Published online Jul 7, 2014. doi: 10.3748/wjg.v20.i25.8166
Revised: January 4, 2014
Accepted: February 17, 2014
Published online: July 7, 2014
Processing time: 259 Days and 15.8 Hours
AIM: To investigate recurrence rates, patterns and complications after nonoperatively managed complicated diverticulitis (CD).
METHODS: A retrospective study of patients treated for CD was performed. CD was defined on computed tomography by the presence of a localized abscess, pelvic abscess or extraluminal air. For follow-up, patients were contacted by telephone. Numbers of elective surgeries, recurrences and abdominal pain were analyzed.
RESULTS: A total of 114 patients (median age 57 years (range 29-97)), were admitted for CD. Nine patients required surgical intervention for failure of conservative therapy (Hartmann’s procedure: n = 6; resection and colorectal anastomosis: n = 3). Of the 105 remaining patients, 24 (22.9%) underwent elective sigmoid resection. The 81 (71%) non-operated patients were all contacted after a median follow-up of 32 mo (4-63). Among them, six had developed a recurrent episode of diverticulitis at a median follow-up of 12 mo (6-36); however, no patient required hospitalization. Sixty-eight patients (84%) were asymptomatic and 13 (16%) had recurrent abdominal pain.
CONCLUSION: Conservative policy is feasible and safe in 71% of cases, with a low medium-term recurrence risk.
Core tip: We sought to determine whether a conservative approach to the sigmoid colon could be proposed after complicated diverticulitis. One hundred and fourteen patients were included in this study, which confirmed that the conservative approach is feasible in 71% of cases after an episode of complicated diverticulitis (CD). Indications for elective sigmoid resection should not be based solely on CD episode. This approach not only has an impact for the patient, but also for the health care system.
- Citation: Bridoux V, Antor M, Schwarz L, Cahais J, Khalil H, Michot F, Tuech JJ. Elective operation after acute complicated diverticulitis: Is it still mandatory? World J Gastroenterol 2014; 20(25): 8166-8172
- URL: https://www.wjgnet.com/1007-9327/full/v20/i25/8166.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i25.8166
Diverticular disease is a common gastrointestinal disorder, found in a third of people over the age of 60 years in the Western world[1]. It is thought to be caused by the low fiber diet in developed countries and affects the sigmoid colon in 90% of cases[2].
Lifetime prevalence of diverticulitis is 10%-25% among patients with diverticular disease, and is increasing[1,3].
Acute diverticulitis is usually graded as ‘uncomplicated’ or ‘complicated’ according to the classification of the European Association for Endoscopic Surgery[4], as ‘mild’ or ‘severe’ according to the Ambrosetti computed tomography (CT) criteria[5], or the modified Hinchey classification[6]. Hinchey classification type I and type II refer to paracolic abscesses, while type III and IV refer to purulent and fecal peritonitis, respectively.
In 2006, the American Society of Colon and Rectum Surgeons revised its practice parameters for sigmoid diverticulitis, and stated that “elective colon resection should typically be advised if an episode of complicated diverticulitis is treated nonoperatively”[7].
Conversely, some authors reported management using a conservative policy. Myers et al[8] reported 92 patients with Hinchey III peritonitis managed by laparoscopic peritoneal lavage only. Of these patients, only two re-presented with diverticulitis at a median follow-up of 36 mo (range 12-84). Recently, Gaertner et al[9] reported 32 patients that received percutaneous drainage of diverticular abscess without subsequent colectomy, with a recurrence-free survival of 58% at 7.4 years.
Since January 2008, we have not systematically performed subsequent colon resection after successful conservative management of complicated diverticulitis (CD). This study, conducted at Rouen University Hospital, investigated recurrence rates, patterns and complications in patients with nonoperatively managed complicated diverticulitis.
We performed a retrospective study of patients admitted between January 2008 and December 2012 for CD managed by conservative approach.
CD was defined on CT by the presence of a mesocolic abscess, pelvic abscess or extraluminal air. This classification was based on the definition used by Ambrosetti et al[5]. Pelvic abscesses were those located below the pelvic brim, and mesocolic abscesses were those located above the pelvic brim.
Patients were managed with intravenous fluids and antibiotics (cefotaxime (1 g three times daily) and metronidazole (500 mg three times daily). Intravenous antibiotics were administered for a minimum of 72 h, and then oral antibiotics were continued for 2 wk (ofloxacine (200 mg twice daily) and metronidazole (500 mg three times daily).
CT-guided percutaneous drainage was performed if clinical and biological parameters had not improved with antibiotics and if the radiologist considered the procedure safe.
Initial response to therapy was assessed in an inpatient setting and included the following criteria: improvement in abdominal pain and tenderness, normal vital signs (blood pressure, heart rate, respiratory rate and fever), normalization of leukocytosis and C-reactive protein, and return of antegrade GI function while tolerating an oral diet.
Failure of nonoperative therapy included persistent or increased abdominal pain and/or tenderness associated with persistent systemic inflammatory response syndrome criteria (temperature < 36 °C or > 38 °C, heart rate > 90 beats per minute, respiratory rate > 20 breaths per minute or PaCO < 32 mmHg; and leukocytes > 12000 cells/mm³, < 4000 cells/mm³, or > 10% immature (band) forms)[10].
Patients with failed nonoperative management underwent repeat abdominal CT followed by surgery.
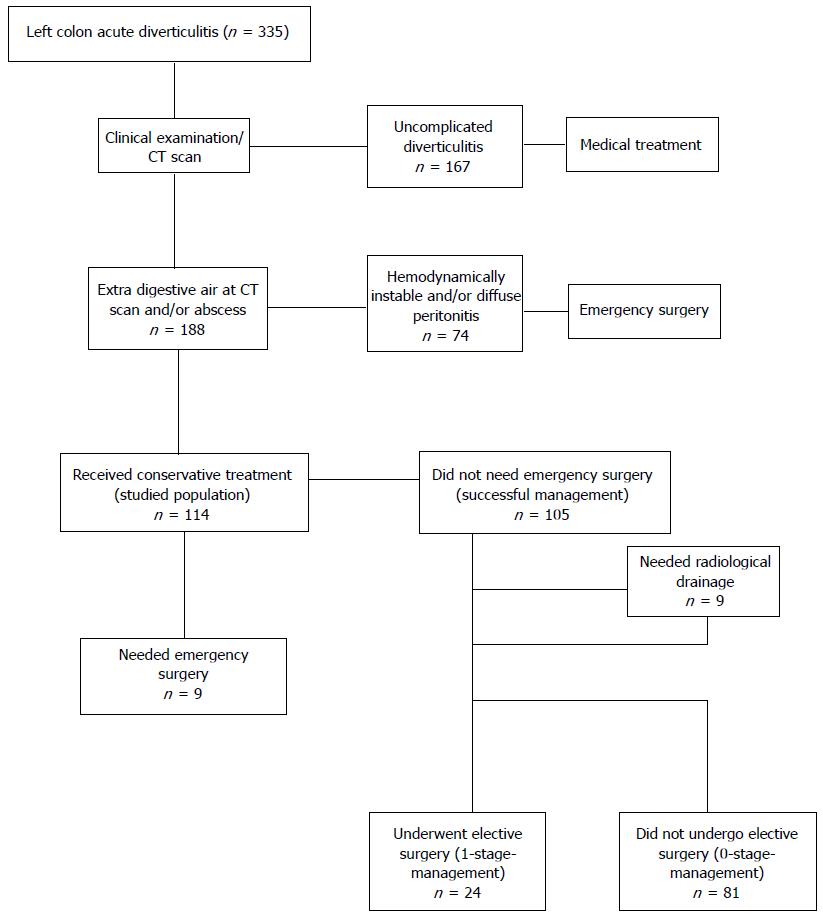
Treatment failure was defined as the need for emergency surgery or mortality. Radiologically guided drainage of intra-abdominal abscess(es) and recurrent symptoms were not considered as treatment failure. Recurrence was defined as recurrence of symptoms more than 30 d after discharge. The patient selection procedure is summarized in Figure 1. Patients were followed up 6 wk later with a colonoscopy. Indication for subsequent colectomy was left to the discretion of the surgeon in charge. In May 2013, patients (or the family physician) managed nonoperatively were contacted by telephone. The numbers of elective surgeries, recurrences and abdominal pain were analyzed.
Continuous data were presented either as median (min.-max.) or mean (± SD). Considering the small number of patients per group, multivariate analysis and logistic regression to assess any relative risk could not be performed. A P value ≤ 0.05 was considered significant. Statistical analyses were performed using SPSS 13.0 (SPSS, Inc., Chicago, IL, United States).
During the study period, 335 patients were admitted to our department with acute diverticulitis (Figure 1).
Seventy-four patients were excluded who underwent immediate surgery because of hemodynamic instability and/or generalized peritonitis. The remaining 114 patients were hemodynamically stable and had CT evidence of extra digestive air and/or abscess without any extra digestive stools/liquid; they constituted the studied population [median age: 57 years (range 29-97); 49 female (43%)].
This was the first episode of diverticulitis for 103 patients (90.3%), and 11 patients (9.7%) had undergone at least one previous episode of uncomplicated diverticulitis. Patient comorbidities are summarized in Table 1.
| Comorbidity | |
| Cardiovascular | 13 (11.4) |
| Pulmonary | 6 (5.3) |
| Diabetes | 5 (4.5) |
| Collagen–vascular | 4 (3.5) |
| Obesity | 9 (7.9) |
| Steroids | 3 (2.6) |
Sixty-six patients had evidence of extraluminal air, with a pericolic pneumoperitoneum and a distant pneumoperitoneum in 56 (84.9%) and 10 (15.1%) cases respectively. In 51 cases, the pneumoperitoneum was the only extracolic anomaly on the CT, in two cases the pneumoperitoneum was associated with a pelvic abscess, and in 13 cases with a mesocolic abscess (Table 2).
| Characteristics | Extraluminal air | No extraluminal air | P value |
| 66 (57.9) | 48 (42.1) | ||
| No. of women | 24 (36.4) | 25 (52) | 0.009 |
| Mean age (yr) | 55.43 (± 15.6) | 61.6 (± 17) | 0.03 |
| No. of patients < 50 years old | 26 (39.4) | 14 (29.1) | 0.25 |
| Previous episodes of diverticulitis | 8 (12.1) | 3 (6.3) | 0.35 |
| Leukocytes | 13307 (± 3967) | 14242 (± 4396) | 0.20 |
| CRP | 128.6 (± 87) | 150 (± 86.6) | 0.21 |
| Mesocolic abscess | 13 (19.7) | 39 (81.2) | < 0.0001 |
| Pelvic abscess | 2 (3) | 9 (18.8) | < 0.0001 |
| No abscess | 51 (77.3) | 0 | - |
| Drainage | 1 (1.5) | 8 (16.7) | 0.004 |
| Surgery during first hospital stay | 6 (9) | 3 (6.3) | 0.73 |
| Surgery later | 13 (19.7) | 11 (22.9) | 0.67 |
| Conservative treatment | 47 (71.3) | 34 (70.8) | 0.96 |
| Recurrence | 4 (6) | 5 (10.4) | 0.48 |
Sixty-three patients had evidence of a mesocolic abscess (in 52 cases) or a pelvic abscess (in 11 cases) (Table 3). In 48 cases, the abscess was the only extracolic anomaly on the CT. Nine patients had percutaneous drainage of a large abscess (Table 4), one of whom required subsequent operation.
| Characteristics | Mesocolic abscess | Pelvic abscess | P value |
| 52 (45.6) | 11 (9.6) | ||
| No. of women | 24 (46.1) | 7 (63.6) | 0.337 |
| Mean age (yr) | 60.2 ± 17 | 56.8 ± 11 | 0.41 |
| No. of patients < 50 years old | 16 (30.8) | 2 (18.2) | 0.48 |
| Previous episodes of diverticulitis | 3 (5.8) | 2 (18.2) | 0.28 |
| Co-morbidity | 10 (19.2) | 3 (27.3) | 0.68 |
| Leukocytes | 14263 ± 4290 | 13981 ± 5996 | 0.88 |
| CRP | 141.5 ± 85 | 174 ± 96 | 0.30 |
| Mean size (mm) | 33 ± 16 | 45.5 ± 23 | 0.1 |
| Free air | 13 (25) | 2 (18.2) | 1.0 |
| Drainage | 4 (7.7) | 5 (45.5) | 0.0057 |
| Surgery during first hospital stay | 6 (11.5) | 1 (9) | 1.0 |
| Surgery later | 12 (23) | 2 (18.2) | 1.0 |
| Conservative treatment | 34 (65.4) | 8 (72.7) | 0.73 |
| Recurrence | 5 (9.6) | 0 | 0.57 |
| Condition | n (%) | Mean size (cm) | Size < 5 cm | |
| Mesocolic abscess | Drainage | 4 (7.7) | 6.8 ± 1.9 | 2 |
| No drainage | 48 (92.3) | 3.1 ± 1.4 | 5 | |
| Pelvic abscess | Drainage | 5 (45.5) | 5.5 ± 2.2 | 2 |
| No drainage | 6 (54.5) | 3.8 ± 2.2 | 4 |
Nine patients (7.9%) required intervention for failure of conservative therapy during index admission (Hartmann’s procedure: n = 6, resection and colorectal anastomosis: n = 3) (Table 5). Indications for emergency colectomy included generalized peritonitis (n = 7) on the control CT and persistent pain and fevers (n = 2). Median time to emergency colectomy was 5 d (range, 2-14).
| DC | Surgery during first hospital stay | Surgery later | |
| 2008 | 22 | 2 (9) | 11 (50) |
| 2009 | 22 | 2 (9) | 5 (22.8) |
| 2010 | 19 | 1 (5.3) | 2 (10.6) |
| 2011 | 30 | 2 (6.7) | 5 (16.7) |
| 2012 | 21 | 2 (9.5) | 1 (4.8) |
One patient died 10 d after Hartmann’s procedure of hemorrhagic shock; this patient was 86 years old. Overall median length of hospital stay was 5 d (range, 2-21).
Of the 105 patients who were discharged without resection, 20 subsequently underwent elective sigmoid resection in our department and four in another hospital (Table 6). Median interval until elective sigmoid resection was 5 mo (range, 2-9) and no patient underwent emergency surgery. Indications for surgery were: persisting symptoms for four patients, recurrent and disabling bouts of diverticulitis for three patients, fistula for three patients (coloenteric, colovesical and colovaginal), sigmoid stenosis for one patient, portal venous pneumatosis for one patient, immunodeficiency for one patient, and surgeon decision for 11 patients (colonic resection to prevent further attacks, or complicated disease).
According to our policy, all patients underwent medical examination and colonoscopy systematically 6 wk after discharge and none of them showed colic adenocarcinoma.
In total, 81 patients (71%) were managed only with medical treatment. These 81 non-operated patients (or the family physician) were all contacted after a median follow-up of 32 mo (range, 4-63). Four patients died during follow-up, but cause of death was not related to diverticular disease. Six patients (7%) developed a recurrent episode of diverticulitis with a median follow-up of 12 mo (range, 6-36); however, none of these patients required hospitalization. At the end of follow-up, 68 patients (84%) were completely asymptomatic and 13 (16%) had recurrent abdominal pain.
In univariate analysis, the only factor associated with elective sigmoid resection following successful nonoperative management was the period of the episode [2008-2009 (n = 16) vs 2010-2012 (n = 8), P = 0.006]. Age less than 50 years, free air or abscess on CT were not associated with need for elective surgery.
In our study, nonoperative treatment with intravenous antibiotics, associated with CT-guided percutaneous drainage in selected patients, has enabled us to avoid surgery in 71% of cases.
Although clinical presentation of sigmoid diverticulitis as abscess has increased in recent years[11], questions remain concerning the therapeutic strategies in an acute setting and after successful conservative treatment[8,12-14].
It is generally acknowledged that elective resection should be performed after complicated acute diverticulitis to avoid the high risk of recurrence and further complications[15-17]. However, recent studies have highlighted the fact that an episode of severe diverticulitis may result in a buttressing effect around the affected portion of the colon, thereby protecting it from subsequent attacks[18].
To investigate recurrence rates and post-operative complications following conservatively managed diverticulitis, Eglinton et al[19] retrospectively analyzed clinical data from all patients with diverticulitis admitted to their department from 1997 to 2002. Complicated diverticulitis recurred in 24% of patients, compared to a recurrence rate of 23.4% in those with uncomplicated diverticulitis. Recurrence typically occurred within 12 mo of the initial episode. Furthermore, Collins noted that perforation might be the first manifestation of complicated diverticulitis in around 75% of patients[20].
In our study, only 10% of patients had previously been admitted for diverticular disease. Furthermore, of the 85 patients who did not undergo elective surgery, but who continued successful nonoperative treatment, only six had recurrence. This rate is consistent with the 7%-25% reported previously after conservative management of uncomplicated diverticulitis[21].
The decision to operate must also take into account operative morbidity and mortality associated with elective colectomy and its effectiveness in preventing recurrence. Prophylactic colectomy is not without risk. Surgery for elective diverticular resection has been associated with a mortality risk of up to 4% and with morbidity rates of 25%-55%, including a 10%-14% incidence of stoma formation[22-25].
Moreover, elective resection is not curative in all patients, with recurrence rates following surgery estimated at 2.6%-10.4%[26-30]: a large number of patients report impairment in bowel function[28,31,32].
Few previous studies have examined the management and outcomes of complicated diverticulitis treated nonoperatively.
Ambrosetti et al[33] conducted a study of 73 cases of diverticular abscesses with 43-mo of follow-up. They found that 58% of patients with a mesocolic abscess who had received successful nonoperative treatment during their first hospitalization did not require operative treatment, vs 47% of patients with a pelvic abscess. The authors concluded that a mesocolic abscess by itself is not an absolute indication for colectomy.
Dharmarajan et al[12] showed that 93% (25 of 27) of their acute diverticulitis patients who presented with stable examination results, and distant free air on computed tomography, were successfully managed without urgent surgery, with 37% of these patients receiving percutaneous drains. Costi et al[34] reported a 92.3% (36 of 39) success rate for nonoperative management in patients with diverticulitis and a pneumoperitoneum, excluding those with hemodynamic instability and/or diffuse extravasation of rectal contrast on computed tomography.
The limitations of our study are its relatively short follow-up and retrospective nature. Furthermore, multiple individual surgeons managed patients, and selection criteria for nonoperative management were not standardized. Our univariate analysis shows that the risk of elective colectomy decreased after 2010, probably reflecting the time required for surgeons from our department to take ownership of this new concept.
However, these data still provide a valuable insight into the natural history of complicated diverticular disease, and might be considered preliminary to a future, multicenter prospective trial to better define target groups for prophylactic resection in this very prevalent and pervasive disease.
In our opinion, the decision to proceed to elective laparoscopic colectomy should not be automatic, but should taken on a case-by-case basis. Transplant patients, immunocompromised patients, or patients who need treatment that increases the risk of perforation (NSAID, steroids etc.), may be proposed for prophylactic sigmoid resection[35], even if the benefit of this approach has not been demonstrated[36,37].
Elective surgery for diverticular disease is intended to treat complications (fistula and symptomatic stenosis) or rare patients with recurrent and disabling bouts of diverticulitis.
A conservative policy is both feasible and safe in 71% of cases, with a low short-term recurrence risk.
We propose that after a complicated episode of diverticulitis treated nonoperatively, elective colectomy should be offered to treat complications (fistula and symptomatic stenosis), or for rare patients with recurrent and disabling bouts of diverticulitis. This attitude warrants further confirmation with larger cohorts.
We are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for reviewing the manuscript’s English.
Although sigmoid complicated diverticulitis has increased in recent years, questions remain concerning the therapeutic strategies in an acute setting, and after conservative treatment has been successful.
It is generally acknowledged that elective resection should be performed after complicated acute diverticulitis to avoid the high risk of recurrence and further complications. However, recent studies have highlighted the fact that an episode of severe diverticulitis may result in a buttressing effect around the affected portion of the colon, thereby protecting it from subsequent attacks.
The authors report the outcomes of 114 patients admitted for complicated diverticulitis (Hinchey I or II and/or extraluminal air). Of these 114 patients, 81 were managed by medical treatment only. After a median follow-up of 32 mo (4-63), six patients (7%) had developed a recurrent episode of diverticulitis at a median follow-up of 12 mo (6-36), but no patient required hospitalization. Of the 81 patients managed nonoperatively, 68 (84%) were asymptomatic and 13 (16%) had recurrent abdominal pain.
This study results suggested that a conservative approach is feasible in 71% of cases after an episode of complicated diverticulitis (CD). Indications for elective sigmoid resection should not be based solely on CD episode. This approach has an impact not only for the patient, but also for society.
Complicated diverticulitis is defined on computed tomography by the presence of a mesocolic abscess, pelvic abscess or extraluminal air. Pelvic abscesses are those located below the pelvic brim, and mesocolic abscesses are those located above the pelvic brim.
This study shows that in patients with complicated acute diverticulitis, conservative management is a “possible” approach in over 70% of cases. This is an encouraging result based on a retrospective design that could lead to superselection of patients with the best prognosis.
P- Reviewers: Festa V, Lange JF, Melton GB, Ribas Y, Tursi A, Smedh K S- Editor: Qi Y L- Editor: Stewart G E- Editor: Zhang DN
| 1. | Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 315] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 2. | Commane DM, Arasaradnam RP, Mills S, Mathers JC, Bradburn M. Diet, ageing and genetic factors in the pathogenesis of diverticular disease. World J Gastroenterol. 2009;15:2479-2488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 94] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Etzioni DA, Mack TM, Beart RW, Kaiser AM. Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 412] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 4. | Köhler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13:430-436. [PubMed] |
| 5. | Ambrosetti P, Grossholz M, Becker C, Terrier F, Morel P. Computed tomography in acute left colonic diverticulitis. Br J Surg. 1997;84:532-534. [PubMed] |
| 6. | Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85-109. [PubMed] |
| 7. | Rafferty J, Shellito P, Hyman NH, Buie WD. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 231] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 9. | Gaertner WB, Willis DJ, Madoff RD, Rothenberger DA, Kwaan MR, Belzer GE, Melton GB. Percutaneous drainage of colonic diverticular abscess: is colon resection necessary? Dis Colon Rectum. 2013;56:622-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864-874. [PubMed] |
| 11. | Ricciardi R, Baxter NN, Read TE, Marcello PW, Hall J, Roberts PL. Is the decline in the surgical treatment for diverticulitis associated with an increase in complicated diverticulitis? Dis Colon Rectum. 2009;52:1558-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Dharmarajan S, Hunt SR, Birnbaum EH, Fleshman JW, Mutch MG. The efficacy of nonoperative management of acute complicated diverticulitis. Dis Colon Rectum. 2011;54:663-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 138] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 13. | Singh B, May K, Coltart I, Moore NR, Cunningham C. The long-term results of percutaneous drainage of diverticular abscess. Ann R Coll Surg Engl. 2008;90:297-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | Chapman J, Davies M, Wolff B, Dozois E, Tessier D, Harrington J, Larson D. Complicated diverticulitis: is it time to rethink the rules? Ann Surg. 2005;242:576-581; discussion 581-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 190] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 15. | Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, Essani R, Beart RW. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100:910-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 346] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 16. | Evans J, Kozol R, Frederick W, Voytavich A, Pennoyer W, Lukianoff A, Lardner J. Does a 48-hour rule predict outcomes in patients with acute sigmoid diverticulitis? J Gastrointest Surg. 2008;12:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Mueller MH, Glatzle J, Kasparek MS, Becker HD, Jehle EC, Zittel TT, Kreis ME. Long-term outcome of conservative treatment in patients with diverticulitis of the sigmoid colon. Eur J Gastroenterol Hepatol. 2005;17:649-654. [PubMed] |
| 18. | Chapman JR, Dozois EJ, Wolff BG, Gullerud RE, Larson DR. Diverticulitis: a progressive disease? Do multiple recurrences predict less favorable outcomes? Ann Surg. 2006;243:876-830; discussion 880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 19. | Eglinton T, Nguyen T, Raniga S, Dixon L, Dobbs B, Frizelle FA. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Collins D, Winter DC. Elective resection for diverticular disease: an evidence-based review. World J Surg. 2008;32:2429-2433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 200] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
| 22. | Jeyarajah S, Faiz O, Bottle A, Aylin P, Bjarnason I, Tekkis PP, Papagrigoriadis S. Diverticular disease hospital admissions are increasing, with poor outcomes in the elderly and emergency admissions. Aliment Pharmacol Ther. 2009;30:1171-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 23. | Pessaux P, Muscari F, Ouellet JF, Msika S, Hay JM, Millat B, Fingerhut A, Flamant Y. Risk factors for mortality and morbidity after elective sigmoid resection for diverticulitis: prospective multicenter multivariate analysis of 582 patients. World J Surg. 2004;28:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Killingback M, Barron PE, Dent OF. Elective surgery for diverticular disease: an audit of surgical pathology and treatment. ANZ J Surg. 2004;74:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Oomen JL, Engel AF, Cuesta MA. Outcome of elective primary surgery for diverticular disease of the sigmoid colon: a risk analysis based on the POSSUM scoring system. Colorectal Dis. 2006;8:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Binda GA, Arezzo A, Serventi A, Bonelli L, Facchini M, Prandi M, Carraro PS, Reitano MC, Clerico G, Garibotto L. Multicentre observational study of the natural history of left-sided acute diverticulitis. Br J Surg. 2012;99:276-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 27. | Niederdellmann H, Schilli W, Ewers R, Akuamoa-Boateng E. Photoelestic behavior of osteosynthesis plates with different arrangement of screw holes for mandibular fractures. Int J Oral Surg. 1975;4:27-31. [PubMed] |
| 28. | Thörn M, Graf W, Stefànsson T, Påhlman L. Clinical and functional results after elective colonic resection in 75 consecutive patients with diverticular disease. Am J Surg. 2002;183:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Benn PL, Wolff BG, Ilstrup DM. Level of anastomosis and recurrent colonic diverticulitis. Am J Surg. 1986;151:269-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 135] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Thaler K, Baig MK, Berho M, Weiss EG, Nogueras JJ, Arnaud JP, Wexner SD, Bergamaschi R. Determinants of recurrence after sigmoid resection for uncomplicated diverticulitis. Dis Colon Rectum. 2003;46:385-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 31. | Levack MM, Savitt LR, Berger DL, Shellito PC, Hodin RA, Rattner DW, Goldberg SM, Bordeianou L. Sigmoidectomy syndrome? Patients’ perspectives on the functional outcomes following surgery for diverticulitis. Dis Colon Rectum. 2012;55:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | Egger B, Peter MK, Candinas D. Persistent symptoms after elective sigmoid resection for diverticulitis. Dis Colon Rectum. 2008;51:1044-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 33. | Ambrosetti P, Chautems R, Soravia C, Peiris-Waser N, Terrier F. Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 cases. Dis Colon Rectum. 2005;48:787-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 138] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 34. | Costi R, Cauchy F, Le Bian A, Honart JF, Creuze N, Smadja C. Challenging a classic myth: pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery in hemodynamically stable patients. A 10-year experience with a nonoperative treatment. Surg Endosc. 2012;26:2061-2071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 35. | Klarenbeek BR, Samuels M, van der Wal MA, van der Peet DL, Meijerink WJ, Cuesta MA. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251:670-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 36. | Hwang SS, Cannom RR, Abbas MA, Etzioni D. Diverticulitis in transplant patients and patients on chronic corticosteroid therapy: a systematic review. Dis Colon Rectum. 2010;53:1699-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 37. | Biondo S, Borao JL, Kreisler E, Golda T, Millan M, Frago R, Fraccalvieri D, Guardiola J, Jaurrieta E. Recurrence and virulence of colonic diverticulitis in immunocompromised patients. Am J Surg. 2012;204:172-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |