Published online Jun 14, 2014. doi: 10.3748/wjg.v20.i22.7005
Revised: January 8, 2014
Accepted: March 6, 2014
Published online: June 14, 2014
Processing time: 225 Days and 2.4 Hours
AIM: To discuss the imaging anatomy about pancreaticobiliary ductal union, occurrence rate of pancreaticobiliary maljunction (PBM) and associated diseases in a Chinese population by using magnetic resonance cholangiopancreatography (MRCP).
METHODS: Data were collected from 694 patients who underwent MRCP from January 2010 to December 2012. Three hundred and ninety-three patients were male and 301 patients were female. The age range was 16-92 years old and the average age was 51.8 years. The recruitment indication of all cases was patients who had clinical symptoms, such as abdominal pain, jaundice, nausea and vomiting, which thus were clinically suspected as relative pancreaticobiliary diseases. All cases were examined by MRCP using single-shot fast spin-echo sequences. In order to obtain MRCP images, the maximum intensity projection was used.
RESULTS: According to the anatomy of pancreaticobiliary ductal union based on our analysis of MRCP images, all cases were classified into normal type and abnormal type according to the position of pancreaticobiliary ductal union. The abnormal type could be further divided into P-B type, B-P type and the duodenum type. By analyzing the incidence of biliary stone and inflammation, pancreatitis, biliary duct tumors and pancreatic tumors between normal and abnormal types, significant differences existed. The abnormal group was more likely to suffer from pancreaticobiliary diseases. Comparing three different types of PBM that were associated with pancreaticobiliary diseases by using Fisher’s method, the result showed that there was no significant difference in the incidence of biliary stones, cholecystitis and pancreatic tumors. The incidence of pancreatitis in B-P type and P-B type was higher than that in duodenum type; the incidence of biliary duct tumor in B-P type was higher than that in P-B type; the incidence of biliary duct tumor in duodenum type was lower than that in P-B type. The incidence of congenital choledochus dilatation in normal type and abnormal type was similar, and there was no significant difference between the two types.
CONCLUSION: Types of PBM are closely related to the occurrence of pancreaticobiliary diseases. MRCP has important clinical value in the early diagnosis and preventive treatment of pancreaticobiliary diseases.
Core tip: This article analyzed the types of pancreaticobiliary ductal union, pancreaticobiliary maljunction (PBM) and associated diseases in a Chinese population by observing the anatomical characteristics of the pancreaticobiliary duct of patients who underwent magnetic resonance imaging and magnetic resonance cholangiopancreatography (MRCP), and found that types of PBM are closely related to the occurrence of pancreaticobiliary diseases, particularly pancreatitis, biliary duct tumors and pancreatic tumors. MRCP has important value in the early diagnosis and preventive treatment of pancreaticobiliary diseases.
- Citation: Wang CL, Ding HY, Dai Y, Xie TT, Li YB, Cheng L, Wang B, Tang RH, Nie WX. Magnetic resonance cholangiopancreatography study of pancreaticobiliary maljunction and pancreaticobiliary diseases. World J Gastroenterol 2014; 20(22): 7005-7010
- URL: https://www.wjgnet.com/1007-9327/full/v20/i22/7005.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i22.7005
Recently, pancreaticobiliary maljunction and its related pancreaticobiliary diseases promised to be areas of intense interest, particularly for Japanese scholars. However, the reported results about anatomical characteristics of pancreaticobiliary maljunction and its typing were mostly on the basis of autopsy and endoscopic retrograde choledochopancreatography (ERCP)[1]. Magnetic resonance cholangiopa-ncreatography (MRCP) is a noninvasive cholangiopancreatography technique which rapidly popularized in clinical use in the 1990s. With the principle that the hydrated pancreaticobiliary duct could be depicted clearly on MR images (MRI) by using heavy T2-weighted sequences, its anatomical structure would be shown as well. This study analyzed the type of pancreaticobiliary ductal union, pancreaticobiliary maljunction (PBM) and the associated diseases in a Chinese population by observing the pancreaticobiliary duct and the anatomical characteristics of patients who underwent MRI and MRCP.
Data of 963 patients who underwent MRI and MRCP from January 2010 to December 2012 were collected. The recruitment indication of all cases was patients who had clinical symptoms, such as abdominal pain, jaundice, nausea and vomiting, which thus were clinically suspected as relative pancreaticobiliary diseases. Two hundred and sixty-nine cases were excluded from analysis due to postoperative examination or poor image quality. Six hundred and ninety-four cases met the diagnostic requirement for this study. Three hundred and ninety-three patients were male and the other 301 patients were female. The age range was 16-92 years and the average age was 51.8 years. All cases were initially suspected of having pancreatic biliary diseases.
SIEMENS Avanto 1.5 Tesla superconducting magnetic resonance scanner was used in the study. Heavy T2-weighted images were originally achieved using a gradient-echo balanced steady-state free precession technique. A fast spin-echo pulse sequence with a long echo time (TE) was then introduced. Non-breath-hold techniques (with respiratory triggering) were used, with images obtained either as a two-dimensional or three-dimensional (3D) acquisition. A 3D technique provides a higher signal to noise ratio, which is traded off for thinner contiguous slices (repetition time 2500 ms, TE 681 ms, slice thickness 1.00 mm, field of view 380 mm). Acquiring images with near isotropic voxels allows improved post-processing manipulation of the images with multi-planar reconstruction, maximum intensity projection and volume rendering.
Normal type: Common bile duct and main pancreatic duct join in the duodenal wall, but the length of the common channel is ≤ 8 mm.
Anomalous union: The main pancreatic duct and the common bile duct open at the second part of the duodenum respectively or after joining as a common channel, which is > 8 mm. It is further divided into P-B type (joining of common bile duct with pancreatic duct), B-P type (joining of pancreatic duct with common bile duct) and duodenum type (the main pancreatic duct and the common bile duct open into different parts of the duodenum).
MRI and MRCP images were comprehensively analyzed and diagnosed by 3 senior radiologists. The index below was observed: (1) the existence of common duct and its length; (2) the existence of pancreaticobiliary maljunction and its type; and (3) the diagnosis of pancreaticobiliary disease. In case of any differences in diagnostic opinion, an agreement should be reached for reference. The results underwent statistical analysis by SPSS 17.0.
PBM is a congenital anomaly defined as a junction of the pancreatic and bile ducts located outside the duodenal wall, and usually forming a markedly long common channel. The action of the sphincter of oddi does not have a functional impact on the junction of the pancreatic and bile ducts. The normal length of the common duct does not have a unified diagnosis standard, yet most literature reported the length of the long common channel was ≥ 8 mm, 12 mm, or 15 mm[2-4]. Three hundred and twenty-six cases in this study could show common ducts clearly by MRCP, and the average length was 7.9 mm. We thus defined long common duct as a common channel with length ≥ 8 mm. The incidence of pancreaticobiliary diseases in < 8 mm group was found to be higher than that in the common duct ≥ 8 mm group.
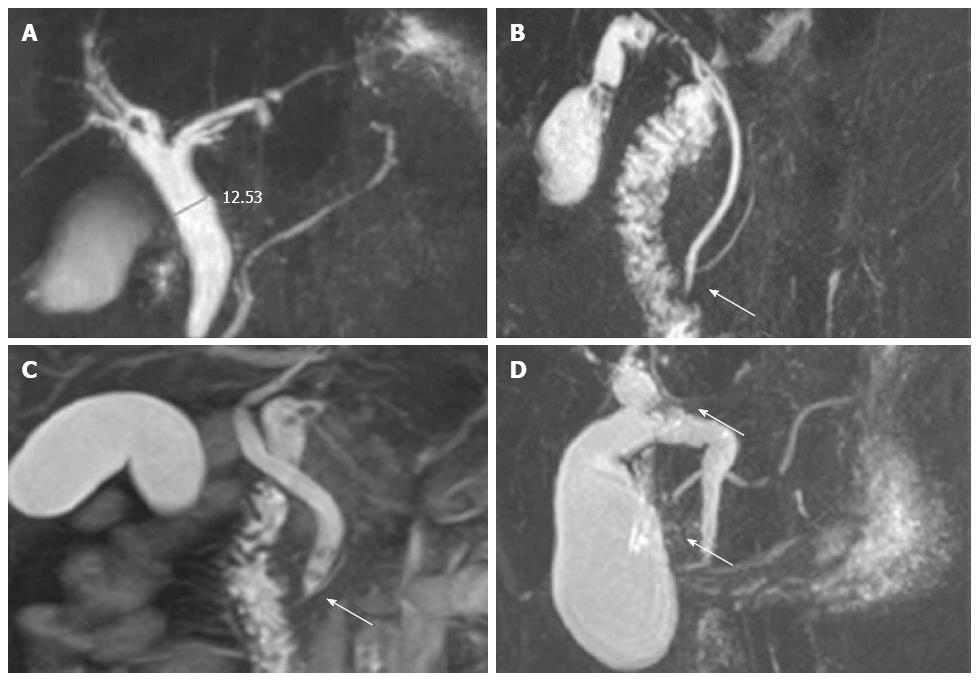
In all 694 cases, 453 cases (65.3%) were classified as normal type (Figure 1A), and 241 cases (34.7%) were anomalous union. In the anomalous group, 84 cases (12.1%) were P-B type (Figure 1B), 85 cases (12.2%) were B-P type (Figure 1C), and 72 cases (10.4%) were duodenal type (Figure 1D). The typing results of all 694 cases were shown in Table 1.
| Results | Type | Case |
| Normal type | 453 (65.3) | |
| P-B type | 84 (12.1) | |
| Abnormal type | B-P type | 85 (12.2) |
| Duodenal type | 72 (10.4) | |
| Total | 694 (100.0) |
In the normal type group (453 cases), 357 cases (78.8%) suffered from biliary stones combined with cholecystitis, while 33 cases (7.3%) suffered from pancreatitis, and 9 cases (2.0%) suffered from biliary duct tumors, and only 1 case (0.2%) suffered from pancreatic tumor. In the anomalous union type group (241 cases), 187 cases (77.6%) suffered from biliary stone and cholecystitis, while 33 cases (13.7%) had pancreatitis, 17 cases (7.1%) had biliary duct tumors and 1 case (0.4%) had a pancreatic tumor (Table 2). In order to compare the differences of corresponding diseases between the normal type group and the abnormal type group, the data underwent a statistical variance test. The differences between the two groups presented statistical significance (P < 0.05). There were differences in the incidence of pancreaticobiliary diseases in different types of PBM (Table 2). Sixty-five cases combined with biliary stone and cholecystitis, and 18 cases with pancreatitis, 4 cases with biliary duct tumor, and 3 cases with pancreatic tumor were in P-B type; 62 cases combined with biliary stone and cholecystitis, and 21 cases with pancreatitis, 11 cases with biliary duct tumor, and 3 cases with pancreatic tumor were in B-P type; and 60 cases combined with biliary stone and cholecystitis, and 3 cases with pancreatitis, 2 cases with biliary duct tumor, and 3 cases with pancreatic tumor were in the duodenal type. In order to compare differences of corresponding diseases in the three abnormal types, the data underwent Fisher’s exact test and the result showed that there was no significant differences in the incidence of biliary stone, cholecystitis and pancreatic tumor (P > 0.05). The incidence of pancreatitis in the B-P type and the P-B type was higher than that in the duodenum type (P < 0.05) and the incidence of biliary duct tumor in the B-P type was higher than that in the P-B type. The incidence of biliary duct tumors in the duodenum type was lower than that in the P-B type (P < 0.05).
| Type | Biliary inflammation | Biliary tumor | Pancreatic inflammation | Pancreatic tumor | |||||
| Y | N | Y | N | Y | N | Y | N | ||
| Types of union | Normal type | 357 | 96 | 9 | 444 | 33 | 420 | 1 | 452 |
| Abnormal type | 187 | 54 | 17 | 224 | 42 | 199 | 9 | 232 | |
| P value | 0.390 | 0.001 | 0.000 | 0.001 | |||||
| Types of union | P-B type | 65 | 19 | 4 | 80 | 18 | 66 | 3 | 81 |
| B-P type | 62 | 23 | 11 | 74 | 21 | 64 | 3 | 82 | |
| Duodenum type | 60 | 12 | 2 | 70 | 3 | 69 | 3 | 69 | |
| P value | 0.501 | 0.006 | 0.022 | 0.002 | |||||
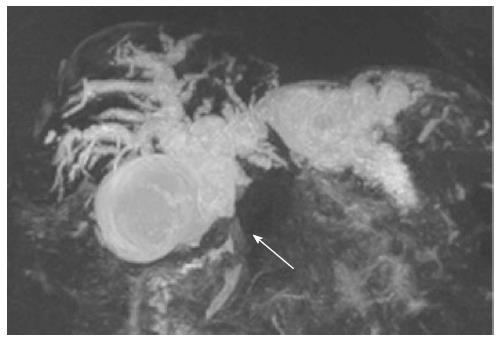
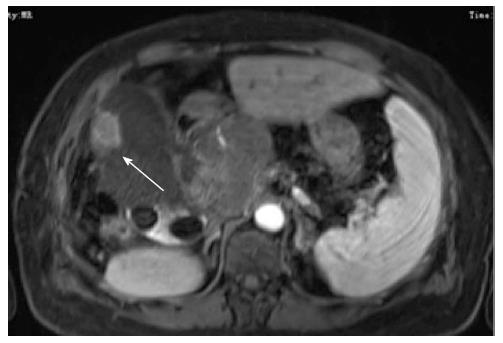
Matsumoto et al[5] found that congenital choledochus dilatation (CCD) was closely related to PBM, as they all originated from the 10th week of embryonic development; whereas Deng et al[6] thought that PBM and CCD were both independent diseases, and they were different either in histology and embryology or in pathology. We analyzed cases combined with CCD in normal type (n = 453) and abnormal type (n = 241), and found that the incidence of CCD in normal type (n = 186) and abnormal type (n = 111) are similar, and there was no significant difference between the two types.
PBM was recorded in the early 20th century, but named PBM officially in 1969; this name is still in use today[7]. Suda et al[8] found that pancreaticobiliary diseases were mainly caused by backflow of pancreatic juice and bile. The main anatomical feature of PBM is that the bile duct and pancreatic duct join out of the duodenal wall forming a lengthy common duct, often combined with sphincter of Oddi dysplasia; thereby the pancreatic duct and bile duct are out of control, causing backflow of pancreatic juice and bile. There is still no unified recognition about the normal length of the common duct, and many literatures reported the length of common duct ≥ 8 mm, 12 mm or 15 mm as abnormality[2-4]. The average length of the common duct measured in MRCP images of this study was 7.9 mm, so the length ≥ 8 mm was taken as the standard to define normal and abnormal common duct in the contrast study. We found that the incidence of pancreaticobiliary diseases in < 8 mm group was higher than that in the common duct ≥ 8 mm group, therefore taking 8 mm as the standard is thought to be appropriate. The definition of PBM has two meanings: (1) bile duct and pancreatic duct join out of the duodenal wall to form a long common duct that ≥ 8 mm; and (2) bile duct and pancreatic duct do not join and open into the duodenal wall separately.
The results of studies about the incidence of PBM were inconsistent. ERCP reported that the incidence was only 0.9%-6.2%, whereas autopsy reported the incidence reached 61.8%-70%[9,10]. Two hundred and forty-one cases showed PBM in the symptomatic group (694 cases) in this article, and the incidence was 34.7%, which was much higher than the ERCP study but lower than autopsy findings reported in literature. This may be related with patient selection, examination method, sample size and other factors.
PBM classification was first found in surgical and pathological reports. Clinicians began paying attention to intravital studies about PBM along with the appearance of various cholangiography techniques. In 1977, Kimura et al[3] classified PBM into type I (pancreatic duct: bile duct type or acute angle type) and type II (bile duct: pancreatic duct type or right angle type). Warshaw et al[10] amended the above-mentioned typing method and proposed classifying PBM into type I-III. Obara et al[11] studied PBM classification integrally and completely with 50 cases, and concluded that type I and type II were the same as Warshaw’s work, but took type III as a complex type which was further classified into three subtypes (a, b, and c type). This method is still in use today. Cases with PBM in this article were classified into three types (P-B type, B-P type and duodenum type), but there was no complex type cases in the symptomatic group. This may be related with patients from different races, different examination methods, restricted MRCP spatial resolution and other relative factors.
Data in this article show that PBM is closely related to the occurrence of pancreatitis, biliary duct tumor and pancreatic tumor; particularly, the incidence of biliary duct tumor is significantly raised in B-P type. This may be related with flow direction of pancreatic juice. The pressure in the normal pancreatic duct is higher than that in the common duct group, which causes a continuous reciprocal reflux of pancreatic juice and bile which might chronically stimulate biliary epithelial cells, initiate gene mutation, activate oncogenes and inactivate tumor suppressor genes. Biliary epithelial cells then undergo hyperplasia, metaplasia and, finally, carcinogenesis[12]. Relationships of PBM and CCD were studied by many scholars; some of them thought that PBM and CCD were related to each other to a certain extent, whereas some thought they didn’t have much relationship[5,6]. This study combined CCD in a normal group and a PBM group, and found that the incidence of CCD in the two groups was not significantly different. Therefore, PBM and CCD are supposed to be two independent diseases (Figures 2 and 3).
This study has important clinical significance to comprehend the anatomic features of pancreaticobiliary duct union and PBM types: (1) it is beneficial to the differential diagnosis of lesions in the pancreatic head, ampullary region, duodenal papilla, and pancreaticobiliary duct; (2) it provides reference information for clinical diagnosis according to the pathological anatomy of PBM and its relationship with pancreaticobiliary diseases in Chinese people; (3) patients with PBM, particularly with recurrent biliary inflammation and pancreatitis, could be given preventive treatment when necessary; and (4) patients with PBM which has a close relationship with pancreaticobiliary malignant tumors should be paid great attention clinically.
There are also some limitations to this study. This study is analyzed on the basis of a symptomatic group, but not based on MRCP performed in a healthy population followed for many years after the MRI, so the incidence of PBM and its relationship with pancreaticobiliary diseases obtained in this study only represents the symptomatic group. Nonetheless, it still has much clinical significance.
Most of the reported results about anatomical characteristics of pancreaticobiliary maljunction (PBM) and its typing were on the basis of autopsy and endoscopic retrograde choledochopancreatography. Magnetic resonance cholangiopancreatography (MRCP) is an atraumatic cholangiopancreatography technique, and there is no study on PBM and its related diseases, particularly differences in the incidence of biliary stone, cholecystitis, pancreatitis, biliary duct tumor and pancreatic tumor in three PBM types on large sample.
The authors demonstrated that PBM are closely related to the occurrence of pancreaticobiliary diseases, particularly pancreatitis, biliary duct tumor and pancreatic tumor. The incidences of certain pancreaticobiliary diseases are different in the three PBM types.
This article analyzed the types of pancreaticobiliary ductal union, PBM and associated diseases in Chinese people by observing the pancreaticobiliary duct and the anatomic characteristics of patients who underwent magnetic resonance imaging and MRCP. Since this clinical study included a large sample of patients, the relationship of PBM and pancreaticobiliary diseases could be elaborated.
MRCP has important value in the early diagnosis and preventive treatment of pancreaticobiliary diseases, and it could provide important information for clinical diagnosis and further comprehension of the anatomy of pancreaticobiliary duct union benefitting from the development of medical image examination machines and imaging techniques.
This is an interesting retrospective study of clinical relevance. The relation between PBM and pancreaticobiliary disorders is a wellknown issue. Authors have handled and discussed this topic extensively in the manuscript.
P- Reviewers: Chetty R, Chiaro MD, Coskun A, Kamisawa T S- Editor: Gou SX L- Editor: O’Neill M E- Editor: Ma S
| 1. | Kamisawa T, Takuma K, Itokawa F, Itoi T. Endoscopic diagnosis of pancreaticobiliary maljunction. World J Gastrointest Endosc. 2011;3:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Misra SP, Dwivedi M. Pancreaticobiliary ductal union. Gut. 1990;31:1144-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 67] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Kimura K, Ohto M, Saisho H, Unozawa T, Tsuchiya Y, Morita M, Ebara M, Matsutani S, Okuda K. Association of gallbladder carcinoma and anomalous pancreaticobiliary ductal union. Gastroenterology. 1985;89:1258-1265. [PubMed] |
| 4. | Misra SP, Gulati P, Thorat VK, Vij JC, Anand BS. Pancreaticobiliary ductal union in biliary diseases. An endoscopic retrograde cholangiopancreatographic study. Gastroenterology. 1989;96:907-912. [PubMed] |
| 5. | Matsumoto Y, Fujii H, Itakura J, Mogaki M, Matsuda M, Morozumi A, Fujino MA, Suda K. Pancreaticobiliary maljunction: etiologic concepts based on radiologic aspects. Gastrointest Endosc. 2001;53:614-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Deng YL, Cheng NS, Lin YX, Zhou RX, Yang C, Jin YW, Xiong XZ. Relationship between pancreaticobiliary maljunction and gallbladder carcinoma: meta-analysis. Hepatobiliary Pancreat Dis Int. 2011;10:570-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Babbitt DP. [Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb]. Ann Radiol (Paris). 1969;12:231-240. [PubMed] |
| 8. | Suda K, Miyano T, Suzuki F, Matsumoto M, Yamashiro Y, Tokumaru T, Oyama T, Matsumoto Y. Clinicopathologic and experimental studies on cases of abnormal pancreatico-choledocho-ductal junction. Acta Pathol Jpn. 1987;37:1549-1562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Hu B, Gong B, Zhou DY. Association of anomalous pancreaticobiliary ductal junction with gallbladder carcinoma in Chinese patients: an ERCP study. Gastrointest Endosc. 2003;57:541-545. [PubMed] |
| 10. | Warshaw AL, Simeone JF, Schapiro RH, Flavin-Warshaw B. Evaluation and treatment of the dominant dorsal duct syndrome (pancreas divisum redefined). Am J Surg. 1990;159:59-64; discussion 64-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 113] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Obara T, Tanno S, Fujii T, Izawa T, Mizukami Y, Yanagawa N, Ura H, Kohgo Y. Epithelial cell proliferation and gene mutation in the mucosa of gallbladder with pancreaticobiliary malunion and cancer. J Hepatobiliary Pancreat Surg. 1999;6:229-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Kasuya K, Nagakawa Y, Matsudo T, Ozawa T, Tsuchida A, Aoki T, Itoi T, Itokawa F. p53 gene mutation and p53 protein overexpression in a patient with simultaneous double cancer of the gallbladder and bile duct associated with pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg. 2009;16:376-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |