Published online Jun 7, 2014. doi: 10.3748/wjg.v20.i21.6685
Revised: March 1, 2014
Accepted: March 12, 2014
Published online: June 7, 2014
Processing time: 190 Days and 2.2 Hours
Schwannomas occurring in the gallbladder are extremely rare. Preoperative diagnosis of gallbladder schwannomas appears to be very difficult because they are normally asymptomatic and are often found incidentally. Until now, only five cases have been reported in the literature. To our knowledge, the contrast-enhanced ultrasound (CEUS) features of gallbladder schwannomas have not been reported before in other studies. We treated a 55-year-old male patient with gallbladder schwannoma in China. He had no symptoms, and the lesion was incidentally found by conventional ultrasound (US) when performing a health examination. The patient had normal liver function; moreover, serum carcinoembryonic antigen and alpha-fetoprotein were within the normal ranges. The lesion showed no blood flow signals on color Doppler US, and the wall beneath the lesion was intact on CEUS. The lesion was believed to be a benign entity; in addition, gallbladder adenomyomatosis was suspected. A laparoscopic cholecystectomy was performed to remove the mass. Pathological examination revealed that the tumor was mainly composed of spindle-shaped cells; neither atypical cells nor signs of malignancy were found. Immunohistochemical staining showed a strong positive S-100 protein reaction. Vimentin and CD56 staining were also positive, whereas CD34 and CD117 were negative. Finally, the lesion was diagnosed as schwannoma. Herein, we report the case; the associated literature is also reviewed.
Core tip: Gallbladder schwannoma, a benign tumor derived from the Schwann’s cells in the gallbladder wall, is extremely rare. This paper describes the case of a 55-year-old man with a mass in the gallbladder but no other symptoms. The patient was treated by cholecystectomy. After 1 year of follow-up with clinical evaluation and ultrasound (US), it did not show any evidence of local recurrence. We learned through this rare case of gallbladder schwannoma that the imaging findings have not been reported in detail before. The US, especially contrast-enhanced ultrasound, features seemed to be helpful in excluding malignancy, and it was essential for treatment planning and the alleviation of patient anxiety in this case.
- Citation: Liu LN, Xu HX, Zheng SG, Sun LP, Guo LH, Wu J. Solitary schwannoma of the gallbladder: A case report and literature review. World J Gastroenterol 2014; 20(21): 6685-6690
- URL: https://www.wjgnet.com/1007-9327/full/v20/i21/6685.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i21.6685
Schwannomas are benign neurogenic tumors that originate from the Schwann’s cells of the peripheral nerves in young to middle-aged patients[1]. Schwannoma can develop in any part of the body, but the most common sites include the head, neck, and flexor surfaces of the extremities[2]. Schwannomas arising in the digestive tract are quite rare, and they occur most commonly in the stomach, followed by the colon and rectum[3,4]. Primary benign schwannoma of the gallbladder is extremely rare. In this paper, we present a case of gallbladder schwannoma, with an emphasis on the imaging and pathological findings. Biliary system schwannomas in the literature are also reviewed.
A 55-year-old male patient was admitted to the hospital because a 2.1-cm mass was incidentally detected in his gallbladder by ultrasound (US) during a health examination. The patient had neither complaints nor symptoms. According to the physical examination, his abdomen was soft and flat; there was no evidence of jaundice or abdominal tenderness. He had no previous history of any other major illness, and his vital signs were stable. The blood laboratory study results were as follows: leukocyte count, 6.86 × 109/L; hemoglobin, 159 g/L; total protein, 80 g/L, total albumin, 50 g/L; total bilirubin, 13.4 μmol/L; direct bilirubin, 10.8 μmol/L; serum alanine aminotransferase 16.1 U/L; serum alkaline phosphatase, 53.4 U/L; and serum gamma-glutamyltranspeptidase, 31.4 U/L. The laboratory studies revealed almost normal liver function. Carcinoembryonic antigen and alpha-fetoprotein were within the normal ranges.
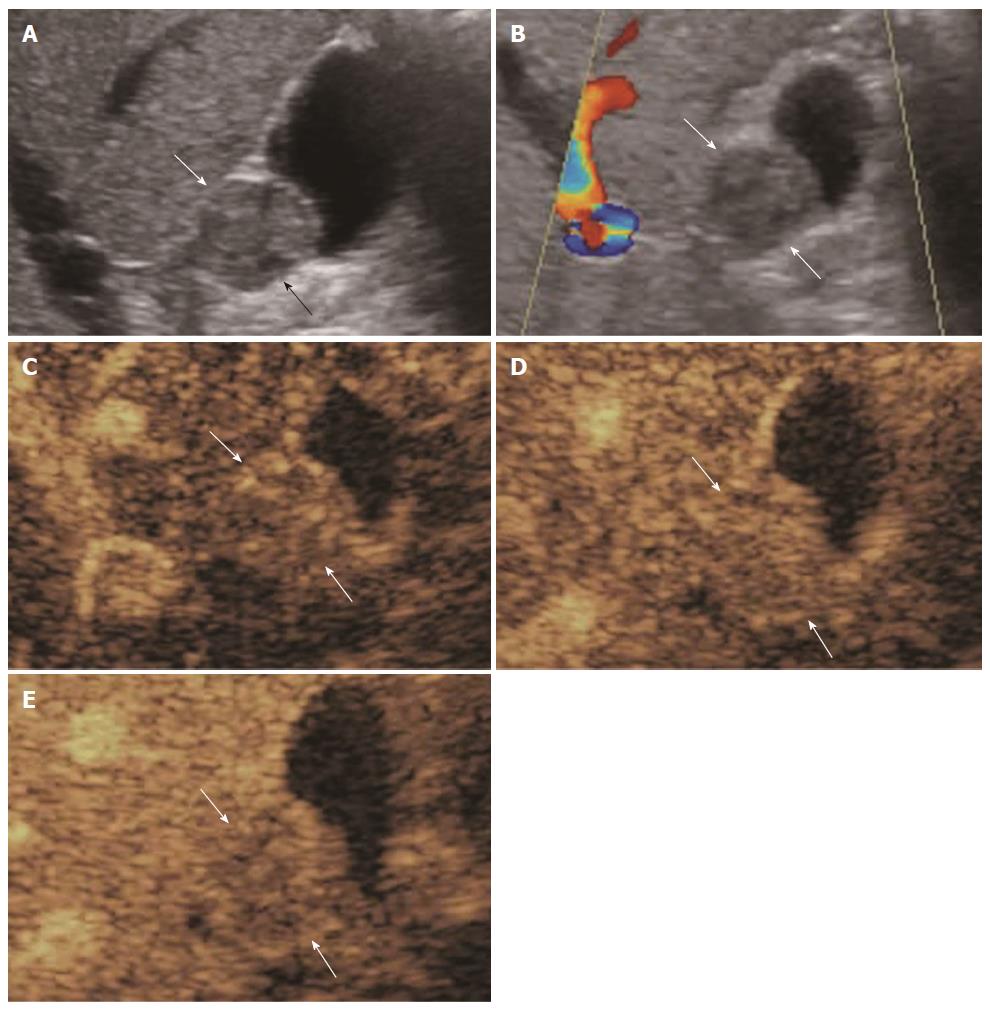
US was performed using a LogiQ E9 scanner (GE Healthcare, Milwaukee, WI, United States) with a convex transducer (frequency range, 2-6 MHz). Conventional US showed a 2.1-cm iso-echoic mural mass in the gallbladder. The mass was solid, homogeneously echogenic, and well defined with no infiltration into the liver (Figure 1A). Color Doppler US showed no flow signals within the mass (Figure 1B). Contrast-enhanced ultrasound (CEUS) was then performed using the low acoustic power contrast-specific imaging mode. The contrast agent used was SonoVue (BR1; Bracco SpA, Milan, Italy), a sulfur hexafluoride-filled microbubble contrast agent. The contrast agent was injected into the antecubital vein as a bolus (within 1-2 s) at a dose of 1.5 mL, followed by a flush of 5 mL of normal saline. The mass appeared slightly hyper-enhanced in the arterial phase and slightly hypo-enhanced in the venous phase. The gallbladder wall under the mass was intact (Figure 1C, 1D and 1E). A diagnosis of gallbladder adenomyomatosis was suspected before surgery.
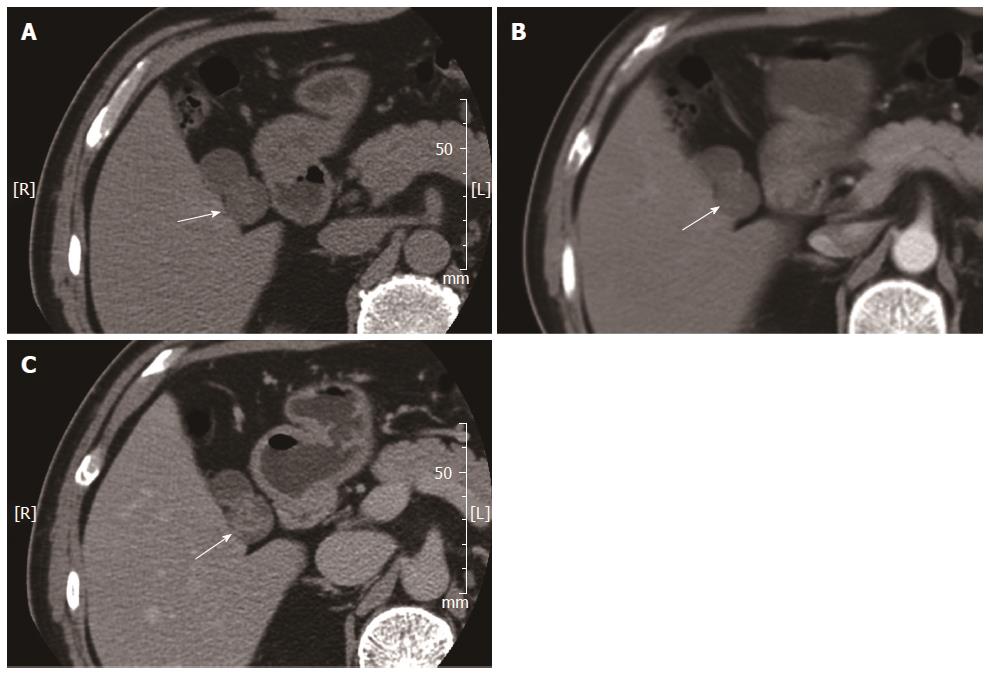
Contrast-enhanced computed tomography (CECT) was subsequently performed to examine the gallbladder within 1 wk after the US examination, using a 64-slice computed tomography (CT) scanner. An un-enhanced CT scan of the gallbladder region showed a well-defined round mass in the gallbladder. The mass showed homogeneous hypo-attenuation without internal calcification or liquefaction (Figure 2A). On CECT, the mass showed slight enhancement in the arterial phase (Figure 2B) and delayed enhancement until the late venous phase (Figure 2C). A CT diagnosis of a gallbladder polyp was suspected before surgery.
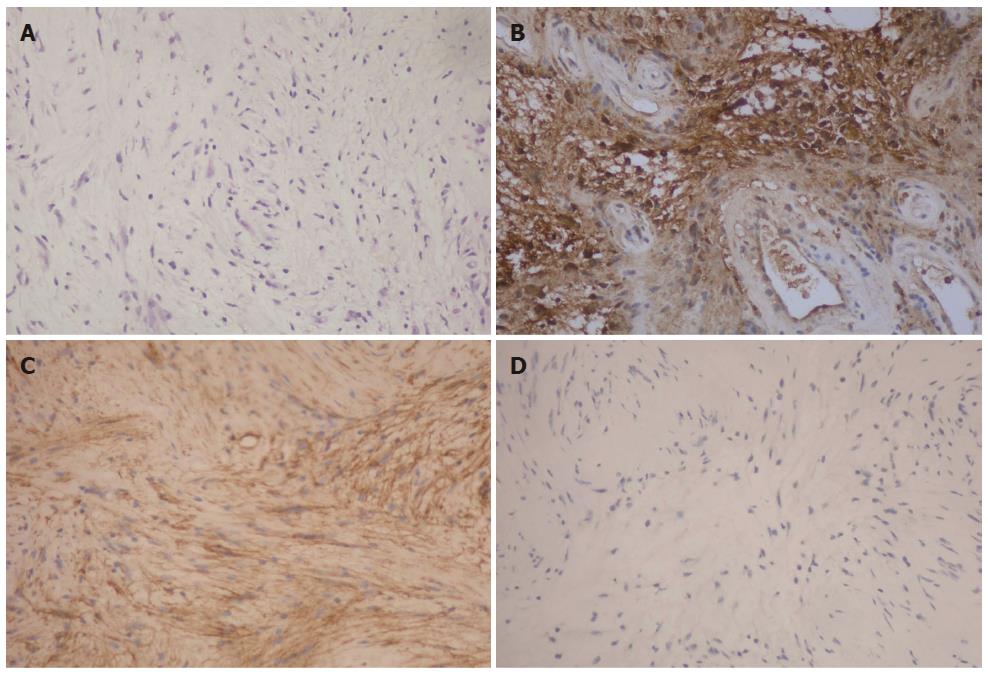
A laparoscopic cholecystectomy was performed to remove the mass. The gross specimen showed a 2.5-cm-sized, well-circumscribed, localized mass, which was surrounded by a fibrous capsule. Microscopic examination revealed that the tumor mainly consisted of spindle-shaped cells; neither atypical cells nor signs of malignancy were found (Figure 3A). Immunohistochemical staining showed a strong positive S-100 protein reaction (Figure 3B). Vimentin and CD56 staining were also positive (Figure 3C), whereas CD34 and CD117 were negative (Figure 3D). The final diagnosis of gallbladder schwannoma was made. Until now, twelve months after operation, the patient remained alive and in good status, without signs of recurrence of the lesion.
Schwannoma is a benign tumor derived from the Schwann’s cells that encapsulates the nerve sheath, so it is known as a neurilemoma. Malignant schwannomas are extremely rare and are always associated with von Recklinghausen’s disease[5,6]. Schwannoma usually occurs in the extremities, but it can also found in head, neck, trunk, retroperitoneum or mediastinum[5]. It can also develop in the gallbladder due to the abundant anastomotic network of sympathetic and parasympathetic nerve fibers in the wall of the gallbladder and bile duct[7]. However, schwannomas arising in gallbladder are extremely rare.
As a result of lacking of adequate knowledge of this tumor and low incidence in clinical practice, correct preoperative diagnosis is hard to achieve. When tumor was small, patient normally appeared asymptomatic; on the contrary, jaundice and vague pain may happened when tumor was too large to compress surrounding organs. Until now, only five similar cases have been reported (Table 1). In the reported cases of gallbladder schwannomas, two cases revealed obstructive jaundice and vague pain; the other three cases were asymptomatic.
| Ref. | Year | Sex | Age | Symptom | Imagingmethod | Location | Size(mm) | Preoperative diagnosis | With GB stones | Treatment | Follow-up | Status |
| Yamagiwa et al[18] | 1991 | M | 58 | Jaundice | NA | Neck | 4 | Bile duct cancer | NA | Cholecystectomy | NA | NA |
| Matsuoka et al[19] | 1996 | M | 74 | Asymptomatic | US MRI CT and endoscopy | Fundus | 10 | Adenomyomatosis | N | Cholecystectomy + hepatectomy | NA | NA |
| Ren et al[20] | 2001 | F | 26 | Vague pain | US and CECT | Neck | 110 | Tumor of GB | N | Cholecystectomy | NA | NA |
| Colović et al[21] | 2003 | F | 61 | NA | NA | Whole | 90 | Tumor of GB | N | Cholecystectomy | 10 Y | Survived |
| Ohta et al[5] | 2008 | M | 58 | Asymptomatic | CT and US | Fundus | 3 | Cholecystolithiasis | Y | Cholecystectomy | 16 M | Survived |
| Current case | 2012 | M | 55 | Asymptomatic | CEUS and CECT | Neck | 22 | Adenomyomatosis | N | Cholecystectomy | 12 M | Survived |
Imaging modalities, such as CT, magnetic resonance imaging (MRI), and US, are useful for detecting and locating tumors; however, definitive diagnosis is rarely achievable. Some cases might even be not visible on imaging examinations when the lesions coexist with cholecystolithiasis or are overly small[5]. Generally speaking, an unenhanced CT scan depicts a schwannoma as a well-defined hypoattenuating area, and CECT shows peripheral enhancement with an irregular pattern. Delayed peripheral enhancement until the late venous phase on the CT scan reflects a fibrous capsule and an internal fibrillary element[1,8]. In our case, however, no obvious enhancement during the arterial phase was observed on CECT. On MRI, schwannomas present as masses of low signal intensity on T1-weighted images and of high signal intensity on T2-weighted images[2,9].
The US features of this lesion are unknown and non-specific. Ohta et al[5] reported a lesion appearing on US as local gallbladder wall thickening at the fundus of the gallbladder with cholecystolithiasis. The lesion was diagnosed as chronic cholecystitis before surgery. In the present case, the lesion was visualized as a well-defined round isoechoic mass originating from the gallbladder wall on gray-scale US, and no intra-lesional blood flow signals were visible on color Doppler US. Although the lesion was larger than 2 cm in diameter, the wall beneath the mass was intact. No infiltration into the adjacent liver was present. CEUS with SonoVue was used for the preoperative diagnosis, which has not been reported before. The contrast arrival time to the lesion was 19 s after administration of the contrast agent. The lesion showed hyper-enhancement in the arterial phase of CEUS and began to be hypo-enhanced 54 s after contrast administration. The gallbladder wall under the mass was intact in all of the phases. According to the previous literature regarding gallbladder CEUS[10-12], malignant gallbladder lesions usually fade more quickly than benign gallbladder lesions, and most malignant gallbladder lesions begin to be hypo-enhanced 50 s before contrast administration. In addition, the gallbladder wall beneath the malignant lesion is usually destroyed, whereas it remains intact with benign gallbladder lesions.
Immunohistochemical analysis is necessary to distinguish schwannomas from neurofibromas, gastrointestinal stromal tumors and leiomyomas[13]. Schwannomas are strongly positive for vimentin and S100 protein while negative for muscle cell markers; CD117 and CD34 are also useful clues for schwannoma, whereas positive staining has been helpful for the immunohistochemical diagnosis of gastrointestinal stromal tumors[5,14].
Histologically, schwannomas originating in the digestive tract are S-100 protein-positive spindle cell tumors that consist mainly of cellular (Antoni A) areas, and they generally do not show a nuclear palisading pattern, which is usually found in conventional schwannomas of the soft tissue and central nervous system[2,15,16]. Whether lack neurofibromatosis-2 genetic alterations might be the key point to distinct schwannomas of the digestive tract from conventional schwannomas[2,17].
Schwannomas of the gallbladder can be successfully treated surgically, like schwannomas in other locations[1]. The treatment of choice is cholecystectomy due to the diagnostic uncertainty before surgery, even with extensive application of various imaging modalities. To our knowledge, this was the first time to evaluate the features and usefulness of CEUS in diagnosing solitary schwannoma of the gallbladder. CEUS can easily excluding the possibility of malignant GB disease.
The authors thank Hao Xi for proofreading the pathologic materials.
A rare case of gallbladder schwannoma was incidentally detected in a 55-year-old man by ultrasound (US) during a health examination.
The patient had no symptoms, such as obstructive jaundice or pain.
Gallbladder polyp; gallbladder adenomyomatosis; gallbladder cancer.
Leukocyte count, 6.86 × 109/L; hemoglobin, 159 g/L; total protein, 80 g/L, total albumin, 50 g/L; total bilirubin, 13.4 μmol/L; direct bilirubin, 10.8 μmol/L; serum alanine aminotransferase 16.1 U/L; serum alkaline phosphatase, 53. 4U/L; serum gamma-glutamyltranspeptidase, 31.4 U/L; carcinoembryonic antigen, alpha-fetoprotein and liver function tests were within the normal limits.
US showed a 2.1-cm, iso-echoic, well-defined, mural mass in the gallbladder; contrast-enhanced ultrasound (CEUS) showed the mass slightly was hyper-enhanced in the arterial phase and slightly hypo-enhanced in the venous phase; moreover, the gallbladder wall under the mass was intact.
Microscopic examination revealed that the tumor mainly consisted of spindle-shaped cells; it was S-100/Vimentin/CD56-positive and CD34/CD117-negative.
The patient was treated with cholecystectomy.
Schwannomas arising in the gallbladder are extremely rare, and preoperative diagnosis appears to be very difficult because these tumors are commonly asymptomatic and are often discovered incidentally.
To our knowledge, the CEUS features of gallbladder schwannomas have not been reported before in the other literature.
This report not only presents the details of the US and CEUS features in this case, but it also indicates the usefulness of CEUS in excluding malignancy before surgery.
This article presents a case of gallbladder schwannoma with an emphasis on the imaging and pathological findings; also, biliary system schwannomas in the literature are reviewed.
P- Reviewer: Cai Q S- Editor: Wen LL L- Editor: A E- Editor: Wang CH
| 1. | Ota Y, Aso K, Watanabe K, Einama T, Imai K, Karasaki H, Sudo R, Tamaki Y, Okada M, Tokusashi Y. Hepatic schwannoma: imaging findings on CT, MRI and contrast-enhanced ultrasonography. World J Gastroenterol. 2012;18:4967-4972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 2. | Jung JH, Joo KR, Chae MJ, Jang JY, Lee SG, Dong SH, Kim HJ, Kim BH, Chang YW, Lee JI. Extrahepatic biliary schwannomas: a case report. J Korean Med Sci. 2007;22:549-552. [PubMed] |
| 3. | Miettinen M, Shekitka KM, Sobin LH. Schwannomas in the colon and rectum: a clinicopathologic and immunohistochemical study of 20 cases. Am J Surg Pathol. 2001;25:846-855. [PubMed] |
| 4. | Sarlomo-Rikala M, Miettinen M. Gastric schwannoma--a clinicopathological analysis of six cases. Histopathology. 1995;27:355-360. [PubMed] |
| 5. | Ohta R, Hirata Y, Oneyama M, Takahashi Y, Kawahara Y, Kitamura M, Goto M, Sekikawa K, Takenoshita S. Schwannoma of the gallbladder: report of a case. Fukushima J Med Sci. 2010;56:38-43. [PubMed] |
| 6. | Coombs RJ. Case of the season. Malignant neurogenic tumor of duodenum and pancreas. Semin Roentgenol. 1990;25:127-129. [PubMed] |
| 7. | Northover JM, Terblanche J. A new look at the arterial supply of the bile duct in man and its surgical implications. Br J Surg. 1979;66:379-384. [PubMed] |
| 8. | Wada Y, Jimi A, Nakashima O, Kojiro M, Kurohiji T, Sai K. Schwannoma of the liver: report of two surgical cases. Pathol Int. 1998;48:611-617. [PubMed] |
| 9. | Rha SE, Byun JY, Jung SE, Chun HJ, Lee HG, Lee JM. Neurogenic tumors in the abdomen: tumor types and imaging characteristics. Radiographics. 2003;23:29-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 264] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 10. | Zheng SG, Xu HX, Liu LN, Lu MD, Xie XY, Wang WP, Hu B, Yan K, Ding H, Tang SS. Contrast-enhanced ultrasound versus conventional ultrasound in the diagnosis of polypoid lesion of gallbladder: a multi-center study of dynamic microvascularization. Clin Hemorheol Microcirc. 2013;55:359-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Liu LN, Xu HX, Lu MD, Xie XY, Wang WP, Hu B, Yan K, Ding H, Tang SS, Qian LX. Contrast-enhanced ultrasound in the diagnosis of gallbladder diseases: a multi-center experience. PLoS One. 2012;7:e48371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Xie XH, Xu HX, Xie XY, Lu MD, Kuang M, Xu ZF, Liu GJ, Wang Z, Liang JY, Chen LD. Differential diagnosis between benign and malignant gallbladder diseases with real-time contrast-enhanced ultrasound. Eur Radiol. 2010;20:239-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 96] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Fonseca GM, Montagnini AL, Rocha Mde S, Patzina RA, Bernardes MV, Cecconello I, Jukemura J. Biliary tract schwannoma: a rare cause of obstructive jaundice in a young patient. World J Gastroenterol. 2012;18:5305-5308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 14. | Parameshwarappa S, Rodrigues G, Kumar S, Patil B, Valliathan M. Schwannoma of common bile duct causing obstructive jaundice. Indian J Surg. 2010;72:333-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Daimaru Y, Kido H, Hashimoto H, Enjoji M. Benign schwannoma of the gastrointestinal tract: a clinicopathologic and immunohistochemical study. Hum Pathol. 1988;19:257-264. [PubMed] |
| 16. | Honjo Y, Kobayashi Y, Nakamura T, Takehira Y, Kitagawa M, Ikematsu Y, Ozawa T, Nakamura H. Extrahepatic biliary schwannoma. Dig Dis Sci. 2003;48:2221-2226. [PubMed] |
| 17. | Lasota J, Wasag B, Dansonka-Mieszkowska A, Karcz D, Millward CL, Ryś J, Stachura J, Sobin LH, Miettinen M. Evaluation of NF2 and NF1 tumor suppressor genes in distinctive gastrointestinal nerve sheath tumors traditionally diagnosed as benign schwannomas: s study of 20 cases. Lab Invest. 2003;83:1361-1371. [PubMed] |
| 18. | Yamagiwa HKK, Kurata M, Suzaki M, Sakai H, Kitagawa M, Itoh H. A case of schwannoma of gallbladder (in Japanese). Med J Mie Univ. 1991;35:4. |
| 19. | Matsuoka J, Tanaka N, Kojima K, Takai K, Hamaya K, Gochi A, Kamikawa Y, Orita K. A case of traumatic neuroma of the gallbladder in the absence of previous surgery and cholelithiasis. Acta Med Okayama. 1996;50:273-277. [PubMed] |
| 20. | Ren JJ, Li TP, Wu JL, Hao B. Schwannoma of the gallbladder: A case report (in Chinese). Zhonghua Waihe Zazhi. 2001;39:673. |
| 21. | Colović R, Grubor N, Jancić-Zguricas M, Zogović S. Schwannoma of the gallbladder. Acta Chir Iugosl. 2003;50:135-137. [PubMed] |