Published online Jun 14, 2014. doi: 10.3748/wjg.v20.i22.6968
Revised: January 6, 2014
Accepted: February 17, 2014
Published online: June 14, 2014
Processing time: 268 Days and 16 Hours
AIM: To review the usefulness of endoscopic biliary stenting for obstructive jaundice caused by hepatocellular carcinoma and identify problems that may need to be addressed.
METHODS: The study population consisted of 36 patients with obstructive jaundice caused by hepatocellular carcinoma (HCC) who underwent endoscopic biliary stenting (EBS) as the initial drainage procedure at our hospital. The EBS technical success rate and drainage success rate were assessed. Drainage was considered effective when the serum total bilirubin level decreased by 50% or more following the procedure compared to the pre-drainage value. Survival time after the procedure and patient background characteristics were assessed comparatively between the successful drainage group (group A) and the non-successful drainage group (group B). The EBS stent patency duration in the successful drainage group (group A) was also assessed.
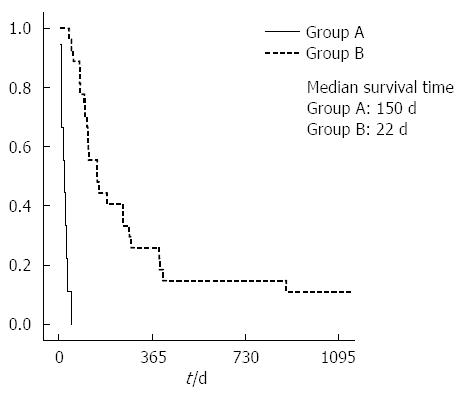
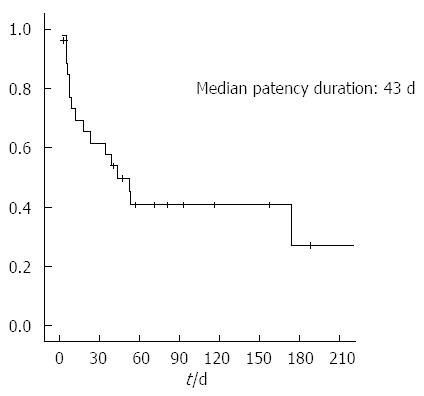
RESULTS: The technical success rate was 100% for both the initial endoscopic nasobiliary drainage and EBS in all patients. Single stenting was placed in 21 patients and multiple stenting in the remaining 15 patients. The drainage successful rate was 75% and the median interval to successful drainage was 40 d (2-295 d). The median survival time was 150 d in group A and 22 d in group B, with the difference between the two groups being statistically significant (P < 0.0001). There were no statistically significant differences between the two groups with respect to patient background characteristics, background liver condition, or tumor factors; on the other hand, the two groups showed statistically significant differences in patients without a history of hepatectomy (P = 0.009) and those that received multiple stenting (P = 0.036). The median duration of stent patency was 43 d in group A (2-757 d). No early complications related to the EBS technique were encountered. Late complications occurred in 13 patients (36.1%), including stent occlusion in 7, infection in 3, and distal migration in 3.
CONCLUSION: EBS is recommended as the initial drainage procedure for obstructive jaundice caused by HCC, as it appears to contribute to prolongation of survival time.
Core tip: Taking into account quality of life, percutaneous transhepatic biliary drainage is normally carried out as a first choice endoscopic biliary stenting in recent years. The resulting prolonged survival time was observed as significantly different when the non-successful group was compared to the successful group. Obstructive jaundice caused by hepatocellular carcinoma is a complex disease state; therefore endoscopic biliary stenting should be investigated from a different viewpoint from that of biliary drainage performed for other malignant biliary obstructions, such as bile duct carcinoma.
- Citation: Sugiyama G, Okabe Y, Ishida Y, Saitou F, Kawahara R, Ishikawa H, Horiuchi H, Kinoshita H, Tsuruta O, Sata M. Evaluation of endoscopic biliary stenting for obstructive jaundice caused by hepatocellular carcinoma. World J Gastroenterol 2014; 20(22): 6968-6973
- URL: https://www.wjgnet.com/1007-9327/full/v20/i22/6968.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i22.6968
It has been reported that concurrent obstructive jaundice due to tumor invasion of the bile ducts in hepatocellular carcinoma (HCC) is less frequent (incidence: 0.5%-13%) than tumor invasion of the portal vein or that of the hepatic vein[1-3]. With the advances made in HCC diagnosis and treatment techniques in recent years, the rates of early tumor diagnosis and long-term survival have been increasing; however, it is not uncommon for treatment to involve grave difficulties, for the prognosis to become unfavorable in patients in whom intercurrent obstructive jaundice develops, and for it to rapidly progress to hepatic failure[3]. Conventionally, percutaneous transhepatic biliary drainage (PTBD) has usually been carried out for the treatment of obstructive jaundice caused by HCC; however, in recent years, endoscopic biliary stenting (EBS) has often been undertaken as first-line therapy to take into account the quality of life[4-6] of the patients. Drainage for obstructive jaundice caused by HCC, nevertheless, often entails greater difficulty as compared to drainage for biliary strictures caused by other malignancies than HCC.
Herein, we carried out a retrospective analysis of the outcomes of EBS for obstructive jaundice caused by HCC undertaken at our hospital, in an attempt to review the usefulness of the procedure and identify problems that may need to be addressed.
The study population consisted of 36 HCC patients with obstructive jaundice caused by direct invasion of the bile duct or hemobilia associated with a tumor who underwent EBS as initial external biliary drainage at our hospital between March 2003 and December 2012.
In HCC patients with suspected obstructive jaundice caused by a tumor, the patient’s hepatic functional reserve (Child-Pugh score) was evaluated from blood biochemical test data. Pertinent data obtained during the non-icteric state were utilized as reference, insomuch as the total bilirubin (TB) is elevated in this disease state. Subsequently, the patient was examined to identify sites of large bile duct obstruction by diagnostic imaging, including abdominal ultrasonography and computed tomography. In addition, clinical stage and PVTT was determined according to the criteria of the Liver Cancer Study Group of Japan[7]. PVTT grading was as follows: Vp0, no PVTT; Vp1, tumor thrombus in a third or more of the peripheral branches of the portal vein; Vp2, tumor thrombus in a second branch of the portal vein; Vp3, tumor thrombus in the first branch of the portal vein; and Vp4, tumor thrombus in the trunk of the portal vein.
Endoscopic retrograde cholangiopancreatography (ERCP) was performed with the patient under deep sedation using a duodenoscope (JF240, JF260V, Olympus Optical Co., Tokyo, Japan) in all cases. Upon confirming the site of the biliary stricture by endoscopic retrograde cholangiography (ERC), the stagnant bile was collected from upstream of the stricture using an ERCP catheter under the guidance of a guidewire and checked for any evidence of bile infection (and, if present, its severity) or hemorrhage. Initial drainage consisted of endoscopic nasobiliary drainage (ENBD) in patients positive for bile infection and/or hemorrhage. ENBD was inserted not only for the treatment of infection, but also to judge the biliary drainage effect. However, considering the prognosis, ENBD was not performed in either advanced cases of HCC or in poor cases of the general state, but it was performed in EBD from the beginning. If any blood clot was detected, an endoscopic sphincterotomy was carried out to extract the blood clots with basket and balloon catheters. Evaluation of tumor invasion to the bile ducts was then applied via the Bismuth-Corlette classification[8] followed by endoscopic placement of a nasobiliary drain. In cases where the ENBD had produced an external biliary drainage effect, nasobiliary drainage was later replaced with an EBS. Plastic stents (7 or 8.5 Fr) were used for ENBD and EBS. When the biliary drainage was insufficient or cholangitis developed, the additional procedure of either repeated EBS replacement or PTBD was undertaken.
ENBD or EBS technical success and drainage success rates were assessed. Drainage success was evaluated as (TB just prior to the procedure) = (lowest TB after the EBS)/(TB just prior to the procedure) × 100, and a drainage success rate of ≥ 50% was considered to indicate effectiveness. Furthermore, survival time (survival days: No. of days from initial drainage to death) and patient background characteristics were assessed comparatively between the successful drainage group (group A) and the non-successful drainage group (group B). EBS patency duration (No. of days from initial drainage stent patency to re-drainage or death) in the successful drainage group (group A) was also assessed. Procedure-related complications were also analyzed in relation to the clinical progression of HCC.
Medians (range) were determined for the measured variables. Comparisons between 2 groups were performed using the Mann-Whitney U test for continuous variables, and the χ2 test for discrete variables. Drainage patency and survival rate were evaluated by the Kaplan-Meier method and compared by the Log-Rank test.
Patient characteristics for those who underwent EBS in this study are shown in Table 1. In total, there were 36 patients in the study, consisting of 30 males and 6 females. The median age of the patients was 65 (37-83) years, and the underlying liver disorder was chronic hepatitis in 3 patients [hepatitis B virus (HBV)/hepatitis C virus (HCV)/non-BC= 1/0/2] and cirrhosis in the remaining 33 patients (HBV/HCV/non-BC= 8/23/2). The Child-Pugh score prior to the development of jaundice in the patients with cirrhosis was A/B/C = 8/19/3 cases (excluding 3 cases with insufficient data). The clinical stage was stage II, III/IVa/IVb = 3/29/4 according to the General Rules for the Clinical and Pathological Study of Primary Liver Cancer, 5th edition, 2009[7]. PVTT was evident in 23 patients (Vp0-2/3/4 = 19/11/6), and hemobilia in 12.
| Total number of patients | 36 |
| Age, yr (mean) | 65 (37-83) |
| Gender, male/female | 30/6 |
| Etiology, HBV/HCV/non-BC | 9/23/4 |
| Chronic hepatitis/liver cirrhosis | 3/33 |
| Child-Pugh score, A/B/C | 8/19/3 |
| Hepatocellular carcinoma, stage I/II/IIIa/IVb | 1/2/29/4 |
| Grade of portal vein invasion, VP0-2/VP3/VP4 | 19/11/6 |
| Previous treatment for Hepatocellular carcinoma, Y/N | 26/10 |
| Location of bile duct obstruction, intrahepatic/extrahepatic | 13/23 |
| Location of bile duct stricture, unilobular/bilobular | 11/25 |
| Hemobilia, present/absent | 12/24 |
| Following treatment for hepatocellular carcinoma, Y/N | 15/21 |
The technical success rate was 100% for both initial ENBD and EBS in all patients. The cases in which ENBD was previously performed consisted of 11 patients in group A and 7 patients in group B. There was only one case in group A in which infection existed in the initial drainage.
A single stent was placed in 21 patients and multiple stents in 15 patients. The drainage was successful in 27 patients (75%), and the median interval to successful drainage was 40 d (2-295 d).
Statistical analysis of the data did not reveal any significant differences between group A and group B with respect to patient background characteristics (age, gender, and hepatitis virus marker profile), background liver (hepatic functional reserve), or tumor factors [tumor location, T-factor, stage, grade of portal vein invasion, or grade of bile duct invasion (Bismuth classification)] (Table 2). As for previous treatment, statistically significant differences were noted between the two groups in the number of patients without a history of hepatectomy (P = 0.009). The number of cases in which hepatectomy was carried out before the appearance of obstructive jaundice was 5 out of the 36 patients. The operation method consisted of: central bisegmentectomy being performed in 1 patient in group A, right hemihepatectomy in 2 patients in group B, left hemihepatectomy in 1 patient in group B, and limited hepatic resection in 1 patient in group B, with a number of patients receiving multiple stents (P = 0.036).
| Group A | Group B | P value | |
| Number | 27 | 9 | |
| Age, yr (range) | 67 (43-77) | 58 (37-77) | 0.168 |
| Gender, male/female | 22/5 | 8/1 | 0.848 |
| Etiology, HBV/HCV/non-BC | 6/17/4 | 3/6/0 | 0.432 |
| Child-Pugh score, A/B/C | 5/16/1 | 3/3/2 | 0.136 |
| Platelet count (× 104) | 12. 4 (3.0-22.7) | 11.1 (3.8-17.2) | 0.880 |
| Albumin (g/dL) | 3.1 (2.1-4.1) | 3.0 (2.2-4.0) | 0.755 |
| ALP, max (U/L) | 824 (365-4447) | 798 (422-1350) | 0.476 |
| PT (%) | 79 (45-117) | 74 (47-99) | 0.199 |
| Tumor size 2 cm over, Y/N | 19/8 | 5/4 | 0.888 |
| Tumor location, unilobular/bilobular | 12/15 | 4/5 | 0.652 |
| Hepatocellular carcinoma. | 15/12 | 5/4 | 0.647 |
| T1-T3/T4 | |||
| Grade of portal vein invasion, VP0-3/VP4 | 24/3 | 5/4 | 0.039 |
| VP, present/absent | 17/10 | 6/3 | 0.721 |
| Grade of bile duct invasion, Bismuth classification 1-3/4 | 16/11 | 6/3 | 0.782 |
| Previous treatment, Y/N | 18/9 | 9/0 | 0.046 |
| HAI, Y/N | 9/18 | 4/5 | 0.842 |
| TACE, Y/N | 8/19 | 4/5 | 0.888 |
| Interventional radiology, Y/N | 14/13 | 5/4 | 0.716 |
| Hepatectomy, Y/N | 1/26 | 4/5 | 0.009 |
| The number of stent, single/multiple | 13/14 | 8/1 | 0.036 |
At the time of statistical analysis, 35 patients had died (group A, n = 26; group B, n = 9), with only 1 patient (group A) surviving. The median survival time (MST) was 150 d in group A and 22 d in group B; the difference in survival between the two groups was statistically significant (P < 0.0001) (Figure 1). The median duration of stent patency in group A was 43 d (2-757 d) (Figure 2). PTBD was performed later in 2 of the 27 patients of group A (in anticipation of attaining an early external biliary drainage effect in one patient and because of hemobilia in 1 patient).
On the other hand, in group B, because of depressed performance status after EBS, PTBD and re-EBS could not be performed in all patients. Only conservative management was carried out, leading to a dismal prognosis.
No early complications associated with the EBS technique were encountered. Late complications occurred after endoscopic placement of biliary stenting in 13 patients (36.1%), including stent occlusion in 7 patients, infection in 3 patients, and distal migration in 3 patients; all these events were successfully managed by conservative treatment (such as re-EBS).
After EBS, treatment for HCC was performed in 15 of the 27 patients of group A. The treatment undertaken for HCC was: hepatectomy in 2 patients, interventional radiology in 12 patients, percutaneous radiofrequency ablation in 2 patients, radiation therapy in 1 patient, and administration of a molecular-targeted drug (sorafenib®) in 1 patient (with duplication). No treatment for HCC was undertaken in 12 of the 27 patients of group A due to various factors (e.g., depressed performance status and advanced age) or in any of the patients of group B.
Jaundice presents in 19%-40% of patients with HCC at the time of diagnosis and usually occurs in later stages. Obstructive jaundice is estimated to occur at an incidence rate of 0.5%-13%[1-3]. Obstructive jaundice caused by HCC was first reported by Mallory et al[1] in 1947. This type of jaundice has been described as more common among highly advanced cases and to be a disease state with a poor prognosis[3,9,10]. The following mechanisms for the genesis of obstructive jaundice caused by HCC have been postulated: (1) intraductal growth and invasion by the tumor per se; (2) impaction of tumor or necrotized tissue fragments coming off from a tumor or blood clots from hemorrhage; and (3) impingement by a large tumor or lymph node[11-13].
It was previously the case that PTBD was often performed for biliary drainage in the treatment for obstructive jaundice caused by HCC[14-16], but in recent years it has become more common for EBS to be undertaken instead when quality of life is taken into account[4-6]. The current widespread application of EBS seems to stem from the high success rate of EBS, the not insignificant risk of technique-related hemorrhage in PTBD, a shorter interval to tube replacement in PTBD, and superior stent patency duration in EBS[6]. Therefore, PTBD is currently applied as a second-line procedure in such cases as failure of EBS[17,18]. We basically chose EBS as the primary route, but in some patients, such as those with a decreased systematic state, endoscopy cannot possible. Surgery is also impossible in patients where the duodenal papilla cannot be reached by endoscopy due to abdominal surgery. PTBD is selected from the beginning in such cases, but we had no such cases in this study.
The drainage success rate with EBS was 75% in our study. Reported drainage success rates in the literature are in the range of 50%-75.9%[19-21], which are inferior to the results of EBS for malignant biliary obstructions, such as carcinoma of the bile duct[2,22,23]. Statistical analysis of data from studies that were performed to explore the factors responsible for such a poor drainage effect, including patient background characteristics, background liver factors, and tumor factors, failed to reveal any significant factors. There have been reports indicating poor drainage efficacy and lack of a survival prolongation effect in patients with VP3 or more advanced disease, as well as in patients with a total bilirubin level of ≥ 13 mg/dL or Child-Pugh class C disease[19]. Elements such as a difficulty in performing a strict evaluation of the hepatic functional reserve in the presence of jaundice, localization of HCC, the diversity of factors contributing to bile duct obstruction, and greater liability to bleeding in HCC are also considered to account for the difficulty inherent in the statistical analysis. On the other hand, in the present study, there was a statistically significant difference in the number of patients without a history of hepatectomy between group A and group B. This would suggest the possibility that such factors as reduced hepatic volume and the complex coursing of the bile duct might have influenced the drainage effect; an article that previously mentioned this in the past was not reported due to it being thought to be an examination error. A statistically significant difference was observed in the number of patients receiving multiple stents between group A and group B. It is thus inferred that proactive introduction of multiple stenting aimed at rapid biliary drainage proved efficacious because most HCC patients had chronic hepatic disorders. This differed from the results of stenting for the treatment of unresectable hilar cholangiocarcinoma. Further investigation in an increased number of cases is needed to identify factors contributory to successful biliary drainage for obstructive jaundice caused by HCC.
As for patient survival duration, the successful drainage group exhibited prolongation of survival time, which was consistent with previous reports. The feasibility of additional treatment for HCC in the successful drainage group might also contribute to the prolongation of survival time. The median duration of stent patency was 42 d; shorter when compared to the duration of stent patency in patients with other malignant bile duct strictures. This could be attributable to the fact that most patients with obstructive jaundice caused by HCC have chronic liver disorders in the background, as well as due to the greater liability of HCC for bleeding. Recent reports have documented placement of self-expandable metallic stents in the treatment of HCC[24-26]; therefore, more effective drainage is anticipated.
Although there have been no reported prospective randomized studies concerning drainage procedures for obstructive jaundice caused by HCC to date, it would be reasonable to establish a first-line drainage method as previously reported. PTBD is an important second-line drainage method for patients in whom EBS is impracticable, as well as in patients who respond poorly to biliary drainage. It is difficult to allude to concrete procedures such as stenting in this paper dealing with a retrospective study, but proactively undertaken biliary drainage afforded prolongation of survival, as reported previously.
Most patients with obstructive jaundice caused by HCC present with a complex disease state (e.g., presence of a chronic liver disorder, greater liability to bleeding, complex factors for bile duct obstruction, and diversity of history of treatment for HCC). Therefore, it is not easy to determine a definite treatment strategy, and a prospective randomized study must be pursued.
In conclusion, proactively undertaken EBS is recommended as a first-line drainage method for the treatment of obstructive jaundice caused by HCC, as it is expected to contribute to prolongation of patient survival. Obstructive jaundice caused by HCC is a complex disease state, so the EBS procedure should be investigated from a viewpoint different from that of biliary drainage performed for other malignant biliary obstructions, such as bile duct carcinoma.
Jaundice appeared in about 40% of patients during the course of hepatocellular carcinoma (HCC); 13% were obstructive jaundice. The state of the cancer progresses greatly, so that drainage is often difficult and the prognosis is usually dismal.
Percutaneous transhepatic biliary drainage (PTBD) was performed for biliary drainage in the treatment for obstructive jaundice caused by HCC, but endoscopic biliary stenting (EBS) has become more common in recent years due to the consideration of quality of life.
MST was 150 d in the successful drainage group and 22 d in the non-successful drainage group; the difference in median survival time between the two groups was statistically significant (P < 0.0001) and, as was the case in previous treatment, statistically significant differences were noted between the two groups in the number of patients without a history of hepatectomy (P = 0.009), as well as the number receiving multiple stents (P = 0.036).
EBS effective cases have been shown to significantly prolong survival. Obstructive jaundice caused by HCC is a complex disease state, so the EBS procedure should be investigated from a viewpoint different from that of biliary drainage performed for other malignant biliary obstructions, such as bile duct carcinoma. Therefore, further studies concerning patient background and a drainage method is expected.
PTBD: A method of performing drainage in patients with obstructive jaundice via ultrasound guided puncturing of the bile duct in the liver. EBS: A method of performing drainage in patients with obstructive jaundice via a duodenoscope and bile duct drainage by duodenal papilla.
The authors’ report the management of a rare HCC associated complication. They present of 36 consecutive patients in their manuscript and clinical outcome; the largest group of patients with said complication in the literature.
P- Reviewers: Juntermanns B, Lalisang TJM S- Editor: Zhai HH L- Editor: Rutherford A E- Editor: Zhang DN
| 1. | Mallory TB, Castleman B, Parris EE. Case records of the Massachusetts General Hospital. N Eng J Med. 1947;237:673-676. |
| 2. | Nomura Y, Kagaya T, Ueda T, Sunagozaka H, Takatori H, Arai K, Kakinoki K, Kawaguchi K, Kitamura K, Yamashita T. The biliary drainage for patients with obstructive jaundice due to hepatocellular carcinoma (article in Japanese). Kanzo. 2012;53:734-740. |
| 3. | Qin LX, Tang ZY. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003;9:385-391. [PubMed] |
| 4. | Barkay O, Mosler P, Schmitt CM, Lehman GA, Frakes JT, Johanson JF, Qaseem T, Howell DA, Sherman S. Effect of endoscopic stenting of malignant bile duct obstruction on quality of life. J Clin Gastroenterol. 2013;47:526-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Ducreux M, Liguory C, Lefebvre JF, Ink O, Choury A, Fritsch J, Bonnel D, Derhy S, Etienne JP. Management of malignant hilar biliary obstruction by endoscopy. Results and prognostic factors. Dig Dis Sci. 1992;37:778-783. [PubMed] |
| 6. | Lau WY, Leung JW, Li AK. Management of hepatocellular carcinoma presenting as obstructive jaundice. Am J Surg. 1990;160:280-282. [PubMed] |
| 7. | Liver Cancer Study Group of Japan. The General Rules for the Clinical and Pathological Study of Primary Liver Cancer (article in Japanese). 5th ed. Tokyo: Kanehara 2009; . |
| 8. | Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31-38. [PubMed] |
| 9. | Lau W, Leung K, Leung TW, Liew CT, Chan MS, Yu SC, Li AK. A logical approach to hepatocellular carcinoma presenting with jaundice. Ann Surg. 1997;225:281-285. [PubMed] |
| 10. | Murata K, Shiraki K, Kawakita T, Yamamoto N, Okano H, Sakai T, Ohmori S, Deguchi M, Shimizu A, Nakano T. Hepatocellular carcinoma presenting with obstructive jaundice: a clinicopathological study of eight cases. Hepatogastroenterology. 2003;50:2057-2060. [PubMed] |
| 11. | Wu CS, Wu SS, Chen PC, Chiu CT, Lin SM, Jan YY, Hung CF. Cholangiography of icteric type hepatoma. Am J Gastroenterol. 1994;89:774-777. [PubMed] |
| 12. | Lai EC, Lau WY. Hepatocellular carcinoma presenting with obstructive jaundice. ANZ J Surg. 2006;76:631-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Lau WY, Leow CK, Leung KL, Leung TW, Chan M, Yu SC. Cholangiographic features in the diagnosis and management of obstructive icteric type hepatocellular carcinoma. HPB Surg. 2000;11:299-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Karnabatidis D, Spiliopoulos S, Katsakiori P, Romanos O, Katsanos K, Siablis D. Percutaneous trans-hepatic bilateral biliary stenting in Bismuth IV malignant obstruction. World J Hepatol. 2013;5:114-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Lau WY, Leung KL, Leung TW, Ho S, Chan M, Liew CK, Leung N, Johnson P, Li AK. Obstructive jaundice secondary to hepatocellular carcinoma. Surg Oncol. 1995;4:303-308. [PubMed] |
| 16. | Lu Z, Sun W, Wen F, Liang H, Shan M, Guo Q. Clinical application of percutaneous drainage in treating hepatocellular carcinoma with bile duct tumor thrombus. Contemp Oncol (Pozn). 2013;17:176-183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Choi J, Ryu JK, Lee SH, Ahn DW, Hwang JH, Kim YT, Yoon YB, Han JK. Biliary drainage for obstructive jaundice caused by unresectable hepatocellular carcinoma: the endoscopic versus percutaneous approach. Hepatobiliary Pancreat Dis Int. 2012;11:636-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Lee JW, Han JK, Kim TK, Choi BI, Park SH, Ko YH, Yoon CJ, Yeon KM. Obstructive jaundice in hepatocellular carcinoma: response after percutaneous transhepatic biliary drainage and prognostic factors. Cardiovasc Intervent Radiol. 2002;25:176-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Minami Y, Kudo M. Hepatocellular carcinoma with obstructive jaundice: endoscopic and percutaneous biliary drainage. Dig Dis. 2012;30:592-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Matsueda K, Yamamoto H, Umeoka F, Ueki T, Matsumura T, Tezen T, Doi I. Effectiveness of endoscopic biliary drainage for unresectable hepatocellular carcinoma associated with obstructive jaundice. J Gastroenterol. 2001;36:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Martin JA, Slivka A, Rabinovitz M, Carr BI, Wilson J, Silverman WB. ERCP and stent therapy for progressive jaundice in hepatocellular carcinoma: which patients benefit, which patients don’t? Dig Dis Sci. 1999;44:1298-1302. [PubMed] |
| 22. | Cho HC, Lee JK, Lee KH, Lee KT, Paik S, Choo SW, Do YS, Choo IW. Are endoscopic or percutaneous biliary drainage effective for obstructive jaundice caused by hepatocellular carcinoma? Eur J Gastroenterol Hepatol. 2011;23:224-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Kanno Y, Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Takasawa O, Kato Y, Koshita S. Single-session endoscopic bilateral y-configured placement of metal stents for hilar malignant biliary obstruction. Dig Endosc. 2011;23:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Speer AG, Cotton PB, Russell RC, Mason RR, Hatfield AR, Leung JW, MacRae KD, Houghton J, Lennon CA. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet. 1987;2:57-62. [PubMed] |
| 25. | Kawaguchi Y, Ogawa M, Maruno A, Ito H, Mine T. A case of successful placement of a fully covered metallic stent for hemobilia secondary to hepatocellular carcinoma with bile duct invasion. Case Rep Oncol. 2012;5:682-686. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Okazaki M, Mizuta A, Hamada N, Kawamura N, Nakao K, Kikuchi T, Osada T. Hepatocellular carcinoma with obstructive jaundice successfully treated with a self-expandable metallic stent. J Gastroenterol. 1998;33:886-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |