Published online May 14, 2014. doi: 10.3748/wjg.v20.i18.5561
Revised: February 27, 2014
Accepted: March 6, 2014
Published online: May 14, 2014
Processing time: 179 Days and 2.9 Hours
A 62-year-old woman was admitted to our hospital in 2011 because of recurrent abdominal pain, nausea and constipation for six months. Computed tomography enterography (CTE) showed tortuous thread-like calcifications in the ileocolic vein and right colic vein, while colonoscopy revealed purple-blue mucosa extending from the cecum to the splenic flexure. Based on the results of these tests, the patient was diagnosed with idiopathic mesenteric phlebosclerosis (IMP). She had a history of Chinese medical liquor intake for one and a half years and her symptoms subsided after conservative treatment. In 2013, a 63-year-old male patient who presented with recurrent lower right abdominal pain, bloating, melena and diarrhea for fifteen months was admitted to our institution. Colonoscopy and CTE led to the diagnosis of IMP. He also used Chinese medical liquor for approximately 12 years. The patient underwent total colectomy and the postoperative course was uneventful. We searched for previously published reports on similar cases and analyzed the clinical data of 50 cases identified in PubMed. As some of these patients admitted use of Chinese medicines, we hypothesize that Chinese medicines may play a role in the pathogenesis of IMP.
Core tip: The clinical data of two idiopathic mesenteric phlebosclerosis (IMP) patients in our hospital were collected. Both patients presented with recurrent ileus and displayed typical imaging characteristics such as dark purple mucosa on endoscopy and calcifications in mesenteric veins on computed tomography enterography. Both patients confirmed long-term use of Chinese medical liquor. After discontinuing the product, the first patient received conservative treatment, while the second underwent surgery. To date, both patients remain healthy. Following a literature review, a further 50 cases of IMP were analyzed, and it was concluded that the use of Chinese medicines may play a role in the pathogenesis of IMP.
- Citation: Guo F, Zhou YF, Zhang F, Yuan F, Yuan YZ, Yao WY. Idiopathic mesenteric phlebosclerosis associated with long-term use of medical liquor: Two case reports and literature review. World J Gastroenterol 2014; 20(18): 5561-5566
- URL: https://www.wjgnet.com/1007-9327/full/v20/i18/5561.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i18.5561
Idiopathic mesenteric phlebosclerosis (IMP) is a rare disease, and the etiology and pathogenesis are unclear. IMP can be diagnosed based on characteristic imaging findings such as thread-like calcifications in the mesenteric veins on computed tomography (CT) associated with purple-blue mucosa on colonoscopy. The disease was first described by Koyama et al[1] in 1991. In 2000, in order to distinguish this disease from ischemic colitis caused by arterial diseases, Yao et al[2] named this rarity ‘‘phlebosclerotic colitis’’. In 2003, Iwashita et al[3] proposed the term “idiopathic mesenteric phlebosclerosis”, as this disease was not an inflammatory disease.
Herein, we present two cases of IMP seen at our department over the last two years, and both patients had a history of Chinese medical liquor intake for a number of years.
In 2011, a 62-year-old woman was admitted to our institution with the main complaints of recurrent abdominal pain, nausea and constipation for six months. Partial intestinal obstruction was diagnosed in local hospitals. The patient denied any personal or family history of liver cirrhosis, hypertension or inflammatory vascular diseases. However, she admitted the intake of Chinese medical liquor for one and a half years. Her physical examination revealed no abnormalities and laboratory testing, including routine blood analysis, C-reactive protein, occult blood test and other biochemical tests were normal, except for elevated antinuclear antibodies (ANA) (1:100).
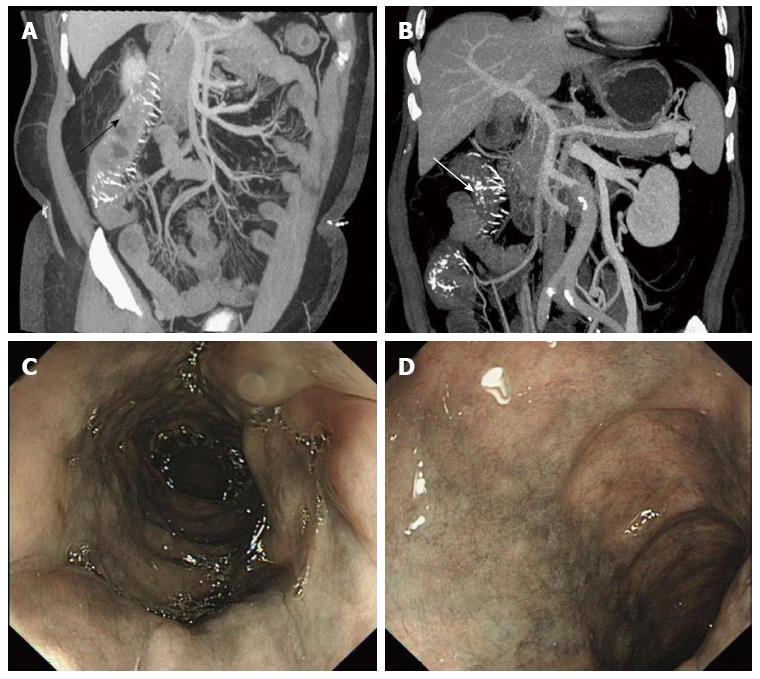
Computed tomography enterography (CTE) (Figure 1A) showed an enlarged appendix, diffuse mural thickening of the ileocecal area, the ascending colon and the transverse colon, and tortuous thread-like calcifications were observed in the ileocolic and right colic veins. Crohn’s disease was initially suspected due to insufficient recognition of IMP. Colonoscopy revealed significant rigidity along the intestinal wall, with purple-blue mucosa extending from the cecum to the splenic flexure (Figure 1C, D). Computed tomography angiography (CTA) was performed and calcifications were found in the same veins (Figure 1B) as described in the CTE. The test results combined with the examination findings confirmed the diagnosis of IMP.
The patient was asked to discontinue the medical liquor and received conservative treatment including low-residue diet. Her symptoms eventually subsided. Following discharge, the patient was followed up for approximately 28 mo and to date, there has been no recurrence of ileus or abdominal discomfort.
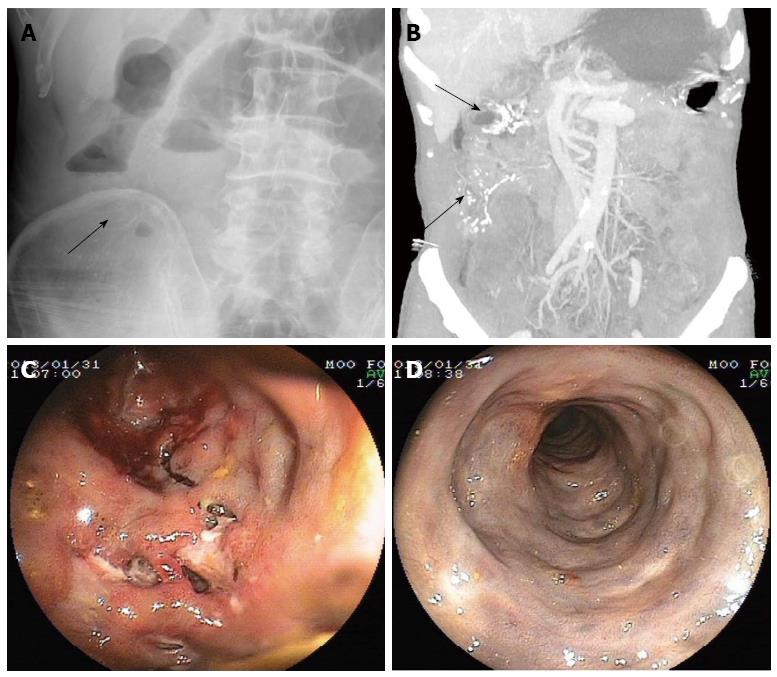
In January 2013, a 63-year-old male patient presented with recurrent lower right abdominal pain, bloating, and melena diarrhea for 15 mo. The patient also had a history of consuming Chinese medical liquor for over 12 years. Inflammatory bowel disease (IBD) was diagnosed elsewhere and he was treated with sulfasalazine. However, this treatment was ineffective. On admission, physical examination showed a non-distended abdomen with mild tenderness in the lower right quadrant. Laboratory tests were almost normal. Plain abdominal X-ray showed thread-like calcifications in the right colon region and dilation in the small intestine, suggesting an incomplete low position obstruction (Figure 2A). Colonoscopy revealed purple-blue mucosa extending from the cecum to the sigmoid, and multiple ulcers were found in the ascending and transverse colon, some of the ulcers in the ascending colon were longitudinal with a purulent surface; openings of suspected fistulas were seen in the cecal area (Figure 2C, D). CTE showed that the wall from the cecum to the descending colon was thickened, especially in the right hemi-colon; the haustra coli had disappeared and the “lead pipe” sign was prominent; thread-like calcifications were seen in the right, middle and left colic veins (Figure 2B). Based on these findings, IMP was diagnosed. However, endoscopic findings could not completely eliminate the possibility of coexisting Crohn’s disease.
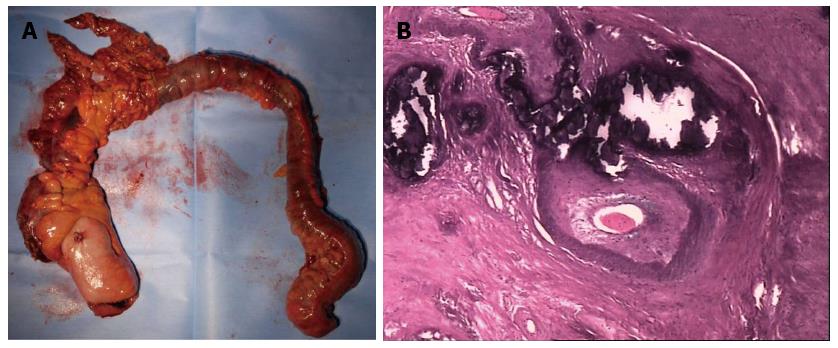
The treatment plan primarily consisted of a clear-liquid diet, vasodilators and a course of mesalazine. However, the patient’s abdominal pain worsened again in March 2013, and he presented with lack of bowel movement and flatulence. Conservative therapy was considered ineffective and a total colectomy with ileostomy was performed, the stoma was closed four months later. The macroscopic appearance (Figure 3A) of the resected specimen consisted of cyanotic, thickened and rigid colonic mucosa with multiple ulcerations. Microscopic examination of the specimen showed vascular proliferation in the mesentery and in the sub-mucosa and serosal layers of the intestinal wall; these vascular walls were thickened, with obvious calcification, while collagen deposition and hyaline degeneration were seen. Dysplasia, cancer and acute ischemic colitis were not observed (Figure 3B).
The postoperative course was uneventful and the patient was followed up regularly with no recurrence of abdominal discomfort to date.
Idiopathic mesenteric phlebosclerosis is a rare, but characteristic disease. Knowledge of its distinctive endoscopic and computed tomographic appearance may lead to early diagnosis. However, the etiology of IMP has not been completely defined. We reviewed the literature in the PubMed database by searching for articles related to “phlebosclerotic colitis” or “mesenteric phlebosclerosis” and found 28 articles and a total of 50 cases related to the disease.
Combining the 50 cases identified in PubMed and the two cases in this study, a detailed analysis of the clinical data of all 52 cases was performed. The average age of these patients was 59.8 years and 53.8% were men. We noted that the majority of patients were Asians, mostly from Japan and Taiwan, 5 of the 52 patients were from Mainland China[4] and 2 from South Korea[5,6]. IMP was reported by Markos et al[7] in a patient from Canada, however, the patient was found to be of Taiwanese descent.
Due to a lack of knowledge and information on IMP and as the clinical manifestations and laboratory examinations of IMP lack specificity, some patients (9/52) were initially misdiagnosed with other diseases such as IBD[2,8], acute colitis[2,9] and acute appendicitis[8]. In the two cases presented in this study, we also considered an initial diagnosis of IBD. The clinical manifestations in all 52 patients were mainly characterized by a gradual onset of right-sided abdominal pain and/or diarrhea or recurrent ileus; melena was recorded in six patients, while intestinal perforation was noted in two patients[10,11]. Some of the reported patients were asymptomatic[12,13]. No specificity was noted in the laboratory examinations except fecal occult blood test was found to be positive in 15 patients. Our two cases did not show any specificity in terms of laboratory examinations.
Significant characteristic findings were observed on radiological examinations and endoscopy. An awareness of the characteristic imaging patterns of IMP is crucial for correct diagnosis. In the majority of plain radiographs in IMP patients, multiple linear calcifications were seen mainly in the right lower region of the abdomen, sometimes extending into the transverse colon. CT features included thickening of the affected colonic wall with calcification of the involved mesenteric vein tributaries. Further investigation such as CTA can demonstrate the precise location and extent of the calcifications. Both of our patients underwent CTE which has not been described in previously reported patients. CTE clearly showed the lesions in the colon and revealed the particular vein affected. Thus, we believe that CT may be the modality of choice for the diagnosis of IMP. However, CTE is an ideal choice as it is capable of identifying the severity of the lesion and precisely locating the calcifications which could prompt further treatment or investigations.
On colonoscopy, the typical and characteristic finding was dark-purple, edematous or rigid mucosa. In some cases, erosion, ulceration and luminal narrowing were observed, depending on the severity of disease. Eighteen out of the 52 patients were seen with ulcerative lesions during colonoscopy, mostly at the ascending colon while luminal narrowing was found in 11 of the patients.
Histopathologic characteristics included thickening of the venous wall with calcifications and fibrosis in the mesentery and intestinal wall. In some patients, mucosal atrophy, ulceration and inflammation were also found. Colonic cancer was reported in three patients[3,13,14], and the cancerous sites were all located in the right hemi-colon, in the same region as the mesenteric phlebosclerotic lesions. This forced us to consider the possibility of IMP stimulating the occurrence of colonic cancer. However, since the data pool was insufficient, further study is needed to confirm whether there is a risk of colonic cancer evolution in patients with IMP. Colonic cancer screening in patients with IMP should be included in the follow-up plan.
Unlike the imaging trends, the pathogenesis of IMP remains unclear. An association with a region-specific lifestyle has been speculated, as most reported cases are from East Asia. Portal vein hypertension[15] and alcohol consumption have also been considered possible etiologies. Kitamura et al[11] reported that the pathogenesis of phlebosclerosis in the colon was related to the CREST syndrome. However, no other similar cases have been reported.
It is interesting to note that 16 of the 52 patients had a history of using Chinese medicines[8,13,16-19] while the other cases lacked accurate detailed information on the use of Chinese medicines.When considering the possibility that some Chinese medicine constituents may be a direct or indirect cause of IMP, Dr. Chang[8] collected clinical data from 5 patients who had been using Chinese herbs for several years and reviewed histologic sections in detail from 4 of these cases. He concluded that certain toxins or biochemicals, probably existing in the frequently ingested herbs, may be absorbed during venous return and might play an important role in IMP. Hiramatsu et al[13] demonstrated that long-term use of geniposide which is found in herbal medicines appears to be associated with mesenteric phlebosclerosis. In the two cases report here, both patients had a history of taking the Chinese medical liquor, Acanthopanax gracilistylus Wine, which is composed of multiple Chinese herbs soaked in liquor and is said to have various effects such as enhancing fitness and optimizing immune response. The medical liquor used by our two patients contains geniposide, which is a traditional Chinese medicine and adds weight to the conclusion by Hiramatsu et al[13]. Other herbs such as Angelica sinensis and Cortex acanthopanacis are also found in this type of medical liquor. Hozumi et al[9] also described a patient who used geniposide-containing Chinese herbs. All of the 16 patients had onset of clinical symptoms following long-term use of herbs. The average duration of Chinese herb consumption was 13.5 years and the mean duration was 1.5 years. When analyzing our two cases, we also found that the patient who used medical alcohol for one and half years had relatively mild symptoms, while the patient who used these herbs for 12 years had severe lesions and progressive symptoms, which suggests that the amount and duration of herb intake could be a determining factor in the severity of the disease. Therefore, we support the theory that Chinese medicines are most probably involved in the pathology of IMP. However, if geniposide or other Chinese medicine is directly involved in the pathogenesis of IMP, this may be determined by further experimentation using a larger data set. The current data pool of 52 cases is insufficient, thus, experimentation in laboratory animals could be performed in order to understand the mechanism and causes of IMP.
Idiopathic mesenteric phlebosclerosis is a rare, but characteristic entity which may easily be missed or misdiagnosed due to a lack of knowledge and information on the disease. It is crucial to recognize the characteristics of the disease such as clinical manifestations and characteristic imaging features including calcification on CT and dark-purple mucosa on colonoscopy. In our opinion, CTE is the ideal tool for evaluation of IMP as it not only locates the affected veins, but also helps assess the severity of the lesions. According to our findings, Chinese medicines may be involved in the etiology of IMP. Therefore, it is recommended that long-term use of Chinese herbs and medical liquor should be avoided. However, further study is required to explore the pathogenesis of IMP and the relationship between IMP and colonic cancer.
Two patients both had a history of drinking Chinese medical liquor and presented with recurrent ileus.
In Case 1, physical examination revealed no abnormality while in Case 2, there was a lack of bowel movement and flatulence.
Inflammatory bowel disease, tuberculosis of intestines, and colonic cancer.
Thread-like calcifications in the mesenteric veins on computed tomography associated with purple-blue mucosa on colonoscopy.
Vascular proliferation in the mesentery and sub-mucosa and serosa layers of the intestinal wall. The vascular walls were thickened, with obvious calcification, while collagen deposition and hyaline degeneration could be seen.
The patients were asked to discontinue the use of medical liquor; conservative treatment or surgery was chosen according to the severity of the disease.
The etiology of this disease is not clear and region-specific lifestyle, portal vein hypertension as well as alcohol consumption have also been considered
Acanthopanax gracilistylus wine: it’s a kind of wine sold in China which has multiple Chinese herbs soaked in alcohol such as geniposide, Angelica sinensis and Cortex Acanthopanacis.
It is therefore recommended to avoid long-term use of Chinese herbs as well as medical liquor and computed tomography enterography is the ideal tool for evaluation as it not only locates the affected veins, but also helps evaluating the severity of the lesions.
This is an interesting report on a relatively rare disease and it may contribute to the knowledge of etiology of this disease.
P- Reviewers: Castro FJ, Cho YS, Pescatori M, Limdi JK, Yen HH S- Editor: Gou SX L- Editor: A E- Editor: Ma S
| 1. | Koyama N, Koyama H, Hanajima T, Matsubara N, Fujisaki J, Shimoda T. Chronic ischemic colitis causing stenosis: report of a case. Stomach Intestine. 1991;26:455-460. |
| 2. | Yao T, Iwashita A, Hoashi T, Matsui T, Sakurai T, Arima S, Ono H, Schlemper RJ. Phlebosclerotic colitis: value of radiography in diagnosis--report of three cases. Radiology. 2000;214:188-192. [PubMed] |
| 3. | Iwashita A, Yao T, Schlemper RJ, Kuwano Y, Yao T, Iida M, Matsumoto T, Kikuchi M. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003;46:209-220. [PubMed] |
| 4. | Hu P, Deng L. Phlebosclerotic colitis: three cases and literature review. Abdom Imaging. 2013;38:1220-1224. [PubMed] |
| 5. | Kang HY, Noh R, Kim SM, Shin HD, Yun SY, Song IH. Phlebosclerotic colitis in a cirrhotic patient with portal hypertension: the first case in Korea. J Korean Med Sci. 2009;24:1195-1199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Jung HG, Koh JW, Lee MY. [A case of idiopathic mesenteric phlebosclerosis]. Korean J Gastroenterol. 2008;52:261-264. [PubMed] |
| 7. | Markos V, Kelly S, Yee WC, Davis JE, Cheifetz RE, Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am J Roentgenol. 2005;184:1584-1586. [PubMed] |
| 8. | Chang KM. New histologic findings in idiopathic mesenteric phlebosclerosis: clues to its pathogenesis and etiology--probably ingested toxic agent-related. J Chin Med Assoc. 2007;70:227-235. [PubMed] |
| 9. | Hozumi H, Hokari R, Shimizu M, Maruta K, Narimatsu K, Sato H, Sato S, Ueda T, Higashiyama M, Watanabe C. Phlebosclerotic colitis that was difficult to distinguish from collagenous colitis. Dig Endosc. 2013;Jul 31; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kato T, Miyazaki K, Nakamura T, Tan KY, Chiba T, Konishi F. Perforated phlebosclerotic colitis--description of a case and review of this condition. Colorectal Dis. 2010;12:149-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Kitamura T, Kubo M, Nakanishi T, Fushimi H, Yoshikawa K, Taenaka N, Furukawa T, Tsujimura T, Kameyama M. Phlebosclerosis of the colon with positive anti-centromere antibody. Intern Med. 1999;38:416-421. [PubMed] |
| 12. | Oshitani N, Matsumura Y, Kono M, Tamori A, Higuchi K, Matsumoto T, Seki S, Arakawa T. Asymptomatic chronic intestinal ischemia caused by idiopathic phlebosclerosis of mesenteric vein. Dig Dis Sci. 2002;47:2711-2714. [PubMed] |
| 13. | Hiramatsu K, Sakata H, Horita Y, Orita N, Kida A, Mizukami A, Miyazawa M, Hirai S, Shimatani A, Matsuda K. Mesenteric phlebosclerosis associated with long-term oral intake of geniposide, an ingredient of herbal medicine. Aliment Pharmacol Ther. 2012;36:575-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Kimura Y, Kashima K, Daa T, Tou Y, Hanzawa K, Nakayama I, Yokoyama S. Phlebosclerotic colitis coincident with carcinoma in adenoma. Pathol Int. 2003;53:721-725. [PubMed] |
| 15. | Kusanagi M, Matsui O, Kawashima H, Gabata T, Ida M, Abo H, Isse K. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am J Roentgenol. 2005;185:441-447. [PubMed] |
| 16. | Miyazaki M, Nakamura S, Matsumoto T. Idiopathic mesenteric phlebosclerosis occurring in a wife and her husband. Clin Gastroenterol Hepatol. 2009;7:e32-e33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Nomura K, Kikuchi D, Iizuka T, Yamada A, Furuhata T, Domon K, Yamashita S, Nakamura M, Matsui A, Mitani T. [Idiopathic mesenteric phlebosclerosis associated with long-term use of Chinese herbs: a case report]. Nihon Shokakibyo Gakkai Zasshi. 2012;109:1567-1574. [PubMed] |
| 18. | Wang HH, Wu YC, Liu CH, Chen YL, Huang GS, Chang WC. Mesenteric phlebosclerosis: an unexpected cause of abdominal pain. J Gastrointestin Liver Dis. 2012;21:344. [PubMed] |
| 19. | Nishiura H, Nakase H, Chiba T. Sustained abdominal discomfort in a 57-year-old woman. Idiopathic mesenteric phlebosclerosis. Gut. 2010;59:578, 594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |