Published online May 21, 2014. doi: 10.3748/wjg.v20.i19.5808
Revised: February 19, 2014
Accepted: March 19, 2014
Published online: May 21, 2014
Processing time: 190 Days and 17.6 Hours
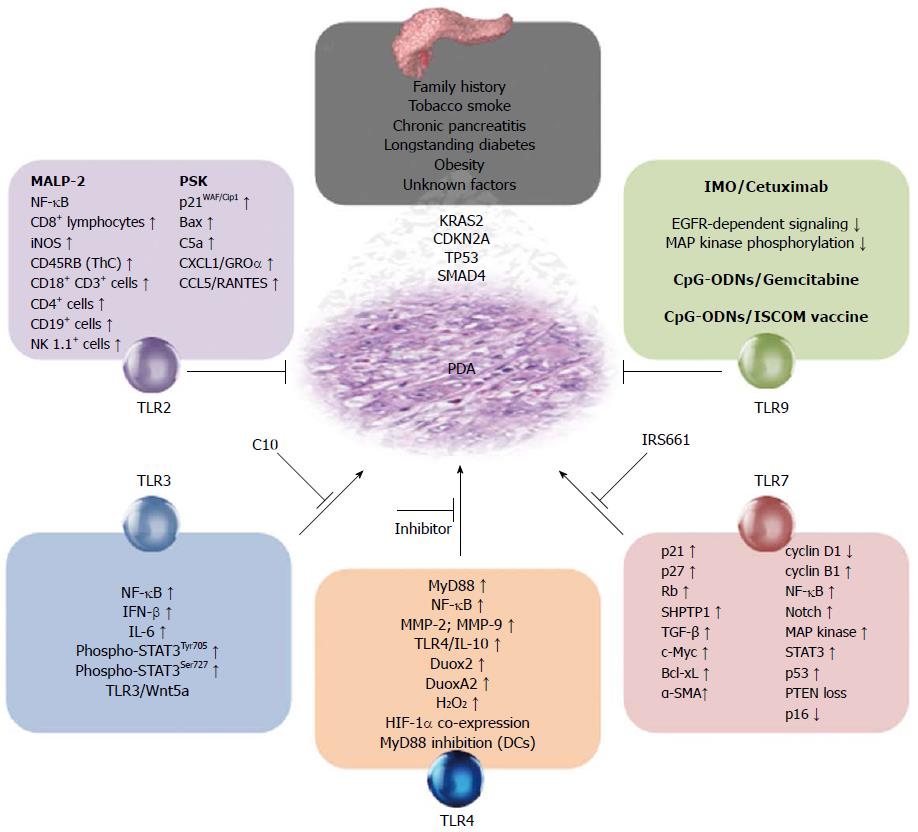
Pancreatic ductal adenocarcinoma (PDA) is a devastating disease with pronounced morbidity and a high mortality rate. Currently available treatments lack convincing cost-efficiency determinations and are in most cases not associated with relevant success rate. Experimental stimulation of the immune system in murine PDA models has revealed some promising results. Toll-like receptors (TLRs) are pillars of the immune system that have been linked to several forms of malignancy, including lung, breast and colon cancer. In humans, TLRs are expressed in the pancreatic cancer tissue and in several cancer cell lines, whereas they are not expressed in the normal pancreas. In the present review, we explore the current knowledge concerning the role of different TLRs associated to PDA. Even if almost all known TLRs are expressed in the pancreatic cancer microenvironment, there are only five TLRs suggested as possible therapeutic targets. Most data points at TLR2 and TLR9 as effective tumor markers and agonists could potentially be used as e.g. future adjuvant therapies. The elucidation of the role of TLR3 in PDA is only in its initial phase. The inhibition/blockage of TLR4-related pathways has shown some promising effects, but there are still many steps left before TLR4 inhibitors can be considered as possible therapeutic agents. Finally, TLR7 antagonists seem to be potential candidates for therapy. Independent of their potential in immunotherapies, all existing data indicate that TLRs are strongly involved in the pathophysiology and development of PDA.
Core tip: The combination of high mortality rates and a tremendously complex pathophysiology makes pancreatic ductal adenocarcinoma (PDA) an enormous challenge. We summarize the current knowledge about the importance of toll-like receptors (TLR) in PDA. Since both tumor and tumor-related cells express TLRs, intervention on TLR-related pathways may represent future candidates for therapy.
- Citation: Vaz J, Andersson R. Intervention on toll-like receptors in pancreatic cancer. World J Gastroenterol 2014; 20(19): 5808-5817
- URL: https://www.wjgnet.com/1007-9327/full/v20/i19/5808.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i19.5808
Disorders of the pancreas are leading causes of morbidity and mortality. Despite advanced surgical and/or oncological treatment strategies, pancreatic ductal adenocarcinoma (PDA) is still associated with an extremely poor prognosis with a median survival of 6 mo and a 5-year survival rate less than 1%-2%[1,2]. PDA represents the fourth cause of cancer-related deaths and its incidence is rising in most countries[3].
The causes of PDA are mainly unknown. A family history is found in up to 5%-10% of patients[4]. Known risk factors for PDA are among others tobacco smoking, diabetes mellitus, obesity and chronic pancreatitis[5-7]. Pancreatic intraepithelial neoplasia (PanIN) in the ductal epithelium has been suggested as the primordial precursor of PDA[8]. As PanIN progress to carcinoma, accumulated mutations might result in the activation of the KRAS2 oncogene, loss of CDKN2A/p16 and/or the inactivation of TP53 and SMAD4[9]. Likewise, stellate cells are major players in PDA, as they are fundamental for the development of the characteristic desmoplastic stroma found in PDA[10]. Pancreatic cancer stem cells might be important in treatment resistance and metastasis. A large range of cell populations, such as tumor-associated macrophages (TAMs), have been reported as central in PDA[11,12]. The current knowledge of the pathophysiology of PDA has elegantly been summarized by Hidalgo[13,14].
At the time of diagnosis, most patients have already developed locally advanced (stages II or III) or metastatic (stage IV) disease and palliative treatment is the only alternative. Gemcitabine is a nucleoside analogue with a broad-spectrum against solid tumors that for long has been used as first-line treatment. In PDA, gemcitabine increases the quality of life of many patients, but merely prolongs the mean survival by one month[15]. Furthermore, a majority of patients do not respond to gemcitabine due to lack of the necessary nucleoside transporter, and the total costs and side-effects related to gemcitabine overtreatment are high[16,17]. FOLFIRINOX (5FU/leucovorin, irinotecan and oxaliplatin) is currently a first-line treatment for metastatic PDA as the regime is more active than gemcitabine at overall survival, progression-free survival and response rate. Moreover, the degradation of the quality of life is also delayed by FOLFIRINOX[18]. However, the regime is more expensive than gemcitabine and not suitable for all patients due to its toxicity. Hence, in most developing countries, gemcitabine is still the gold standard. Thus, current chemotherapeutic strategies lack proper cost-efficiency determinations and are not effective in the vast majority of cases.
In order to increase survival rates in PDA, it is imperative to find novel therapies that specifically target tumor cells and/or associated cell populations and stroma. Toll-like receptors (TLRs) are pillars of the immune system that have been linked to major cancer forms, including lung, breast and colon cancer[19-21]. In humans, TLRs are expressed in the pancreatic cancer tissue and in several cancer cell lines, whereas they are not expressed in the normal pancreas[22,23] (Table 1). TLRs thus appear to play a role in the pathophysiology of PDA (Table 2, Figure 1) and may thereby also represent targets for intervention (Table 3). In the present review, we explore the current knowledge concerning the role of different TLRs associated to PDA.
| Cell line | Source | Phenotype | Expressed TLR | Ref. |
| AsPC-1 | Metastasis: ascites | Du | TLR3, TLR4, TLR9 | [23,57,58] |
| BxPC-3 | Primary tumor | Du | TLR2-4 | [40,50,57] |
| CFPAC | Metastasis: liver | Du | TLR4 | [57] |
| Colo357 | Metastasis: lymph node | Un | TLR3, TLR7 | [48] |
| GER | Primary tumor | An | TLR9 | [72] |
| MIA PaCa-2 | Primary tumor | An | TLR2-4, TLR7, TLR9 | [23,40] |
| MDAPanc-28 | Primary tumor | Du/Ac | TLR2-4, TLR7, TLR9 | [23] |
| Panc-1 | Primary tumor | Du/An | TLR2-4, TLR7, TLR9 | [23,40,50,58,79] |
| Panc-89 | Metastasis: lymph node | Du | TLR3 , TLR7 | [48] |
| PancTu-1 | Primary tumor | Du | TLR3, TLR7 | [48] |
| Pt45P1 | Primary tumor | Du | TLR3, TLR7 | [48] |
| SU.8686 | Metastasis: liver | Du | TLR2 | [41] |
| SW-1990 | Metastasis: spleen | Du | TLR2-4, TLR7, TLR9 | [23] |
| T3M4 | Metastasis: lymph node | Du | TLR9 | [77] |
| Pathophysiological significance | Ref. | |
| TLR2 | Cell growth | [33,40,43] |
| Immunosuppression | [33,41,43] | |
| Mean survival | [33,35] | |
| Progression and metastasis | [43] | |
| TLR3 | Carcinogenesis | [47] |
| Cell growth and migration | [50] | |
| Immune responses | [48] | |
| TLR4 | Angiogenesis | [63] |
| Carcinogenesis | [49] | |
| Cell growth | [49,57,61] | |
| Epithelial-to-mesenchymal transition | [61] | |
| Leukocyte recruitment and genomic instability | [57] | |
| Mean survival | [62] | |
| Progression and metastasis | [49,58,61] | |
| Stromal expansion | [49,61] | |
| TLR7 | Carcinogenesis, stromal expansion, progression and metastasis | [67] |
| Immune responses | [48] | |
| TLR9 | Cell growth | [77,79] |
| Mean survival | [77] | |
| Metastasis | [72,77,79] |
| Substance/compound | Intervention | Effects | Ref. | |
| TLR2 | MALP-2 (G) | Activation | Induce lymphocyte invasion and tumor necrosis | [33] |
| Inhibit tumor growth | [33] | |||
| Prolongs mean survival | [35] | |||
| Reverse tumor-associated immunosuppression | [33] | |||
| Polysaccharide-K (G) | Activation | Inhibit tumor growth and induce apoptosis in tumor cells | [40] | |
| Dmt-Tic-Cy5 | Activation | Acts as vaccine adjuvant in pancreatic cancer | [41] | |
| Target imaging and therapy | [41,42] | |||
| PAUF | Mixed | Facilitates tumor growth | [43] | |
| Promotes tumor immune-resistance | [43] | |||
| TLR3 | Polycytidylic acid | Activation | Accelerates carcinogenesis | [49] |
| Induces T cell invasion and tumor lysis | [48] | |||
| Phenylmethimazole | Inhibition | Inhibits tumor growth and migration | [50] | |
| TLR4 | Lipopolysaccharide | Activation | Accelerates carcinogenesis | [49] |
| Induce desmoplastic stroma | [49] | |||
| Induce increased H2O2 extracellular production | [57] | |||
| Increased invasiveness | [58,61] | |||
| Induce M2-polarization in tumor-associated macrophages | [61] | |||
| TLR7 | Imiquimod | Activation | Induce T cell invasion and tumor lysis | [48] |
| IRS661 | Inhibition | Prevent tumor progression and stromal expansion | [67] | |
| Regulates cell cycle in cancer cells | [67] | |||
| TLR9 | CpG-ODN 1816/26 (G’) | Activation | Delays tumor development, reduce invasiveness | [72] |
| Prolongs mean survival | [72] | |||
| IMO (C) | Activation | Prolongs mean survival, inhibit tumor growth and migration | [77] | |
| Reestablish cetuximab sensibility in cancer cells | [77] | |||
| CpG-ODN 2216 | Activation | Inhibits tumor growth and migration | [79] |
TLRs are pattern recognition receptors that recognize numerous pathogen-associated molecular patterns (PAMPs) derived from virus, pathogenic bacteria, pathogenic fungus and parasitic protozoa. Likewise, TLRs can start immunological reactions against endogenous molecules released into the extracellular compartment under e.g., stress or tissue damage[24]. TLRs are type I integral membrane glycoproteins expressed in various cell compartments, and in humans the expression of ten different TLRs (TLR1 to TLR10) has been reported[25]. Upon activation, TLRs form heterodimers or homodimers, and an activating signal is started. After the recruitment of adaptor molecules, TLRs can activate two major intracellular signaling pathways. All TLRs, except TLR3, can activate a MyD88-dependent pathway, causing the transcription of pro-inflammatory genes through the activation of nuclear factor κβ (NFκB) and/or the activation of activating protein 1[24,26]. An alternative, non MyD88-dependent pathway, can be initiated by TLR3 and TLR4. In the TRIF-pathway, the activation of interferon-regulated factors (IRF) via TRIF results in the synthesis of interferon (IFN) and/or the activation of NFκB[24].
Mainly expressed on the plasma membrane, TLR2 is found in a large diversity of cells of the immune system[27]. In addition to its role in infectious diseases, TLR2 has been associated to e.g., atherosclerosis, asthma and renal disease[28-30].
Macrophage activating lipopeptide-2 (MALP-2) is a synthetic lipopeptide that activates immune responses through TLR2 and TLR6[31,32]. In syngeneic subcutaneous and in orthotopic murine models the local administration of MALP-2 results in significant tumor growth reduction and prolonged survival[33]. Furthermore, the MALP-2 anti-tumor effect is enhanced by co-treatment with gemcitabine. However, the metastatic potential of cancer cells is not reduced by MALP-2 administration. MALP-2 might exert its effects through CD8+ lymphocytes and NK-cells since the murine Panc-2 cell line used for this experiment do not express TLR2. Hypothetically, MALP-2 activates dendritic cells (DCs) in a TLR2/TLR6-dependent manner[34]. A subsequent phase I/II trial showed promising results[35]. Ten patients in different PDA disease stages were included, both with “radical” surgery or palliative procedures leaving the pancreatic tumor behind. MALP-2 was injected intratumorally during surgery and six patients received adjuvant chemotherapy. The drug was well tolerated and a mean survival of 17.1 mo was observed. The median survival was 9.3 mo and no metastases were reported during follow-up. Despite the limited number of patients, the reported mean survival was remarkably high. The local administration of MALP-2 appears to upregulate the activation of both the innate and the adaptive immune system, resulting in decreased tumor proliferation and metastasis. Still, it is unclear if MALP-2 has a future as adjuvant therapy in PDA, since no further trials have been reported up to date. In addition, several less expensive TLR2 agonists appear to have similar biochemical properties when compared to MALP-2.
Protein-bound polysaccharide-K (PSK, Krestin®) is a natural remedy derived from highly purified mushroom extracts (Trametes versicolor) that since decades has been used as adjuvant therapy in cancer[36]. Even if the mechanisms are only partially known, PSK is thought to be a novel TLR2 agonist and it has documented therapeutic effects in colorectal and lung cancer[37-39]. Moreover, PSK promotes apoptosis and inhibit tumor growth in various human PDA (hPDA) cell lines[40]. Even if PSK-related cancer cell apoptosis is unlikely to be mediated through TLR2, the inhibition of the later significantly reduced the positive effects of PSK in all cell lines challenged. Thus, TLR2-pathways might be (if only in part) involved in the tumor suppressor effect of PSK.
TLR2 is also a promising cell-surface target since its protein expression is specifically increased in hPDA tissue[22]. Designed, fully synthetic high affinity TLR2 agonists have been studied with encouraging outcome. Derived from natural TLR2 ligands and also from MALP-2, these new compounds are able to induce the immune system when given as vaccine adjuvants in murine PDA (mPDA) models[41]. These results imply a potential in developing high affinity tumor targeted therapies through TLR2. A particularly potent compound has been conjugated with a near-infrared fluorescent dye, the novel Dmt-Tic-Cy5. The combination of Dmt-Tic-Cy5 and 3D imaging methods was applied in the intraoperative detection of tumor masses in a mouse xenograft model[42]. Using Dmt-Tic-Cy5 as a tumor marker during surgery in mice, successful R0 resections were obtained. Future applications of this technic could include the detection of early tumors or the improvement of current surgical procedures in hPDA.
Pancreatic adenocarcinoma upregulated factor (PAUF) is a protein overexpressed in hPDA and other types of cancer[43]. PAUF appears to modulate the metastatic potential of cancer cells and it upregulates the expression of CXCR4, the later being related to increased cancer cell motility[44]. PAUF induce the expression of the cytokines RANTES and MIF via TLR2 and it is also associated with the inhibition of CXCR4-dependent and TLR2-mediated NFκB activation, with subsequent decreased tumor necrosis factor-α levels[45]. Theoretically, PAUF might contribute to tumor persistence via the disruption of TLR2-dependent anti-tumor pathways in cancer.
In summary, TLR2 is not only expressed in tumor tissue but also in several hPDA cell lines (Table 1). Since TLR2 is present in both primary tumor cell lines and in cell lines from metastases, the receptor may be a novel target for immunotherapy in hPDA. The clinical significance of TLR2-targeting can become important in the future since the marker is present in up to 70% of resected tumors[22] but mainly absent in the normal pancreas. While the pathophysiological role of TLR2 in mPDA seems to be complex (Table 2, Figure 1), TLR2 agonists have shown promising results in animal models and in a phase I/II clinical trial (Table 3).
TLR3 is a nucleic acid-recognizing receptor expressed as dimers on endosomal membranes of DCs and monocytes. Besides its role in viral infections, TLR3 has been linked to chronic pancreatitis and breast cancer[46,47].
Polycytidylic acid (Poly I:C) is a well-known TLR3 agonist capable of inducing cell lysis in hPDA cell lines by enhancing the cytotoxic activity of γδ T cells in vitro[48]. However, Poly I:C has also been reported to accelerate pancreatic carcinogenesis in KRAS-mutated mice[49].
TLR3 expression in hPDA cell lines is correlated with increased tumor cell growth and constitutive Wnt5a expression[50]. Wnt-associated pathways are related to a vast variety of cellular processes in embryogenesis and carcinogenesis[51]. Phenylmethimazole (C10) is a TLR3 inhibitor able to suppress the dsRNA induced, TLR3-mediated IRF3/IFN-pathway, independent of Wnt5a. The administration of C10 leads to less tumor development in a xenograft murine model. Importantly, C10 decreased TLR3 expression and significantly inhibited hPDA cell growth and motility/migration. The expression of TLR3 in tumor cells might result in increased interleukin (IL)-6 levels[52]. C10 effects could then be mediated by the inhibition of phosphorylated STAT3 via the disruption of TLR3/Wnt5a-related pro-inflammatory IL-6 expression in hPDA.
Even if TLR3 is constitutively expressed in primary hPDA cell lines (Table 1), it is unclear which role TLR3 plays in hPDA. Opposite results have been reported when TLR3 inhibitors have been tried. Hence, no conclusions can be made at this point.
Being the first TLR identified, TLR4 is widely expressed as homodimers or heterodimers with TLR6 on the plasma membranes of many immune cells. TLR4 has been linked to several diseases, including obesity, acute pancreatitis and breast cancer[18,53,54].
TLR4 is overexpressed both in mPDA and hPDA[49]. Stromal leukocytes from patients have increased TLR4 expression. Interestingly, the upregulation is also found both in epithelial and stromal cells in KRAS-mutated mice. Moreover, TLR4-inhibition in these mice had protective effects against tumorigenesis and TLR4-/- animals had a slower tumor growth. However, the inhibition of MyD88-dependent and TRIF-pathways had opposite effects in mPDA. While MyD88-inhibition clearly accelerated tumor development and gave rise to highly aggressive TP53 mutated cancer cells, TRIF-inhibition had anti-tumor effects. MyD88-inhibition could induce aggressive cancer cells even in TRIF-deficiency co-existence.
Even if MyD88 blockage has been associated with a decreased tumor development in other cancer forms[55], the presence of DCs in PDA microenvironment appears to be the main factor for MyD88-dependent tumor-stimulating effects. Upon MyD88 blockage, DCs seem to induce pancreatic antigen-restricted Th2-deviated CD4+ T cells[49]. Furthermore, the abundance of Th2 cells in hPDA is linked to a worsened prognosis[56].
Inflammatory cytokines can induce NFκB activation in mPDA. LPS and INF-γ challenge results in increased production of extracellular H2O2 in primary hPDA cell lines[57]. Through TLR4, the activation of NFκB might enhance the transcription of dual oxidase 2, trigger leukocyte recruitment and genetic instability. In hPDA cell lines, LPS challenge induced improved invasiveness via TLR4/MyD88-depending pathways[58]. Moreover, RNAi silencing TLR4 or MyD88 completely reversed the effects of LPS. NFκB activation might induce increased expression of matrix metalloproteinases (MMPs) in mPDA. MMP-2 and MMP-9 overexpression is related to the progression of hPDA, and its blockage has been subject of intensive research[59]. Thus, LPS may act through a TLR4-MyD88-NFκB axis that finally leads to MMP-9 overexpression and thereby to increased invasiveness in vitro[60].
The overexpression of MMPs has also been coupled to TAMs. M2-polarized TAMs mediate EMT, induce cancer cell proliferation and migration in hPDA cells in vitro[61]. These effects may partially be achieved through TLR4. TLR4 overexpression in M2-polarized macrophages could lead to IL-10 release with impact on the EMT and thereby on the metastatic potential of the cancer cells.
hPDA is characterized by a poor vascularization. Thus, the role of angiogenesis in hPDA remains controversial[9]. In humans, hypoxia-inducible transcription factor alpha (HIF-α) is overexpressed in resected pancreatic cancer tissue. Moreover, a positive correlation between mRNA/protein HIF-α levels and mRNA/protein TLR4 levels in primary tumors and metastases has been found. TLR4 was expressed in 69.2% of the analyzed tumor tissue. Besides, the expression of either TLR4 or HIF-α was related to a decreased survival rate and when both were expressed, an accumulative effect was observed[62]. Some data imply that hypoxia in solid tumors, such as hPDA, induces HIF-α overexpression, which might be responsible for the expression of TLR4 in hPDA cells in vitro and in a xenograft murine model[63]. Here, TLR4 was found in 76 % of the tumor tissue but no data on average survival or prognosis was presented.
The inhibition/blockage of TLR4-related pathways has shown some promising results, but there are still many steps left before TLR4 inhibitors can be considered as possible therapeutic agents. Since both stromal cells and primary tumor cells express TLR4, it is plausible that TLR4 ligands found in the inflammatory tumor microenvironment initiate complex interactions between the different cell populations. This might in turn lead to the secretion of tumor stimulating cytokines and the recruitment of further cell populations into the tumor stroma. Since hypoxia and TLR4 ligands are common in the tumor stroma, the upregulation of TLR4 and HIF-α in hPDA could be auto-stimulatory. Poor prognosis can then be partially predicted, as a highly hypoxic tumor stroma is less sensitive for radiotherapy and disrupt the delivery of chemical agents into the primary cancer cells.
TLR7 is a nucleic acid-recognizing receptor expressed as dimers on endosomal membranes of APCs and leukocytes. TLR7 activation is currently used for the treatment of various malignancies, such as melanoma and breast cancer[64]. Like TLR3, TLR7 has also been used to enhance cytotoxic activity in γδ T cells in vitro[48].
The role of TLR7 in mPDA has been reported previously[65,66]. Upregulated TLR7 is found in epithelial cells and macrophages, DCs, neutrophils, and B- and T-cells of the tumor microenvironment. In hPDA, the expression of TLR7 is increased both in epithelial ductal cells and inflammatory cells within the tumor stroma.
Moreover, the administration of ssRNA40, a TLR7 agonist, results in pronounced tumor growth and stromal expansion in mice. In KRAS-mutated mice, the tumor-stimulating effects of TLR7 appears to be mediated by a complex array of events, including loss of expression of PTEN, p16 and cyclin D1 and upregulation of among others p21, p27, p53, c-Myc, SHPTP1, TGF-β, PPARγ and cyclin B1. Moreover, ssRNA40 challenge resulted in the activation of STAT3, MAP kinase, Notch and NFκB pathways. Notch target genes were downregulated, giving rise to the hypothesis that Notch, together with NFκB, might mediate inflammation in the tumor microenvironment, thus promoting tumor persistence and metastatic potential[67].
Importantly, TLR7 stimulation is not self-sufficient for malignant transition when KRAS mutations are absent. Equally important, mice with TLR7-/- phenotype seem to be protected against tumor progression. The administration of IRS661, an oligonucleotide inhibitor of TLR7, prevented tumor progression and stromal expansion in mice[67]. IRS661 treatment decreased the expression of p21, p27, p-p27, cyclin B1, CDK4 and p-STAT3 in mice with invasive PDA. Thus, TLR7 inhibition was able to affect cell cycle regulation in already formed pancreatic tumors. However, the expression of Rb or TP53 was not affected by IRS661.
The evidence of the importance of TLR7 in mPDA is strong and TLR7 antagonists are without doubt promising experimental adjuvant agents that must be further evaluated. Importantly, PanIN in humans do not express TLR7 with the same intensity as established hPDA tumors. Moreover, the expression of TLR7 appears to increase with tumor progression and it is found in nearly 50% of the advanced tumors[67]. TLR7 may induce tumor progression in a KRAS-dependent manner since the mutation must be present for TLR7-mediated tumor progression in mice. As KRAS2 is mutated in over 90% of hPDA[18], these may only be a minor obstacle for the future clinical use of TLR7-targeting.
As TLR3 and TLR7, TLR9 is expressed on endosomal membranes of several immune cells, including macrophages, B cells and DCs[68]. Besides its role in bacterial, viral or malaria infection, TLR9 has been linked to acute pancreatitis and cancer[54,69].
Synthetic TLR9 agonists (CpG-ODNs) are oligodeoxynucleotides containing CpG motifs that have been used as vaccine adjuvants or as antiallergic agents[70]. In combination with vaccines based on immune stimulatory complexes, a TLR9 agonist inhibits the tumor immune evasion in mPDA[71]. It is believed that CpG-ODNs can activate NK-cells, DCs and cytotoxic T cells, thus initiating anti-tumor immune responses. TLR9 is highly expressed in the tumor microenvironment and in circulating leukocytes in a murine xenograft PDA model. CpG-ODNs treated mice had a reduced tumor spread to the diaphragm, liver and spleen and the combination of gemcitabine and CpG-ODNs resulted in delayed development of bulky disease, less metastasis and improved survival, when compared to gemcitabine monotherapy[72].
The epidermal growth factor receptor (EGFR) is overexpressed in 50%-60% of hPDA[73]. Cetuximab is a monoclonal anti-EGFR antibody that has shown promising results experimentally, but not clinically in hPDA[74,75]. Immunomodulatory nucleotides (IMO) are second-generation CpG-ODNs with higher metabolic stability. IMO interferes with EGFR-dependent signaling and has thereby a synergistic effect with anti-EGFR agents[76]. In combination with cetuximab, IMO inhibits cell growth in hPDA and cancer progression in KRAS-mutated murine cell lines[77]. Importantly, in cetuximab-resistant cell lines, IMO potentiated the activity of cetuximab. The administration of IMO resulted in tumor growth inhibition and prolonged survival in a murine xenograft model. The associations between EGFR/TLRs interactions and carcinogenesis are slowly being elucidated. However, the impact on hPDA is still unexplored[78].
Another CpG-ODN (ODN2216) has shown anti-proliferative properties in an hPDA cell[79]. Tumor cell growth, replication rate and migration ability were decreased in cells challenged with ODN2216. The effects seem to be time- and dose-dependent. Moreover, the expression of TLR9 is more pronounced in hPDA tissue than in peritumoral ones (73.3% vs 33.3%)[79].
As TLR2, TLR9 appears to be a promising tumor marker. Likewise, TLR9 agonists could be used as adjuvant therapy by themselves or in combination with already established chemotherapies (Table 3). Nonetheless, the pathophysiological role of TLR9 in hPDA is mainly unexplored.
The role of the immune system in cancer is an area of intensive research. Cancer cells have the ability to evade immune responses and promote tumor phenotypes and pathways in immune cells. TLRs are related to several cancer forms, and immunotherapies involving TLRs are a reality[27]. At least thirty new clinical trials evaluating TLRs agonist and cancer have started since May 2012[80].
The combination of high mortality rates and a tremendously complex pathophysiology makes PDA an enormous challenge. The role of inflammation and immune cells in PDA cannot be stressed enough[81]. Both MyD88-dependent cascades and TRIF-pathways have been associated with tumor growth, survival and metastatic potential in PDA[65]. Even if almost all known TLRs are expressed in the pancreatic cancer microenvironment, there are only five TLRs suggested as potential therapeutic targets.
Importantly, the effects of TLRs agonists and antagonists in PDA are presumably mediated by the inducement of anti-tumor immune response. This requires access to the primary tumor site. Moreover, TLR-targeting can theoretically disrupt important pathways in primary tumor cells with therapeutic effects. Thus, TLR-based agents must either be administered intratumorally or delivered through the tumor stroma. The recognition of specific tumor targets is then imperative for the application of TLRs intervention in PDA. In clinical practice, CA 19-9 is widely used as hPDA marker. CA 19-9 is a relatively specific marker useful as indicator for advanced disease or tumor recurrence after surgery. However, as pancreatic cancer progress and spreads beyond the pancreas, the accumulation of abnormalities might change the sensitivity and/or specificity of tumor markers since metastases may differ profoundly from the primary tumor[82]. We have recently propose mucin 4 (MUC4) as a novel tumor marker in hPDA. MUC4 is found in both primary and matched metastatic tumors with a high level of concordance (82 %)[83]. Specific tumor markers open the door for efficient drug delivery via e.g., nanotechnology. For instance, targeted liposomal delivery of TLR9 ligands in cancer has already been evaluated with encouraging results[84].
Independently of their potential in immunotherapies, all existing data indicate that TLRs are strongly involved in the pathophysiology of PDA (Figure 1). The role of TLRs in PDA is not limited to the direct effect on tumors or associated cells. TLRs are also involved in the pathophysiology of several risk factors for hPDA, such as chronic pancreatitis, diabetes and obesity[47,85].
The present paper summarizes the current understanding of interventions on TLRs in PDA. Despite initial encouraging results, further research and elucidation of involved mechanisms is demanded.
P- Reviewers: Yip-Schneider MT, Zhang AM S- Editor: Zhai HH L- Editor: A E- Editor: Zhang DN
| 1. | Warshaw AL, Fernández-del Castillo C. Pancreatic carcinoma. N Engl J Med. 1992;326:455-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1056] [Cited by in RCA: 1015] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 2. | Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363:1049-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1481] [Cited by in RCA: 1545] [Article Influence: 73.6] [Reference Citation Analysis (0)] |
| 3. | Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9215] [Cited by in RCA: 9856] [Article Influence: 821.3] [Reference Citation Analysis (4)] |
| 4. | Shi C, Hruban RH, Klein AP. Familial pancreatic cancer. Arch Pathol Lab Med. 2009;133:365-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 5. | Pandol SJ, Apte MV, Wilson JS, Gukovskaya AS, Edderkaoui M. The burning question: why is smoking a risk factor for pancreatic cancer? Pancreatology. 2012;12:344-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Shikata K, Ninomiya T, Kiyohara Y. Diabetes mellitus and cancer risk: review of the epidemiological evidence. Cancer Sci. 2013;104:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 193] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 7. | Gukovsky I, Li N, Todoric J, Gukovskaya A, Karin M. Inflammation, autophagy, and obesity: common features in the pathogenesis of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1199-1209.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 253] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 8. | Hruban RH, Maitra A, Goggins M. Update on pancreatic intraepithelial neoplasia. Int J Clin Exp Pathol. 2008;1:306-316. [PubMed] |
| 9. | Feldmann G, Beaty R, Hruban RH, Maitra A. Molecular genetics of pancreatic intraepithelial neoplasia. J Hepatobiliary Pancreat Surg. 2007;14:224-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 180] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 10. | Apte MV, Wilson JS, Lugea A, Pandol SJ. A starring role for stellate cells in the pancreatic cancer microenvironment. Gastroenterology. 2013;144:1210-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 366] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 11. | Li C, Lee CJ, Simeone DM. Identification of human pancreatic cancer stem cells. Methods Mol Biol. 2009;568:161-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 165] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 12. | Yoshikawa K, Mitsunaga S, Kinoshita T, Konishi M, Takahashi S, Gotohda N, Kato Y, Aizawa M, Ochiai A. Impact of tumor-associated macrophages on invasive ductal carcinoma of the pancreas head. Cancer Sci. 2012;103:2012-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 13. | Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2078] [Cited by in RCA: 2206] [Article Influence: 147.1] [Reference Citation Analysis (2)] |
| 14. | Hidalgo M. New insights into pancreatic cancer biology. Ann Oncol. 2012;23 Suppl 10:x135-x138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Burris HA, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15:2403-2413. [PubMed] |
| 16. | Andersson R, Aho U, Nilsson BI, Peters GJ, Pastor-Anglada M, Rasch W, Sandvold ML. Gemcitabine chemoresistance in pancreatic cancer: molecular mechanisms and potential solutions. Scand J Gastroenterol. 2009;44:782-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Ansari D, Tingstedt B, Andersson R. Pancreatic cancer - cost for overtreatment with gemcitabine. Acta Oncol. 2013;52:1146-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Jarboe J, Saif MW. First line therapy for metastatic pancreatic cancer. JOP. 2013;14:340-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Ahmed A, Redmond HP, Wang JH. Links between Toll-like receptor 4 and breast cancer. Oncoimmunology. 2013;2:e22945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 20. | Eyking A, Ey B, Rünzi M, Roig AI, Reis H, Schmid KW, Gerken G, Podolsky DK, Cario E. Toll-like receptor 4 variant D299G induces features of neoplastic progression in Caco-2 intestinal cells and is associated with advanced human colon cancer. Gastroenterology. 2011;141:2154-2165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Thomas A, Hassan R. Immunotherapies for non-small-cell lung cancer and mesothelioma. Lancet Oncol. 2012;13:e301-e310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Morse DL, Balagurunathan Y, Hostetter G, Trissal M, Tafreshi NK, Burke N, Lloyd M, Enkemann S, Coppola D, Hruby VJ. Identification of novel pancreatic adenocarcinoma cell-surface targets by gene expression profiling and tissue microarray. Biochem Pharmacol. 2010;80:748-754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Rosenberg JS, Singh S, Raul S, Tong Z, Guha S. Pancreatic cancer screening by TLR phenotyping. Cancer Research. 2011;71:Abstract nr 894. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Piccinini AM, Midwood KS. DAMPening inflammation by modulating TLR signalling. Mediators Inflamm. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 692] [Cited by in RCA: 691] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 25. | Hedayat M, Netea MG, Rezaei N. Targeting of Toll-like receptors: a decade of progress in combating infectious diseases. Lancet Infect Dis. 2011;11:702-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 26. | O’Neill LA, Bowie AG. The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling. Nat Rev Immunol. 2007;7:353-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1836] [Cited by in RCA: 2013] [Article Influence: 111.8] [Reference Citation Analysis (0)] |
| 27. | O’Neill LA, Bryant CE, Doyle SL. Therapeutic targeting of Toll-like receptors for infectious and inflammatory diseases and cancer. Pharmacol Rev. 2009;61:177-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 350] [Cited by in RCA: 340] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 28. | Anders HJ, Banas B, Schlöndorff D. Signaling danger: toll-like receptors and their potential roles in kidney disease. J Am Soc Nephrol. 2004;15:854-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 295] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 29. | Eder W, Klimecki W, Yu L, von Mutius E, Riedler J, Braun-Fahrländer C, Nowak D, Martinez FD. Toll-like receptor 2 as a major gene for asthma in children of European farmers. J Allergy Clin Immunol. 2004;113:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 330] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 30. | Satoh M, Ishikawa Y, Minami Y, Takahashi Y, Nakamura M. Role of Toll like receptor signaling pathway in ischemic coronary artery disease. Front Biosci. 2008;13:6708-6715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Morr M, Takeuchi O, Akira S, Simon MM, Mühlradt PF. Differential recognition of structural details of bacterial lipopeptides by toll-like receptors. Eur J Immunol. 2002;32:3337-3347. [PubMed] |
| 32. | Takeuchi O, Kaufmann A, Grote K, Kawai T, Hoshino K, Morr M, Mühlradt PF, Akira S. Cutting edge: preferentially the R-stereoisomer of the mycoplasmal lipopeptide macrophage-activating lipopeptide-2 activates immune cells through a toll-like receptor 2- and MyD88-dependent signaling pathway. J Immunol. 2000;164:554-557. [PubMed] |
| 33. | Schneider C, Schmidt T, Ziske C, Tiemann K, Lee KM, Uhlinsky V, Behrens P, Sauerbruch T, Schmidt-Wolf IG, Mühlradt PF. Tumour suppression induced by the macrophage activating lipopeptide MALP-2 in an ultrasound guided pancreatic carcinoma mouse model. Gut. 2004;53:355-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Weigt H, Mühlradt PF, Emmendörffer A, Krug N, Braun A. Synthetic mycoplasma-derived lipopeptide MALP-2 induces maturation and function of dendritic cells. Immunobiology. 2003;207:223-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Schmidt J, Welsch T, Jäger D, Mühlradt PF, Büchler MW, Märten A. Intratumoural injection of the toll-like receptor-2/6 agonist ‘macrophage-activating lipopeptide-2’ in patients with pancreatic carcinoma: a phase I/II trial. Br J Cancer. 2007;97:598-604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 36. | Sun C, Rosendahl AH, Wang XD, Wu DQ, Andersson R. Polysaccharide-K (PSK) in cancer--old story, new possibilities? Curr Med Chem. 2012;19:757-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Hayakawa K, Mitsuhashi N, Saito Y, Nakayama Y, Furuta M, Nakamoto S, Kawashima M, Niibe H. Effect of Krestin as adjuvant treatment following radical radiotherapy in non-small cell lung cancer patients. Cancer Detect Prev. 1997;21:71-77. [PubMed] |
| 38. | Lu H, Yang Y, Gad E, Wenner CA, Chang A, Larson ER, Dang Y, Martzen M, Standish LJ, Disis ML. Polysaccharide krestin is a novel TLR2 agonist that mediates inhibition of tumor growth via stimulation of CD8 T cells and NK cells. Clin Cancer Res. 2011;17:67-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 120] [Cited by in RCA: 114] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 39. | Ohwada S, Ikeya T, Yokomori T, Kusaba T, Roppongi T, Takahashi T, Nakamura S, Kakinuma S, Iwazaki S, Ishikawa H. Adjuvant immunochemotherapy with oral Tegafur/Uracil plus PSK in patients with stage II or III colorectal cancer: a randomised controlled study. Br J Cancer. 2004;90:1003-1010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 40. | Rosendahl AH, Sun C, Wu D, Andersson R. Polysaccharide-K (PSK) increases p21(WAF/Cip1) and promotes apoptosis in pancreatic cancer cells. Pancreatology. 2012;12:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Huynh AS, Chung WJ, Cho HI, Moberg VE, Celis E, Morse DL, Vagner J. Novel toll-like receptor 2 ligands for targeted pancreatic cancer imaging and immunotherapy. J Med Chem. 2012;55:9751-9762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Huynh AS, Patek R, Abrahams D, Baldwin MK, Lioyd MC, Centeno BA, Vagner J, Gillies R, Morse DL. Intraoperative detection of pancreatic cancer using tumor targeted fluorescent probes. Mol Imaging Biol. 2012;14:S979. |
| 43. | Kim SA, Lee Y, Jung DE, Park KH, Park JY, Gang J, Jeon SB, Park EC, Kim YG, Lee B. Pancreatic adenocarcinoma up-regulated factor (PAUF), a novel up-regulated secretory protein in pancreatic ductal adenocarcinoma. Cancer Sci. 2009;100:828-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 44. | Lee Y, Kim SJ, Park HD, Park EH, Huang SM, Jeon SB, Kim JM, Lim DS, Koh SS. PAUF functions in the metastasis of human pancreatic cancer cells and upregulates CXCR4 expression. Oncogene. 2010;29:56-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 45. | Park HD, Lee Y, Oh YK, Jung JG, Park YW, Myung K, Kim KH, Koh SS, Lim DS. Pancreatic adenocarcinoma upregulated factor promotes metastasis by regulating TLR/CXCR4 activation. Oncogene. 2011;30:201-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 46. | Andre F, Slimane K, Bachelot T, Dunant A, Namer M, Barrelier A, Kabbaj O, Spano JP, Marsiglia H, Rouzier R. Breast cancer with synchronous metastases: trends in survival during a 14-year period. J Clin Oncol. 2004;22:3302-3308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 274] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 47. | Soga Y, Komori H, Miyazaki T, Arita N, Terada M, Kamada K, Tanaka Y, Fujino T, Hiasa Y, Matsuura B. Toll-like receptor 3 signaling induces chronic pancreatitis through the Fas/Fas ligand-mediated cytotoxicity. Tohoku J Exp Med. 2009;217:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Shojaei H, Oberg HH, Juricke M, Marischen L, Kunz M, Mundhenke C, Gieseler F, Kabelitz D, Wesch D. Toll-like receptors 3 and 7 agonists enhance tumor cell lysis by human gammadelta T cells. Cancer Res. 2009;69:8710-8717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 49. | Ochi A, Nguyen AH, Bedrosian AS, Mushlin HM, Zarbakhsh S, Barilla R, Zambirinis CP, Fallon NC, Rehman A, Pylayeva-Gupta Y. MyD88 inhibition amplifies dendritic cell capacity to promote pancreatic carcinogenesis via Th2 cells. J Exp Med. 2012;209:1671-1687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 242] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 50. | Schwartz AL, Malgor R, Dickerson E, Weeraratna AT, Slominski A, Wortsman J, Harii N, Kohn AD, Moon RT, Schwartz FL. Phenylmethimazole decreases Toll-like receptor 3 and noncanonical Wnt5a expression in pancreatic cancer and melanoma together with tumor cell growth and migration. Clin Cancer Res. 2009;15:4114-4122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 51. | Katoh M, Katoh M. Transcriptional mechanisms of WNT5A based on NF-kappaB, Hedgehog, TGFbeta, and Notch signaling cascades. Int J Mol Med. 2009;23:763-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 141] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 52. | Harii N, Lewis CJ, Vasko V, McCall K, Benavides-Peralta U, Sun X, Ringel MD, Saji M, Giuliani C, Napolitano G. Thyrocytes express a functional toll-like receptor 3: overexpression can be induced by viral infection and reversed by phenylmethimazole and is associated with Hashimoto’s autoimmune thyroiditis. Mol Endocrinol. 2005;19:1231-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 53. | Kleinridders A, Schenten D, Könner AC, Belgardt BF, Mauer J, Okamura T, Wunderlich FT, Medzhitov R, Brüning JC. MyD88 signaling in the CNS is required for development of fatty acid-induced leptin resistance and diet-induced obesity. Cell Metab. 2009;10:249-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 389] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 54. | Vaz J, Akbarshahi H, Andersson R. Controversial role of toll-like receptors in acute pancreatitis. World J Gastroenterol. 2013;19:616-630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 55. | Rakoff-Nahoum S, Medzhitov R. Regulation of spontaneous intestinal tumorigenesis through the adaptor protein MyD88. Science. 2007;317:124-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 456] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 56. | De Monte L, Reni M, Tassi E, Clavenna D, Papa I, Recalde H, Braga M, Di Carlo V, Doglioni C, Protti MP. Intratumor T helper type 2 cell infiltrate correlates with cancer-associated fibroblast thymic stromal lymphopoietin production and reduced survival in pancreatic cancer. J Exp Med. 2011;208:469-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 464] [Cited by in RCA: 554] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 57. | Wu Y, Lu J, Antony S, Juhasz A, Liu H, Jiang G, Meitzler JL, Hollingshead M, Haines DC, Butcher D. Activation of TLR4 is required for the synergistic induction of dual oxidase 2 and dual oxidase A2 by IFN-γ and lipopolysaccharide in human pancreatic cancer cell lines. J Immunol. 2013;190:1859-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 58. | Ikebe M, Kitaura Y, Nakamura M, Tanaka H, Yamasaki A, Nagai S, Wada J, Yanai K, Koga K, Sato N. Lipopolysaccharide (LPS) increases the invasive ability of pancreatic cancer cells through the TLR4/MyD88 signaling pathway. J Surg Oncol. 2009;100:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 132] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 59. | Bloomston M, Zervos EE, Rosemurgy AS. Matrix metalloproteinases and their role in pancreatic cancer: a review of preclinical studies and clinical trials. Ann Surg Oncol. 2002;9:668-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 124] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 60. | Del Pozo JL. Primers on molecular pathways: lipopolysaccharide signaling - potential role in pancreatitis and pancreatic cancer. Pancreatology. 2010;10:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 61. | Liu CY, Xu JY, Shi XY, Huang W, Ruan TY, Xie P, Ding JL. M2-polarized tumor-associated macrophages promoted epithelial-mesenchymal transition in pancreatic cancer cells, partially through TLR4/IL-10 signaling pathway. Lab Invest. 2013;93:844-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 356] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 62. | Zhang JJ, Wu HS, Wang L, Tian Y, Zhang JH, Wu HL. Expression and significance of TLR4 and HIF-1alpha in pancreatic ductal adenocarcinoma. World J Gastroenterol. 2010;16:2881-2888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 64] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 63. | Fan P, Zhang JJ, Wang B, Wu HQ, Zhou SX, Wang CY, Zhang JH, Tian Y, Wu HS. Hypoxia-inducible factor-1 up-regulates the expression of Toll-like receptor 4 in pancreatic cancer cells under hypoxic conditions. Pancreatology. 2012;12:170-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 64. | Kanzler H, Barrat FJ, Hessel EM, Coffman RL. Therapeutic targeting of innate immunity with Toll-like receptor agonists and antagonists. Nat Med. 2007;13:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 678] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 65. | Zambirinis CP, Miller G. Signaling via MYD88 in the pancreatic tumor microenvironment: A double-edged sword. Oncoimmunology. 2013;2:e22567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 66. | Zambirinis CP, Ochi A, Barilla R, Greco S, Deutsch M, Miller G. Induction of TRIF- or MYD88-dependent pathways perturbs cell cycle regulation in pancreatic cancer. Cell Cycle. 2013;12:1153-1154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 67. | Ochi A, Graffeo CS, Zambirinis CP, Rehman A, Hackman M, Fallon N, Barilla RM, Henning JR, Jamal M, Rao R. Toll-like receptor 7 regulates pancreatic carcinogenesis in mice and humans. J Clin Invest. 2012;122:4118-4129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 162] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 68. | Hemmi H, Takeuchi O, Kawai T, Kaisho T, Sato S, Sanjo H, Matsumoto M, Hoshino K, Wagner H, Takeda K. A Toll-like receptor recognizes bacterial DNA. Nature. 2000;408:740-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4803] [Cited by in RCA: 4823] [Article Influence: 192.9] [Reference Citation Analysis (0)] |
| 69. | Noack J, Jordi M, Zauner L, Alessi D, Burch A, Tinguely M, Hersberger M, Bernasconi M, Nadal D. TLR9 agonists induced cell death in Burkitt’s lymphoma cells is variable and influenced by TLR9 polymorphism. Cell Death Dis. 2012;3:e323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 70. | Krieg AM. Therapeutic potential of Toll-like receptor 9 activation. Nat Rev Drug Discov. 2006;5:471-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 935] [Cited by in RCA: 986] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 71. | Jacobs C, Duewell P, Heckelsmiller K, Wei J, Bauernfeind F, Ellermeier J, Kisser U, Bauer CA, Dauer M, Eigler A. An ISCOM vaccine combined with a TLR9 agonist breaks immune evasion mediated by regulatory T cells in an orthotopic model of pancreatic carcinoma. Int J Cancer. 2011;128:897-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 72. | Pratesi G, Petrangolini G, Tortoreto M, Addis A, Belluco S, Rossini A, Selleri S, Rumio C, Menard S, Balsari A. Therapeutic synergism of gemcitabine and CpG-oligodeoxynucleotides in an orthotopic human pancreatic carcinoma xenograft. Cancer Res. 2005;65:6388-6393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 73. | Friess H, Wang L, Zhu Z, Gerber R, Schröder M, Fukuda A, Zimmermann A, Korc M, Büchler MW. Growth factor receptors are differentially expressed in cancers of the papilla of vater and pancreas. Ann Surg. 1999;230:767-774; discussion 774-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 74. | Heinemann V, Haas M, Boeck S. Systemic treatment of advanced pancreatic cancer. Cancer Treat Rev. 2012;38:843-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 75. | Xiong HQ, Rosenberg A, LoBuglio A, Schmidt W, Wolff RA, Deutsch J, Needle M, Abbruzzese JL. Cetuximab, a monoclonal antibody targeting the epidermal growth factor receptor, in combination with gemcitabine for advanced pancreatic cancer: a multicenter phase II Trial. J Clin Oncol. 2004;22:2610-2616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 337] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 76. | Damiano V, Caputo R, Bianco R, D’Armiento FP, Leonardi A, De Placido S, Bianco AR, Agrawal S, Ciardiello F, Tortora G. Novel toll-like receptor 9 agonist induces epidermal growth factor receptor (EGFR) inhibition and synergistic antitumor activity with EGFR inhibitors. Clin Cancer Res. 2006;12:577-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 77. | Rosa R, Melisi D, Damiano V, Bianco R, Garofalo S, Gelardi T, Agrawal S, Di Nicolantonio F, Scarpa A, Bardelli A. Toll-like receptor 9 agonist IMO cooperates with cetuximab in K-ras mutant colorectal and pancreatic cancers. Clin Cancer Res. 2011;17:6531-6541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 78. | Liu K, Anderson GP, Bozinovski S. DNA vector augments inflammation in epithelial cells via EGFR-dependent regulation of TLR4 and TLR2. Am J Respir Cell Mol Biol. 2008;39:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 79. | Wu HQ, Wang B, Zhu SK, Tian Y, Zhang JH, Wu HS. Effects of CPG ODN on biological behavior of PANC-1 and expression of TLR9 in pancreatic cancer. World J Gastroenterol. 2011;17:996-1003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 80. | Galluzzi L, Vacchelli E, Eggermont A, Fridman WH, Galon J, Sautès-Fridman C, Tartour E, Zitvogel L, Kroemer G. Trial Watch: Experimental Toll-like receptor agonists for cancer therapy. Oncoimmunology. 2012;1:699-716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 171] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 81. | Zheng L, Xue J, Jaffee EM, Habtezion A. Role of immune cells and immune-based therapies in pancreatitis and pancreatic ductal adenocarcinoma. Gastroenterology. 2013;144:1230-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 253] [Article Influence: 21.1] [Reference Citation Analysis (1)] |
| 82. | Venook AP, Stagg RJ, Lewis BJ. Regional chemotherapy for colorectal cancer metastatic to the liver. Oncology (Williston Park). 1988;2:19-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 83. | Ansari D, Urey C, Gundewar C, Bauden MP, Andersson R. Comparison of MUC4 expression in primary pancreatic cancer and paired lymph node metastases. Scand J Gastroenterol. 2013;48:1183-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 84. | Hamzah J, Altin JG, Herringson T, Parish CR, Hämmerling GJ, O’Donoghue H, Ganss R. Targeted liposomal delivery of TLR9 ligands activates spontaneous antitumor immunity in an autochthonous cancer model. J Immunol. 2009;183:1091-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 85. | Fresno M, Alvarez R, Cuesta N. Toll-like receptors, inflammation, metabolism and obesity. Arch Physiol Biochem. 2011;117:151-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |