in the right lower quadrant which developed gradually over 3 mo, weight loss and intermittent fever. She denied other symptoms such as vomiting, hematemesis and melena. Her past medical history was positive for diabetes, hyperthyroidism treated with total thyroidectomy in 2008 and replacement therapy with levothyroxine, and class I obesity (body mass index: 30.7 kg/m2). She denied smoking, alcohol use, or any illicit drug use. Two months previously she had 3 consecutive fecal occult blood tests which were all negative. Physical examination showed a sore and tender abdomen, particularly painful in the right lower quadrant where a rigid, suspicious mass was palpable along with a positive Blumberg maneuver. Bowel sounds in all 4 quadrants and rectal examination were normal. Blood tests revealed microcytic, hypochromic anemia [hemoglobin (Hb) 9.5 g/dL; normal value (NV) 12-16], normal leukocyte count, and elevated C-reactive protein (17.5 mg/dL; NV 0-0.5). Aspartate aminotransferase and alanine aminotransferase values were slightly increased (57 U/L; NV 15-46 and 145 U/L; NV 11-66, respectively). Gamma-glutamyltransferase, triglyceride and cholesterol levels were within the normal range. Oncomarkers (carcinoembryonic antigen and carbohydrate antigen) values were within the normal range. An abdominal computed tomography (CT) scan showed a solid irregular mass, measuring 96 mm × 91 mm × 66 mm, with large necrotic areas and several enlarged lymph nodes around it (Figure 1A and B). The lesion also seemed to be adherent to the VI liver segment. Clinical and radiological findings raised the suspicion of right colon cancer involving the surrounding structures with a clinical preoperative staging of: cT4 cN+ cM0. After 24 h, because of worsening of clinical conditions, the patient underwent median laparotomy. Intraoperatively, a large mass, fixed to nearby structures, and involving the ileocecal valve and cecum was found. A frozen section of the specimen was performed and revealed chronic inflammation. A right colectomy was performed. Postoperative recovery was uneventful.
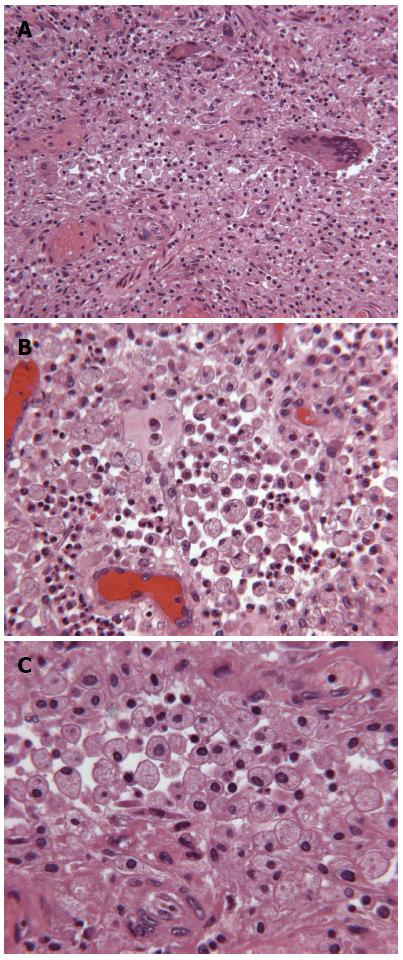
Histological examination revealed the intestinal wall distorted by a diffuse infiltration of lipid-laden macrophages (macrophage cytoplasm containing large amounts of lipid) and giant cells, mainly filling the sub-serosal surface, associated with suppurative peritonitis. The intestinal wall of the ileocecal valve was closely adhered to the appendix, causing luminal stenosis. In the appendix, the mucosa was histologically not involved in the disease, but the outer part of the appendix wall was closely adhered to the ileocecal junction and was equally heavily infiltrated by a large amount of lipid-laden macrophages (Figure 2).
XGI is a rare disease first reported in the genitourinary tract[7,8]. Any organ can be involved, but it is most common in the kidney and in the gallbladder. In particular, XGI of the gallbladder is found in 1%-4% of resected specimens[9]. In some cases, when the inflammatory process involves adjacent organs, it may clinically resemble invasive gallbladder carcinoma leading to extensive surgical resection. As reported by Rastogi et al[9] in 2010, most patients with xanthogranulomatous cholecystitis are female, presenting with vomiting, right upper quadrant pain, and a previous or concomitant diagnosis of gallstones. Xanthogranulomatous pyelonephritis constitutes less than 1% of chronic pyelonephritis, is frequently associated with urinary tract obstruction, nephrolitiasis and concomitant infection, and is preponderant in females and younger age groups[10]. Due to its vague and non-specific clinical presentation, equivocal laboratory and radiological investigations may mimic renal tuberculosis or renal carcinoma[10].
XGI is a disease with specific macroscopic and microscopic features. Typical findings on macroscopic examination include a bright yellow mass with abscessual cavities and micro-abscesses; on microscopic examination, it includes large numbers of lipid-laden macrophages, combined with a minor component of chronic and acute inflammatory cells[4]. Other lesions containing foam cells, such as xanthoma, malacoplakia and pseudoxanthogranulomatous inflammation should be considered in the differential diagnosis. Xanthomatous lesions are not accompanied by fibrosis or giant cells. Malacoplakia is an unusual inflammatory condition characterized by inflammatory xanthomatous proliferation with the presence of Michaelis-Gutmann bodies. Pseudoxanthogranulomatous inflammation is characterized by pigmented foam cell collections with brown lipofuscin or hemosiderin pigment in their cytoplasm that are positive for Fontana-Masson or Prussian blue stains[4]. In the present case, no pigment-containing cells were found and the Fontana-Masson stain was negative, therefore pseudoxanthogranulomatous inflammation was exluded in the differential diagnosis.
The exact pathogenesis of XGI is not well known. There have been many hypotheses, from inflammation and chronic suppuration, to hemorrhages and digestion of blood cells from macrophages, to defective lipid transportation, defective chemotaxis of macrophages and lymphatic obstruction[1-6]. Most recent studies are suggest that XGI probably represents a chronic suppurative process leading to tissue destruction and localized proliferation of macrophages containing large amounts of lipid, which are the characteristic histological features of the disease[2,6].
In particular, for the colon, it is possible that the inflammatory processes following diverticulitis, perforation, or appendicitis may cause a chronic suppurative process, with tissue destruction, that serves as an environment in which the host and microorganisms interact, leading to aggregation of lipid-accumulating macrophages[11]. Specifically, our patient was suffering from hyperthyroidism and diabetes, so had disrupted lipid and carbohydrate metabolism. Those conditions could play a role in development of XGI.
When XGI presents as a mass with an extension of fibrosis and inflammation to the surrounding tissues, it is not possible to differentiate it from an infiltrative cancer[2]. For this reason, symptoms, signs and imaging studies showing an irregular contrast-enhanced lesion extending to surrounding tissues, can easily mislead the surgeon.
To the best of our knowledge, there are only 5 reported cases regarding colonic XGI in the international literature (Table 1), 3 women and 2 men, and the age of the patients ranged from 30 to 72 years, all of them undergoing radical surgical intervention with no described relapse of the disease[2,6]. The first paper was published in 1986 by Davis et al[3], reporting the case of a 30-year-old woman with a double cervix and uterus didelphys presenting with rectal pain and palpable rectal mass. The final diagnosis, after a posterior surgical approach because of the suspicion of a tumor involving the sacrum, was an anorectal xanthogranulomatous abscess in a Müllerian duct remnant. Then, in 1996, Lo et al[4] presented the case of a 72-year-old male with abdominal distension and a palpable mass in the left iliac fossa. With suspicion of an occluding carcinoma of the sigmoid colon or diverticulitis with stricture, the patient underwent resection of the sigmoid, part of the jejunum and the peritoneum. The final pathology showed a XGI of the sigmoid colon. Later, in 2005, Oh et al[5] published the case of a 38-year-old female with diarrhea, fever and left lower quadrant abdominal pain. She underwent low anterior resection with a final diagnosis of XGI of the sigmoid colon. Anadol et al[2] reported in 2009 a case very similar to ours. The patient was a 57-year-old women presenting with right lower quadrant abdominal pain, rectorrhagia, anemia, and a solid mass of the right colon on a CT scan. She also underwent right colectomy with a pathological report showing a xanthogranulomatous colitis of the cecum. One of the differences with our case is that our patient presented to the Emergency Department with local peritonitis in the right lower quadrant and was admitted as having an acute abdomen; because of the suspicion of an abscess with diverticula and/or a neoplasm we did not perform colonoscopy. The worsening of the clinical conditions led to the surgical intervention. Finally, very recently, Dhawan et al[6] reported a 60-year-old male with abdominal pain, vomiting and constipation, who underwent right colectomy. The pathology showed right colic XGI with mucosal involvement; this is in contrast to our case, and all other reports about colic XGI, where intestinal wall involvement was mainly sub-serosal. All these 5 cases show that the symptoms, signs and radiological examination are very similar to those of colorectal cancer. In our experience, we suggest considering XGI also in the event of acute abdomen, or inflammatory abscess. The consensus is that it might be useful to confirm the diagnosis intraoperatively, as a frozen section did not help us in our surgical strategy, as was also reported by Anadol et al[2].
| Ref | Age (yr)/sex | Involved organs | Clinical presentation | CT findings preoperative diagnosis | Surgical operation/ pathology |
| Anadol et al[2] | 57/F | Cecum and appendix | RLQ abdominal pain, rectorrhagia, anemia | CT: Solid mass in the RLQ with poorly defined margins and mesenteric fatty tissue infiltrationCecum cancer | Appendectomy |
| Frozen section | |||||
| Right colectomy | |||||
| XGI of the cecum | |||||
| Davis et al[3] | 30/F | Anorectal area | Rectal and sacral pain, nausea, weight loss, palpable tender mass on rectal examination | CT: two masses involving the intramural portion of the distal rectal wall | Posterior approach, removal of the tumors, reapproximation of the rectal wall |
| Tumor involving the sacrum | XGI of a Müllerian duct remnant involving the anorectum | ||||
| Lo et al[4] | 72/M | Sigmoid colon | Intestinal obstruction, palpable tender mass in the LIF, tenesmus, nausea and weight loss | Barium enema: stricture at the sigmoid colon causing obstruction | Excision of the mass including sigmoid colon, proximal jejunum and part of the peritoneum |
| Sigmoid cancer or diverticulitis with stricture | XGI of the sigmoid colon | ||||
| Oh et al[5] | 38/F | Sigmoid colon, appendix, salpinx | Abdominal pain, diarrhoea, fever, mild RLQ tenderness without any palpable mass | CT: Colonic loop around the rectosigmoid junction with mesenteric fat infiltration | Resection of the sigmoid colon, appendectomy, right salpingectomy |
| Sigmoid cancer | XGI of the sigmoid colon | ||||
| Dhawan et al[6] | 60/M | Ascending colon | Abdominal pain, constipation, vomiting | CT: irregular circumferential thickening involving 6 cm of the ascending colon. Multiple small pericolic lymph nodes | Right colectomy |
| Right colon cancer | XGI of the ascending colon with mucosal involvement | ||||
| Present case | 56/F | Cecum, jejunal loop | Abdominal pain, palpable mass in the RIF, fever and weight loss | CT: expansive mass originating from the cecum with necrotic areas that seems to involve VI liver segment. Many lymph nodes enlarged, especially next to the mass. | Right colectomy |
| Right colon cancer | XGI of the ileocecal valve |
XGI is a rare entity, with kidney and gallbladder as the most common reported sites. The large intestine is an unusual localization of XGI, with only 5 cases being reported in the literature. It is very difficult to differentiate from advanced cancer and/or a local abscessed intestinal mass because inflammation and fibrosis of the lesion extend to the surrounding tissues. We think that the suspicion of malignancy is likely to remain unclear until the final pathological examination is performed. Colonic XGI is a benign disease, often requiring extended surgical resection, and has an excellent postoperative outcome.
P- Reviewer: Lipar M S- Editor: Zhai HH L- Editor: Cant MR E- Editor: Wang CH
| 1. | Cozzutto C, Carbone A. The xanthogranulomatous process. Xanthogranulomatous inflammation. Pathol Res Pract. 1988;183:395-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Anadol AZ, Gonul II, Tezel E. Xanthogranulomatous inflammation of the colon: a rare cause of cecal mass with bleeding. South Med J. 2009;102:196-199. [PubMed] |
| 3. | Davis M, Whitley ME, Haque AK, Fenoglio-Preiser C, Waterman R. Xanthogranulomatous abscess of a mullerian duct remnant. A rare lesion of the rectum and anus. Dis Colon Rectum. 1986;29:755-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Lo CY, Lorentz TG, Poon CS. Xanthogranulomatous inflammation of the sigmoid colon: a case report. Aust N Z J Surg. 1996;66:643-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Oh YH, Seong SS, Jang KS, Chung YW, Paik CH, Park YW, Han DS. Xanthogranulomatous inflammation presenting as a submucosal mass of the sigmoid colon. Pathol Int. 2005;55:440-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Dhawan S, Jain D, Kalhan SK. Xanthogranulomatous inflammation of ascending colon with mucosal involvement: report of a first case. J Crohns Colitis. 2011;5:245-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Peterson RO. Urologic pathology. 3rd ed. Philadelphia: JB Lippincott Co 2006; 23-24. |
| 8. | Selzer DW, Dahlin DC, Deweerd JH. Tumefactive xanthogranulomatous pyelonephritis. Surgery. 1957;42:874-883. [PubMed] |
| 9. | Rastogi A, Singh DK, Sakhuja P, Gondal R. Florid xanthogranulomatous cholecystitis masquerading as invasive gallbladder cancer leading to extensive surgical resection. Indian J Pathol Microbiol. 2010;53:144-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Goyal S, Gupta M, Goyal R. Xanthogranulomatous pyelonephritis: A rare entity. N Am J Med Sci. 2011;3:249-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Antonakopoulos GN, Chapple CR, Newman J, Crocker J, Tudway DC, O’Brien JM, Considine J. Xanthogranulomatous pyelonephritis. A reappraisal and immunohistochemical study. Arch Pathol Lab Med. 1988;112:275-281. [PubMed] |