Published online May 28, 2014. doi: 10.3748/wjg.v20.i20.6353
Revised: February 9, 2014
Accepted: March 5, 2014
Published online: May 28, 2014
Processing time: 147 Days and 0.6 Hours
Synchronous gastric cancer and primary small intestinal lymphoma are extremely rare. A 49-year-old woman was referred to our hospital with a history of upper abdominal pain for two weeks and was diagnosed with synchronous cancer. During hospitalization, the patient underwent laparoscopic distal gastrectomy + resection of bilateral ovaries + partial resection of both small intestine and descending colon. Pathological examination revealed a synchronous cancer consisting of early gastric cancer with poorly differentiated adenocarcinoma located in mucosa, with lymph node metastasis (3+/29) (T1N1M0, stage IB); and diffuse large B cell lymphoma of small intestine involving descending colon and bilateral ovaries, with lymph node metastasis (2+/5) (Ann Arbor IIE). The patient recovered well, without any obvious complications and was discharged on post-operative day 7. The patient received six cycles of chemotherapy after operation. She has been doing well with no evidence of recurrence for 13 mo.
Core tip: Synchronous gastric cancer and primary small intestinal lymphoma are extremely rare. Only one such case has been reported in English literature. We here report a case of a 49-year-old woman with synchronous gastric cancer and primary small intestinal lymphoma, who was successfully treated by combined laparoscopic resection and adjuvant chemotherapy.
- Citation: Chen DW, Pan Y, Yan JF, Mou YP. Laparoscopic resection of synchronous gastric cancer and primary small intestinal lymphoma: A case report. World J Gastroenterol 2014; 20(20): 6353-6356
- URL: https://www.wjgnet.com/1007-9327/full/v20/i20/6353.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i20.6353
Gastric cancer is one of the most common gastrointestinal tract carcinomas, and it is the fourth most common cancer and the second most common cause of cancer-related death worldwide. Primary small intestinal lymphoma is relatively rare. Only one case of the synchronous gastric cancer and primary small intestinal lymphoma has been reported in English literature[1]. We herein report a case of a 49-year-old woman with synchronous gastric cancer and primary small intestinal lymphoma, who was successfully treated by combined laparoscopic resection and adjuvant chemotherapy.
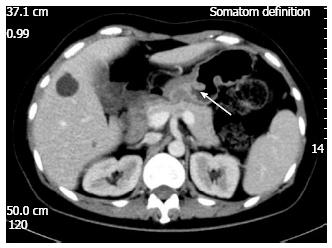
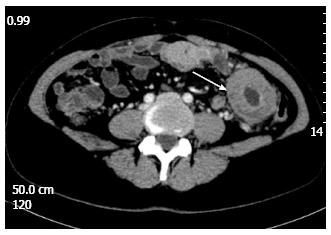
A 49-year-old woman was referred to our hospital on November 1, 2012 due to upper abdominal pain for two weeks. On admission, she was chronically ill-looking and alert. Her blood pressure was 120/70 mmHg, pulse 70/min, respiration 20/min, and body temperature 36.8 °C. Lungs were clear to auscultation and heart examination was normal, without murmur or rubs. Liver and spleen were non-palpable. Slight tenderness on the upper middle abdomen was noted. Laboratory test results showed WBC 6.4 × 103/uL, hemoglobin 7.4 g/dL, glucose 4.29 mmol/L, TP 65 g/L, ALB 39.8 g/L; CA19-9 6.66 IU/mL (normal range:0-37 IU/mL), and CEA 1.14 ng/mL (normal range:0-5 ng/mL). Fecal occult blood test was positive (2+). Gastroscopy showed the rough mucosa of gastric antrum, the pathological diagnosis was adenocarcinoma of gastric antrum. Computed tomography (CT) and magnetic resonance imaging revealed thickened gastric antrum wall (Figure 1); thickened small intestinal wall in the left mid-abdomen, with peripheral lymph nodes enlargement (Figure 2); and cystic lesions of bilateral ovaries. The positron emission tomography (PET) CT showed thickened gastric antrum wall and thickened small intestinal wall in the left mid-abdomen with peripheral lymph nodes enlargement, along with slight elevation of 18F-fluorodeoxyglucose. She had no remarkable family history.
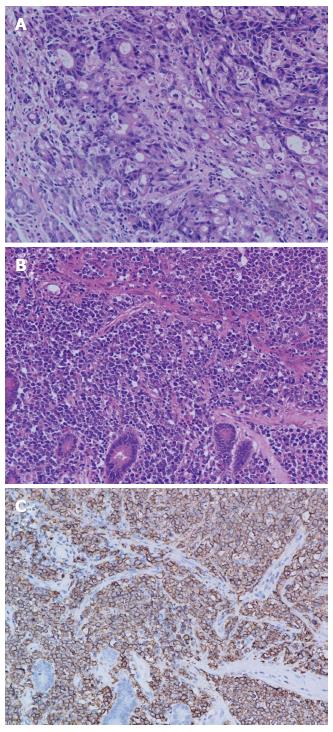
During hospitalization, the patient underwent laparoscopic distal gastrectomy + resection of bilateral ovaries + partial resection of both small intestine and descending colon. Perioperation found a 3 cm × 3 cm ulcerofungating mass in the gastric antrum on the lesser curvature, not extending to the serosa layer; obvious thickening of small intestinal wall of about 13 cm in length, 40 cm distant to ligament of Treitz, which invaded the descending colon; and cystic masses in bilateral ovaries (Figures 3 and 4). Pathological examinations (Figure 5) revealed an early gastric cancer with poorly differentiated adenocarcinoma located in mucosa, with lymph nodes metastasis (3+/29); and a diffuse large B cell lymphoma of small intestine involving the descending colon and bilateral ovaries, being positive for CD20, CD10, Bcl-6 and Bcl-2, and 80% positive for Ki67, negative for CK, CD3, CD5 and Cyclind-1and MUM-1, with lymph nodes metastasis (2+/5). The patient recovered well, without any obvious complications, and was discharged on post-operative day 7. The patient received six cycles of chemotherapy after operation. Each cycle of the chemotherapy regimen including: Rituximab 600 mg ivgtt d1 + oxaliplatin 130 mg ivgtt d1 + epirubicin 90 mg ivgtt d1 + vincristine 2 mg ivgtt d1 + dexamethasone 15 mg iv d1-3. She has been doing well with no evidence of recurrence for 13 mo.
Gastric cancer is one of the most common malignant tumors. Despite steady declines in the incidence and mortality, gastric cancer remains the fourth most common malignancy diagnosed in developed countries in both men and women[2]. However, primary gastrointestinal lymphoma is very rare, accounting for only about 1%-8% of all gastrointestinal malignancies[3]. Meanwhile, primary small intestinal lymphoma constitutes 20%-30% of all primary gastrointestinal lymphomas[4]. The incidence of gastric cancer with a synchronous second primary cancer varies from 0.7% to 3.5%[5]. However, gastric cancer occurring simultaneously with a primary small intestinal lymphoma is extremely rare.
For the present case, in view of the gastric cancer and thickness of small intestinal wall located in the left mid-abdomen with peripheral lymph node enlargement shown by imaging studies, we initially diagnosed it as gastric cancer with abdominal metastasis. We also considered the possibility of synchronous gastric cancer with primary small intestinal lymphoma. The sustained positive occult blood test in this patient suggested active gastrointestinal tract bleeding. We then chose to perform the laparoscopic exploration, and finally decided to perform laparoscopic distal gastrectomy + resection of bilateral ovaries + resection of partial small intestine and partial descending colon. After surgery, the patient was diagnosed with a synchronous cancer based on the pathological results, and received regular chemotherapy subsequently. Therefore, once it is determined that a patient has a localized and potentially curable lesion, a multidisciplinary evaluation and multimodality therapy are recommended[6]. In a review of some retrospective studies, it has been reported that surgery combined with postoperative chemotherapy is superior to the chemotherapy or radiotherapy used alone for such patient[7-9].
To diagnose a synchronous cancer, three criteria should be satisfied. First, cancer lesions should be located apart from each other, and should not be contiguous. Second, they must be pathologically different. Third, mucosal invasion should occur in both lesions[10]. In our case, the postoperative pathologic findings showed that the two lesions were located separately. It implies that the cancer originates from two lesions: one from the gastric antrum and the other from the small intestine. Moreover, the pathological diagnosis of the two lesions is obviously different from each other.
Through prudent diagnosis and treatment plan, complete resection of the tumor burden and combination of chemotherapy will lead to improvement in patient survival.
In conclusion, our case highlights a rare occurrence of synchronous double malignancies consisting of a gastric cancer and a primary small intestinal lymphoma.
A 49-year-old woman with upper abdominal pain for two weeks.
Synchronous gastric cancer and primary small intestinal lymphoma.
Gastric cancer with abdominal metastasis.
Laboratory test results: WBC 6.4 × 103/uL, hemoglobin 7.4 g/dL, CA19-9 6.66 IU/mL, and CEA 1.14 ng/mL. Fecal occult blood test: positive (2+).
Computed tomography and magnetic resonance imaging showed: thickened gastric antrum wall; thickened small intestinal wall in the left mid-abdomen, with peripheral lymph node enlargement; and cystic lesions of bilateral ovaries.
Early gastric cancer with poorly differentiated adenocarcinoma located in mucosa, with lymph node metastasis (3+/29); diffuse large B cell lymphoma of small intestine involving the descending colon and bilateral ovaries, with lymph node metastasis (2+/5).
Laparoscopic distal gastrectomy + resection of bilateral ovaries + partial resection of both small intestine and descending colon, followed by six cycles of chemotherapy after operation.
The gastric cancer occurring simultaneously with primary small intestinal lymphoma is extremely rare. Only one such case has been reported in English literature.
Their case highlights a rare occurrence of synchronous double malignancies consisting of a gastric cancer and a primary small intestinal lymphoma. Through prudent diagnosis and treatment plan, complete resection of the tumor burden and combination of chemotherapy will lead to improvement in patient survival.
This article highlights a rare occurrence of synchronous double malignancies consisting of a gastric cancer and a primary small intestinal lymphoma.
P- Reviewers: AL-Asari S, Marks JM, O'Dwyer PJ, Tran TT S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Carson HJ. Unexpected synchronous non-Hodgkin’s lymphoma encountered during the treatment of a previously-diagnosed carcinoma: report of three cases. Leuk Lymphoma. 1996;23:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Blakely AM, Miner TJ. Surgical considerations in the treatment of gastric cancer. Gastroenterol Clin North Am. 2013;42:337-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Nakamura S, Matsumoto T. Gastrointestinal lymphoma: recent advances in diagnosis and treatment. Digestion. 2013;87:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Bandyopadhyay R, Sinha SK, Chatterjee U, Nag D, Mukhopadhyay S, Chowdhury SR, Biswas PK. Primary pediatric gastrointestinal lymphoma. Indian J Med Paediatr Oncol. 2011;32:92-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Lee JH, Bae JS, Ryu KW, Lee JS, Park SR, Kim CG, Kook MC, Choi IJ, Kim YW, Park JG. Gastric cancer patients at high-risk of having synchronous cancer. World J Gastroenterol. 2006;12:2588-2592. [PubMed] |
| 6. | Taketa T, Sudo K, Wadhawa R, Blum MM, Ajani JA. Adjuvant therapy in gastric cancer: what is the optimal approach? Curr Oncol Rep. 2013;15:146-151. [PubMed] |
| 7. | Wang GB, Xu GL, Luo GY, Shan HB, Li Y, Gao XY, Li JJ, Zhang R. Primary intestinal non-Hodgkin’s lymphoma: a clinicopathologic analysis of 81 patients. World J Gastroenterol. 2011;17:4625-4631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Ibrahim EM, Ezzat AA, El-Weshi AN, Martin JM, Khafaga YM, Al Rabih W, Ajarim DS, Al-Foudeh MO, Zucca E. Primary intestinal diffuse large B-cell non-Hodgkin’s lymphoma: clinical features, management, and prognosis of 66 patients. Ann Oncol. 2001;12:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Kim SJ, Kang HJ, Kim JS, Oh SY, Choi CW, Lee SI, Won JH, Kim MK, Kwon JH, Mun YC. Comparison of treatment strategies for patients with intestinal diffuse large B-cell lymphoma: surgical resection followed by chemotherapy versus chemotherapy alone. Blood. 2011;117:1958-1965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Lim SM, Jung ES, Shin SK, Chung HS, Kim HI, Kim do W, Cho BC. A case of synchronous squamous cell carcinoma in the esophagus and stomach. Gut Liver. 2012;6:118-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |