Published online Jul 7, 2014. doi: 10.3748/wjg.v20.i25.8298
Revised: March 13, 2014
Accepted: April 5, 2014
Published online: July 7, 2014
Processing time: 249 Days and 13.8 Hours
Arteriovenous fistulas between the inferior mesenteric artery and vein are rare, with only 26 primary and secondary cases described in the literature. Secondary fistulas occur following operations of the left hemicolon and manifest as abdominal pain, abdominal mass, gastrointestinal bleeding, colonic ischemia and portal hypertension. Symptom intensities are flow-dependent, and can range from minimal symptoms to severe heart failure due to left to right shunt. Diagnosis is usually established by radiological or intraoperative examination. Treatment options include embolization and/or surgical resection. Therapeutic decisions should be adapted to the unique characteristics of the fistula on an individual basis. A new case of a primary arteriovenous fistula is described and discussed along with a complete review of the literature. The patient in this report presented with signs and symptoms of colonic ischemia without portal hypertension. The optimal treatment for this patient required a combination of embolization and surgical operation. The characteristics of these rare inferior mesenteric arteriovenous fistulas are examined and some considerations concerning diagnostic and therapeutic strategies that should be followed are presented.
Core tip: Inferior mesenteric arteriovenous fistulas are rare, with only 26 known cases described in the literature. This case report describes the diagnostic and therapeutic approach to a new case of a fistula in the inferior mesenteric artery and vein along with a complete literature review. The pathophysiologic, clinical and diagnostic aspects are explored in order to raise awareness of this rare condition.
- Citation: Athanasiou A, Michalinos A, Alexandrou A, Georgopoulos S, Felekouras E. Inferior mesenteric arteriovenous fistula: Case report and world-literature review. World J Gastroenterol 2014; 20(25): 8298-8303
- URL: https://www.wjgnet.com/1007-9327/full/v20/i25/8298.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i25.8298
An arteriovenous fistula (AVF) is a direct communication between an artery and a vein without interposition of the capillary bed. AVFs commonly involve the hepatic, superior mesenteric and splenic arteries[1,2], though rare instances of fistulas between the inferior mesenteric artery and vein (IMA-V) have been described in the literature (Tables 1 and 2). These rare AVFs act as a left to right shunt causing pathophysiologic alteration of bowel function and manifest with a variety of signs and symptoms that are attributed to ischemic, congestive or hemodynamic mechanisms, including abdominal pain, abdominal mass with thrill, upper or lower gastrointestinal (GI) bleeding, portal hypertension, ischemic colitis and cardiac failure[3-5]. The condition is diagnosed upon observing a thickened and congested left hemicolon by computed tomography (CT), or by direct visualization of the AVF and estimation of its precise anatomy using angiography or magnetic resonance angiography (MRA)[1,2,6,7]. Treatment strategies for AVF involve either surgical intervention or embolization, which though safer, carries the danger of ischemia or passage of embolization material into portal circulation[3,7]. In this report, a new case of congenital IMA-V AVF is presented along with a complete review of the literature. Furthermore, the particular characteristics of AVFs are analyzed and methods for proper treatment are discussed.
| Case | Sex | Age | Clinical sign | ||||||
| Abdominal pain | Lower GI bleeding | Abdominal mass/bruit | Upper GI bleeding | Portal hypertension | Ischemic colitis | Management | |||
| Van Way et al[10], 1971 | F | 72 | √ | √ | Left hemicolectomy | ||||
| Sabatier et al[17], 1978 | M | 22 | √ | √ | √ | None (patient’s refusal) | |||
| Oyama et al[18], 1980 | M | 70 | √ | Left hemicolectomy | |||||
| Manns et al[11], 1990 | M | 33 | √ | √ | Left hemicolectomy; mesenteric vein anastomosed to vena cava | ||||
| Baranda et al[16], 1996 | M | 63 | √ | √ | Ligation and resection of fistula | ||||
| Capuano et al[9], 2004 | F | 76 | √ | √ | √ | Embolization; ligation of AVF | |||
| Nemcec and Yakes[19], 2005 | M | 65 | √ | √ | Vein embolization | ||||
| Matsui et al[20], 2007 | M | N/A | Embolization | ||||||
| Kim et al[3], 2008 | M | 56 | √ | √ | √ | √ | Percutaneous angioplasty of portal vein; left hemicolectomy | ||
| Metcalf et al[7], 2008 | M | 50 | √ | √ | Left hemicolectomy | ||||
| Türkvatan et al[2], 2009 | M | 83 | √ | √ | √ | Left hemicolectomy | |||
| Akgun et al[6], 2013 | M | 48 | √ | √ | Total colectomy | ||||
| El Muhtasaeb et al[21], 2013 | M | 57 | √ | √ | √ | Embolization; left hemicolectomy | |||
| Plotkin et al[14], 2013 | F | 70 | √ | √ | √ | Embolization | |||
| Takahashi et al[15], 2013 | M | 78 | √ | √ | Resection | ||||
| Current case | M | 63 | √ | √ | Embolization; left hemicolectomy | ||||
| Case | Sex | Age | Previous operation | Clinical sign | Management | |||||
| Abdominal pain | Lower GI bleeding | Abdominal mass/bruit | Upper GI bleeding | Portal hypertension | Ischemic colitis | |||||
| Houdard et al[22], 1970 | F | 51 | Excision of splenic flexure | √ | √ | √ | Left hemicolectomy | |||
| Hirner et al[23], 1978 | F | 43 | Obstetrical | √ | √ | Left hemicolectomy | ||||
| Capron et al[13], 1984 | F | 60 | Volvulus of the sigmoid | √ | √ | √ | √ | Intraarterial embolization | ||
| Slutski et al[12], 1988 | M | 63 | Anterior resection of rectum | √ | Embolization | |||||
| Peer et al[24], 1989 | M | 63 | Anterior resection of the rectum | √ | √ | √ | Embolization | |||
| Pietri et al[25], 1990 | M | 62 | Left colectomy | √ | √ | Left hemicolectomy | ||||
| F | 60 | Left colectomy | √ | √ | √ | Intraarterial embolization | ||||
| Vauthey et al[1], 1997 | M | 58 | Blunt trauma | √ | √ | AVF occlusion; embolization; percutaneous alcohol injection | ||||
| Okada et al[8], 2002 | F | 69 | Sigmoidectomy | √ | √ | Left sigmoidectomy | ||||
| Fabre et al[5], 2005 | M | N/A | Esophagogastrectomy; sigmoidectomy | Embolization | ||||||
| Gorospe et al[26], 2012 | M | 58 | Right hemicolectomy | √ | √ | Embolization; total colectomy | ||||
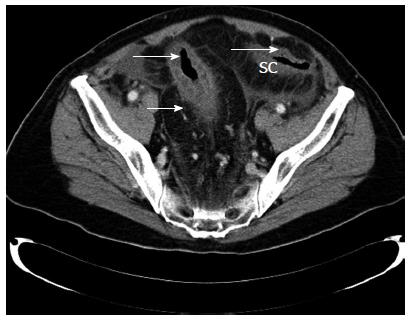
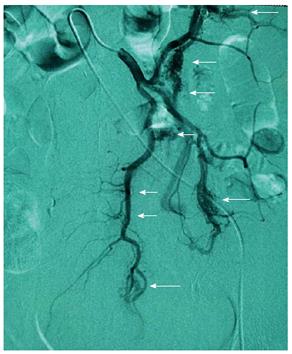
A 66-year-old patient was referred to our department for definitive treatment of a primary IMA-V AVF. A month prior to admission, the patient was treated at a private hospital for a right groin hernia. Although he had been discharged in good condition, he was readmitted after ten days with symptoms of intestinal obstruction. An abdominal CT scan revealed a dilated colon and extensive transmural edema of the colonic wall extending from the splenic flexure to the end of the rectum along with pericolic fat edema. Dilation of the vascular branches of the IMA-V plexus within the bowel wall of the anal canal, rectum and inferior sigmoid was noted, raising suspicion of an arteriovenous communication (fistula) between the branches of the inferior mesenteric artery (IMA) and vein (IMV) (Figure 1). An elective angiography of the IMA confirmed this suspicion and further defined at least four definite points of high flow between all IMA and IMV branches and with the hemorrhoidal plexus (Figure 2). The patient’s worsening condition prompted laparoscopic (robotically assisted) exploration. The procedure was converted to an open operation with a midline incision due to the marked mesenteric enlargement of the left colon. Dilated veins and arteries were found at the left colon mesentery and the decision was made to proceed with a colostomy. Following a right-end colostomy and left colonic mucus fistula, the patient gradually recovered. Pathologic examination of the left part of the dilated transverse colon removed for biopsy revealed multiple foci of vascular malformations in the submucosal layer and within the colic fat with accessory areas of collateral vascular flow formation. Vascular branches showed signs of thrombophlebitis and vascular congestion. The passive congestion and stasis were attributed to the arteriovenous communication. At this point, the patient was transferred to our department for further treatment.
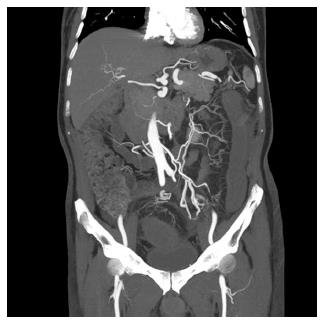
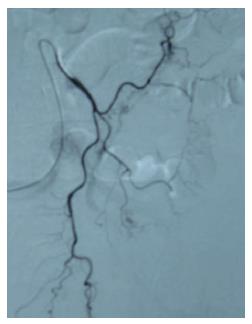
The physical examination of the abdomen upon admission was unremarkable. No mass was detected in the left lower quadrant and no bruit or thrills were noted. The patient presented no signs or symptoms of portal hypertension. Full laboratory tests were also unremarkable. A colonoscopy showed signs of ischemic colitis of the left colon 25 cm from the anal verge and normal rectal mucosa. An MRA of the abdominal aortic branches confirmed the persistence of AVFs (Figure 3). This diagnosis of primary IMA-V AVF indicated angiography and subsequent embolism of the AVF sites (Figure 4). In the event that this intervention was not curative, it was believed that it would facilitate a successful left hemicolectomy.
Two weeks after the fistula embolization, a CT scan revealed reduced swelling of the remaining colon and contraction of the aberrant vascular branches. The patient’s abdominal discomfort and bloody diarrhea gradually disappeared over a three-month period, and repeated colonoscopies showed gradual improvement of the mucosal swelling. Necrotic foci healed, however the left colon was constricted. Multiple biopsies of the left and right colon did not show any signs of malignancy. A barium enema did not reveal a mass, but rather a narrowing of the left colon.
Six months after the initial operation, the patient underwent an additional procedure to reconnect the colostomy. A left hemicolectomy was performed, as the remaining descending colon, sigmoid and upper rectum were not functional due to atrophy and ischemia (Figure 5). The right colon was directly anastomosed to the upper rectum and a prophylactic ileostomy was performed. The patient’s postoperative course was complicated on the tenth day by a pulmonary embolism that was treated with low molecular weight heparin for a week followed with oral anticoagulants. The patient was discharged in very good health on the fourteenth postoperative day. The ileostomy was restored uneventfully after two months, and repeated colonoscopies and CTs were normal after six months.
IMA-V AVFs can be of congenital or iatrogenic etiology, though there is one reported case of traumatic origin involving branches of the superior mesenteric artery[1]. Congenital AVFs occur from undifferentiated embryonic vessels that fail to regress and interconnect the arterial and venous system. In a relatively low percentage of cases, these AVFs remain wide open as discrete arteriovenous communications[4,8]. Congenital etiologies often result in the formation of multiple AVFs[2], which are components of Osler-Weber-Rendu and Ehlers-Danlos syndromes[1,9]. The rupture of a congenital arterial aneurysm in very close proximity to a vein can also result in the formation of an AVF[10]. Iatrogenic AVFs between the IMA and IMV typically occur as fistulas formed following a left hemicolectomy or sigmoidectomy, caused by transfixion sutures that simultaneously pass through arteries and veins, or by the ligation of an artery and vein[8]. Arterioportal AVFs, which are connections between the arterial and portal systems, have also been described after a variety of interventional procedures including percutaneous biopsy, cholangiography and splenoportography[1]. Surgical arterialization of the portal vein is known to cause sclerosis at portal vein radicles and intrahepatic fibrosis[11].
Clinical signs and symptoms of IMA-V AVFs (Table 3) result from pathophysiologic changes. Abdominal pain is caused by the simultaneous shunting of left hemicolon arterial perfusion and congestion of venous circulation. The congested viscera can form a palpable abdominal mass, as do fistulas that have assumed a tumor-like form. The turbulent circulation inside the AVF presents as bruit upon auscultation. Colonic ischemia is a result of the shunting of arterial flow from the inferior mesenteric vein and portal system and venous stasis caused by the AVF. Lower GI bleeding can result from vascular engorgement of the bowel mucosa, fistula rupture in the bowel lumen[12], the ischemic colitis itself or by hemorrhoids. Upper GI bleeding, which is less common in congenital cases, can result from portal hypertension caused by esophageal varices. Interestingly, upper GI bleeding shows a gender bias, occurring in 25% of female cases and 0% of males with IMA-V AVFs. Portal hypertension also shows a gender difference, observed in 87.5% of female cases vs 36.8% of males, and is caused by an inferior mesenteric AVF. This “forward” or “hyperkinetic” hypertension may precipitate from both an increase in blood flow into the portal system that can not directly accept it and a compensatory increase in hepatic vascular resistance[3,8], resulting in a normal hepatic venous pressure gradient[13]. Portal hypertension can induce ascites, varices, hepatic encephalopathy and splenomegaly, and is more prominent in older patients, as the minimal intrahepatic resistance in younger patients allows systemic circulatory symptoms to dominate[2,5,14]. Of particular interest are the cases presented by Plotkin et al[14] and Takahashi et al[15] where portal hypertension gave rise to hepatic regenerative nodules, resembling hepatocellular carcinoma, even at biopsy, which involuted after AVF correction. Baranda et al[16] described a case of AVF between the left colic artery and IMV, manifesting with duodenal varices. Lastly, high flow through an AVF can lead to cardiac failure[4], such as in a case reported by Fabre et al[5] where embolization of the IMA-V AVF in a patient with cardiac failure resulted in improved cardiac function and an increased ejection fraction.
| Total | Congenital | Acquired | |
| Males | 70.4% | 81.3% | 54.5% |
| Age, yr | 60.2 | 61.3 | 58.7 |
| Abdominal pain | 55.6% | 62.5% | 45.5% |
| Lower GI bleeding | 55.6% | 56.3% | 54.5% |
| Abdominal mass/thrill | 22.4% | 12.5% | 36.4% |
| Upper GI bleeding | 7.4% | 0% | 18.2% |
| Ischemic colitis | 33.3% | 43.8% | 18.2% |
| Portal hypertension | 51.9% | 50.0% | 54.5% |
The infrequency of IMA-V AVFs makes it difficult to establish specific criteria for diagnosis, which is not clinically feasible, and occurs during in-depth investigation of patient signs and symptoms. For example, IMA-V AVFs may be diagnosed by the observation of ischemic colitis during colonoscopy, identification of turbulent flow by ultrasound, or CT visualization of colonic thickening and congestion, the AVF itself or its venous branches. To prevent misdiagnosis and suboptimal intervention, we believe that it is necessary to combine: (1) a clinical sign of an ischemic colon; (2) proof of the fistula’s presence, preferably by angiography; and (3) an intraoperative sign of a congested colon. Furthermore, a medical history that includes an operation at the left hemicolon strongly enhances, but is not necessary, for diagnosis.
Proper treatment for IMA-V AVFs is debatable and case-specific, though typically involves embolization or surgical resection. Embolization is less invasive and potentially safer but carries the risk of organ ischemia or a probable recurrence, especially if there are more than one feeding vessels. Furthermore, the migration of embolization material can occur when the AVF diameter is greater than 8 mm and has a high flow rate[2,5]. As demonstrated by the case presented here, even partial success with embolization reduces the risk for hemorrhage or possible future surgical intervention. Complete surgical resection of the entire affected bowel, though more likely to be curative, carries a significant risk for hemorrhage. Partial resection is not likely to be curative or palliative, as evidenced in our patient by the lack of reduced flow in the fistula and re-channeling to other branches after the first procedure.
Our patient suffered from a congenital IMA-V AVF causing colonic ischemia with abdominal pain but without portal hypertension. As the initial partial resection was inadequate, a safer option was embolization in order to eliminate the AVF and the risk of hemorrhage if surgery was considered necessary, as was finally the case. The complexity of AVFs demands the cooperation of those with diverse specialties and expertise, as well as case-specific solutions. Considering the large number of left hemicolon operations that are performed, it is remarkable that these fistulas are so rare. However, the surgical community should be cognizant of their occurrence, as a high rate of suspicion is beneficial for the patient and would likely increase the number of diagnoses. When diagnosed, intervention should be carefully planned to avoid performing unsuccessful procedures that can impede subsequent therapies and add to morbidity and mortality.
A 66-year-old man presented with symptoms of intestinal obstruction attributed to a fistula between the inferior mesenteric artery and vein.
Abdominal pain and ileus.
Colonic ischemia, ileus from adhesion, intestinal obstruction from a tumor.
Unremarkable.
Elective angiography of the inferior mesenteric artery confirmed at least four definite points of high flow between all inferior mesenteric artery and vein branches and with the hemorrhoidal plexus.
Multiple foci of vascular malformations in the submucosal layer of the colon specimen and within the colic fat with accessory areas of collateral vascular flow formation.
Elective embolization of the inferior mesenteric artery and a left hemicolectomy due to atrophy after embolization.
Existence of inferior mesenteric artery-vein fistulas can be suspected but definite proof is only by angiography.
An arteriovenous fistula is a direct communication between an arterial and venous branch that bypasses the capillary bed. An arterioportal fistula is a connection between the splanchnic arteries and the portal vein that can result in portal hypertension.
This case explains a diagnostic approach to a rare situation but also analyzes the importance of very careful preoperative interventional planning to avoid a suboptimal procedure.
This article analyzes and reviews a rare occurrence of an inferior mesenteric arteriovenous fistula with a complete review of the world literature. A diagnostic algorithm is proposed when a fistula is suspected early to prevent misdiagnosis and improper treatment of the patient.
P- Reviewers: Di Fabio F, Lee KY, Tsimogiannis KE, Xiao LB S- Editor: Wen LL L- Editor: A E- Editor: Liu XM
| 1. | Vauthey JN, Tomczak RJ, Helmberger T, Gertsch P, Forsmark C, Caridi J, Reed A, Langham MR, Lauwers GY, Goffette P. The arterioportal fistula syndrome: clinicopathologic features, diagnosis, and therapy. Gastroenterology. 1997;113:1390-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 134] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Türkvatan A, Ozdemir Akdur P, Akdoğan M, Cumhur T, Olçer T, Parlak E. Inferior mesenteric arteriovenous fistula with ischemic colitis: multidetector computed tomographic angiography for diagnosis. Turk J Gastroenterol. 2009;20:67-70. [PubMed] |
| 3. | Kim IH, Kim DG, Kwak HS, Yu HC, Cho BH, Park HS. Ischemic colitis secondary to inferior mesenteric arteriovenous fistula and portal vein stenosis in a liver transplant recipient. World J Gastroenterol. 2008;14:4249-4252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Blaisdell FW, Stein M. Natural history of congenital arteriovenous fistula. Cardiovasc Surg. 1998;6:566-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Fabre A, Abita T, Lachachi F, Rudelli P, Carlier M, Bocquel JB, Remond A, Pech de Laclause B, Maisonnette F, Durand-Fontanier S. [Inferior mesenteric arteriovenous fistulas. Report of a case]. Ann Chir. 2005;130:417-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Akgun V, Sari S, Verim S, Bozlar U. Arteriovenous malformation of the inferior mesenteric artery in a patient with ischaemic colitis. BMJ Case Rep. 2013;2013:pii: bcr2013009565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Metcalf DR, Nivatvongs S, Andrews JC. Ischemic colitis: an unusual case of inferior mesenteric arteriovenous fistula causing venous hypertension. Report of a case. Dis Colon Rectum. 2008;51:1422-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Okada K, Furusyo N, Sawayama Y, Ishikawa N, Nabeshima S, Tsuchihashi T, Kashiwagi S, Hayashi J. Inferior mesenteric arteriovenous fistula eight years after sigmoidectomy. Intern Med. 2002;41:543-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Capuano G, Pomponi D, Iaccarino V, Budillon G. An unusual case of ascites. Dig Liver Dis. 2004;36:628-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Van Way CW, Crane JM, Riddell DH, Foster JH. Arteriovenous fistula in the portal circulation. Surgery. 1971;70:876-890. [PubMed] |
| 11. | Manns RA, Vickers CR, Chesner IM, McMaster P, Elias E. Portal hypertension secondary to sigmoid colon arteriovenous malformation. Clin Radiol. 1990;42:203-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Slutski S, Peer A, Abramsohn R, Weitz E, Bogokowsky H. Early postoperative inferior mesenteric arteriovenous fistula-A case report. Vasc Endovascular Surg. 1988;22:432-435. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Capron JP, Gineston JL, Remond A, Lallement PY, Delamarre J, Revert R, Veyssier P. Inferior mesenteric arteriovenous fistula associated with portal hypertension and acute ischemic colitis. Successful occlusion by intraarterial embolization with steel coils. Gastroenterology. 1984;86:351-355. [PubMed] |
| 14. | Plotkin E, Assis D, Boyer J. Now you see it, now you don’t. Hepatology. 2013;58:446-447. [DOI] [Full Text] |
| 15. | Takahashi K, Kashida H, Kudo M. Hepatic nodules associated with an inferior mesentric arteriovenous malformation. Intern Med. 2012;51:2753-2755. [PubMed] |
| 16. | Baranda J, Pontes JM, Portela F, Silveira L, Amaro P, Ministro P, Rosa A, Pimenta I, Andrade P, Bernardes A. Mesenteric arteriovenous fistula causing portal hypertension and bleeding duodenal varices. Eur J Gastroenterol Hepatol. 1996;8:1223-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Sabatier JC, Bruneton JN, Drouillard J, Elie G, Tavernier J. [Inferior mesenteric arteriovenous fistula of congenital origin. A report on one case and review of the published literature (author’s transl)]. J Radiol Electrol Med Nucl. 1978;59:727-729. [PubMed] |
| 18. | Oyama K, Hayashi S, Kogure T, Kirakawa K, Akaike A. Inferior mesenteric arteriovenous fistula. -Report of a case and review of the literature. Nihon Igaku Hoshasen Gakkai Zasshi. 1980;40:944-950. [PubMed] |
| 19. | Nemcek AA, Yakes W. SIR 2005 Annual Meeting Film Panel case: inferior mesenteric artery-to-inferior mesenteric vein fistulous connection. J Vasc Interv Radiol. 2005;16:1179-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Matsui A, Iwai K, Kawasaki R, Wada T, Mito Y, Doi T. [Transcatheter embolization of an inferior mesenteric arteriovenous fistula with frequent mucous diarrhea]. Nihon Shokakibyo Gakkai Zasshi. 2007;104:194-199. [PubMed] |
| 21. | El Muhtaseb MS, Gorgun E, Liu M. Arteriovenous malformation: a potential cause of ischaemic colitis. ANZ J Surg. 2013;83:93-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Houdard C, Helenon C, Carles J, Botella R, Favre M, Boulay M, Boschet P. Fistule artérioveineuse mésentérique inferieure et rectocolite ulcéreuse. Arch Fr Mal App Dig. 1970;59:463-474. |
| 23. | Hirner A, Häring R, Bost H, Sörensen R. [Hyperkinetic portal hypertension. Arterioportal fistula: problems--case reports--review of the literature]. Chirurg. 1978;49:303-310. [PubMed] |
| 24. | Peer A, Slutzki S, Witz E, Abrahmsohn R, Bogokowsky H, Leonov Y. Transcatheter occlusion of inferior mesenteric arteriovenous fistula: a case report. Cardiovasc Intervent Radiol. 1989;12:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Pietri J, Remond A, Reix T, Abet D, Sevestre H, Sevestre MA. Arterioportal fistulas: twelve cases. Ann Vasc Surg. 1990;4:533-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Gorospe E, Leggett C, Sun G. Inferior mesenteric arteriovenous malformation: an unusual cause of ischemic colitis. Ann Gastroenterol. 2012;25:165. |