Published online Apr 7, 2014. doi: 10.3748/wjg.v20.i13.3712
Revised: February 12, 2014
Accepted: March 6, 2014
Published online: April 7, 2014
Processing time: 140 Days and 19.6 Hours
Hemobilia accounts for approximately 3% of all major percutaneous liver biopsy complications, and rarely results from arterioportal fistula. We report a patient who suffered from four complications over 11 d after ultrasound-guided percutaneous liver biopsy: hemobilia, acute pancreatitis, acute cholecystitis, and multiple stomach ulcers. Digital subtraction angiography was done after consultation with doctors, and showed obvious arteriovenous fistula of the right liver. The hepatic artery was selected and embolized by spring orbs. The active bleeding was stopped after embolization of the hepatic artery. The patient was discharged home on day 12 after embolization and remained well.
Core tip: We report a patient who suffered from four complications over 11 d after ultrasound-guided percutaneous liver biopsy: hemobilia, acute pancreatitis, acute cholecystitis, and multiple stomach ulcers. Digital subtraction angiography was done after consultation with doctors, and showed obvious arteriovenous fistula of the right liver. The hepatic artery was selected and embolized by spring orbs. The active bleeding was stopped after embolization of the hepatic artery.
- Citation: Zhou HB. Hemobilia and other complications caused by percutaneous ultrasound-guided liver biopsy. World J Gastroenterol 2014; 20(13): 3712-3715
- URL: https://www.wjgnet.com/1007-9327/full/v20/i13/3712.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i13.3712
Percutaneous ultrasound-guided liver biopsy is a common practice in the differential diagnosis and treatment of chronic liver disease. The rates of major complications and mortality are 2%-4% and 0.01%-0.33%, respectively. Arterioportal fistula as a complication of percutaneous liver biopsy is infrequently seen and normally asymptomatic. Hemobilia accounts for approximately 3% of overall major percutaneous liver biopsy complications, and rarely results from arterioportal fistula. We report a patient who suffered from four complications over 11 d after ultrasound-guided percutaneous liver biopsy: hemobilia, acute pancreatitis, acute cholecystitis, and multiple stomach ulcers.
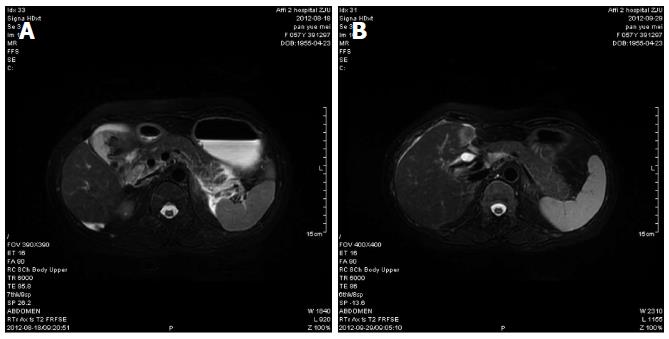
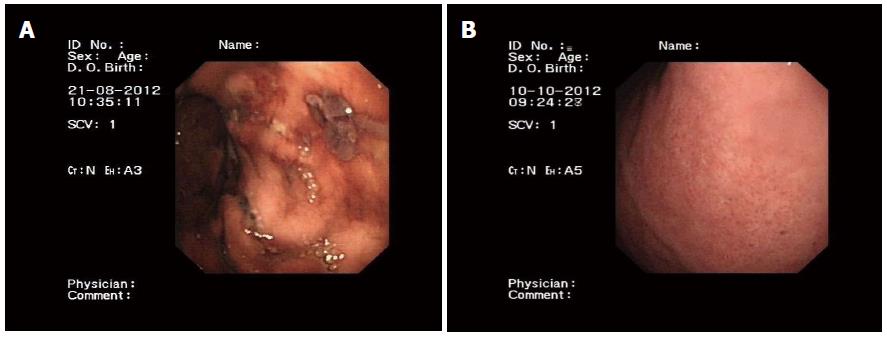
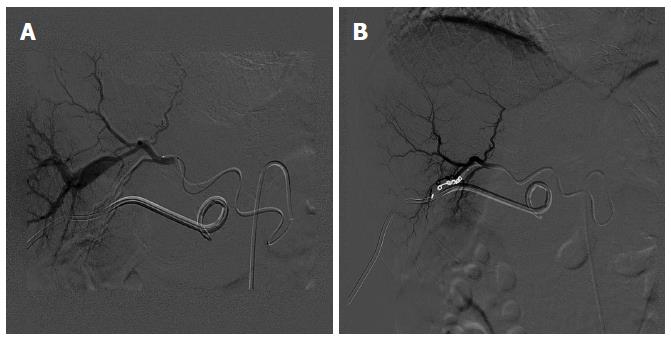
A 57-year-old woman underwent ultrasound-guided liver biopsy because of abnormal liver function for 4 years. She experienced acute epigastric pain and melena without hematemesis 7 d after the procedure. Type-B ultrasound showed cholecystitis, cholangitis, and siltation of biliary mud in the gallbladder. Enhanced computed tomography showed cholangitis, cholecystolithiasis, high-density reflection in the common bile duct, and mild cholangiectasis. After antibiotics, proton pump inhibitors and analgesics, the patient had no obvious improvement and had severe abdominal pain, hematemesis, and bloody stools. After fasting, gastrointestinal decompression and fluid replacement, the patient was hospitalized. In the following days, she developed worsening right epigastric pain and 1500 mL red bloody stools. Her hemoglobin level decreased from 134 to 73 g/L (normal range: 113-151 g/L). Serum amylase was 614 U/L (normal range: 22-80 U/L), and total bilirubin was 65 mg/dL (normal range: 0.1-1.2 mg/dL). Ultrasound examination demonstrated enlargement of the gallbladder and the possibility of empyema. There was a low echo-level mass (hematocele) in the common bile duct, and distension of the pancreatic duct. Magnetic resonance cholangiopancreatography (MRCP) revealed pancreatitis, cholecystolithiasis, cholecystitis, cholangiectasis, and abnormal signals indicating muddy stone or hematocele in the common bile duct and hepatic duct (Figure 1). The gastroscope showed multiple gastric ulcers and bleeding duodenal papilla (Figure 2). The epigastric pain was decreased after percutaneous ultrasound, which was guided by the tube drainage of the tumescent gallbladder. About 100-250 mL of red bile was drained within 1 d. Her hemoglobin level decreased to 52 g/L after 4 d in hospital. She received 4 U packed red blood cells. Digital subtraction angiography (DSA) was performed, which showed obvious arteriovenous fistula of the right liver. The hepatic artery was selected and embolized by spring orbs. The active bleeding was stopped after embolization of the hepatic artery. The patient was discharged home on day 12 after embolization and remained well. After 2 mo, her hemoglobin level increased to 140 g/L. Serum amylase was 68 U/L, and total bilirubin was 0.75 mg/dL. MRCP showed little exudation in the gallbladder fossa and the bile ducts in the left liver were thickened. Gastroscopy revealed chronic superficial gastritis (Figure 3).
Hemobilia is often considered to occur in liver injury and after calculus removal from the bile duct. With the application of traumatic examination of the liver and endoscopic technology, the traumatic intrahepatic biliary bleeding that is induced by iatrogenic trauma such as percutaneous transhepatic cholangial drainage has gradually increased[1]. Traumatic intrahepatic biliary bleeding may not occur during the procedure, but possibly a few days later. One needs to be extra vigilant in the clinic. Due to the close relationship of the intrahepatic bile duct and hepatic artery and portal vein, a puncture needle can easily injury all of these structures to form arteriovenous fistula, arterial bile duct fistula, and venous bile duct fistula. Venous bile duct fistula bleeding can often stop spontaneously because of the low venous pressure. When patients have biliary obstruction and infection, the hepatic arterial blood flow increases, and hyperplasia and distention of the arterial peribiliary vascular plexus and the branch of the hepatic artery in periportal areas can lead to bile duct fistula hemorrhage. This is the pathological basis of biliary bleeding. Blood clots formed in the bile duct can cause obstructive jaundice, leading to acute cholangitis and acute pancreatitis[2,3]. The present case had a tumescent gallbladder because of a hematocele. A blood clot in the biliary tract could have caused the increased pressure. That could have provoked acute pancreatitis and increasing hemodiastase. Pancreatitis caused by hemobilia and increased pressure can be improved by reducing the biliary tract pressure. Patients with hemobilia and increased pressure in the biliary tract should undergo puncture gallbladder to reduce pressure. This could strive the time of treatment. Reducing the biliary tract pressure can prevent pancreatitis.
In the present case, traumatic arteriovenous fistula of the liver was detected by DSA. Lim et al[4] have reported that percutaneous liver biopsy can lead to liver arteriovenous fistula. Lee et al[5] reported that arteriovenous fistula formed in 38% (8/21) of cases after liver biopsy. Arteriovenous fistula bleeding in the liver often results from intrahepatic hematoma and portal hypertension. Although DSA did not directly show arteriobiliary fistula, and the contrast agent was not obviously leaking into the bile, traumatic arteriovenous fistula guided us to find the possible bleeding artery. In our case, selective arterial embolization was performed and gastrointestinal bleeding stopped. Usually, the best opportunity for DSA is acute sustained bleeding with at a rate > 0.5 mL/min. Tillotson et al[6] have suggested that patients with unexplained gastrointestinal bleeding should receive immediate access to DSA and interventional treatment. Interventional treatment includes arterial embolization and drug infusion. Embolic materials often used are gelatin sponge, autoallergy-sludged blood, spring orb and polyvinyl alcohol particles. Hypophysin is also commonly used. Several studies have suggested that superselective embolization is a safer and more effective treatment for active bleeding, but it is not a substitute for emergency surgery[7,8]. In patients with hematemesis and/or melena, right upper quadrant pain, and iatrogenic jaundice occurring after invasive surgery of the liver, care is needed to guard against the presence of tardive hemobilia. It is important to request the correlated case history. It is necessary to perform DSA and give interventional treatment when the treatment of gastrointestinal tract hemorrhage is ineffective.
The patient experienced acute epigastric pain and red bloody stools after ultrasound-guided liver biopsy.
We report a rare case of a 57-year-old woman who suffered from four complications over 11 d after ultrasound-guided percutaneous liver biopsy: hemobilia, acute pancreatitis, acute cholecystitis, and multiple stomach ulcers.
Acute epigastric pain and red bloody stools hinted at differential diagnosis between hemobilia and bleeding peptic ulcer.
Serological testing revealed anemia, hyperamylasemia and hyperbilirubinemia.
Magnetic resonance cholangiopancreatography (MRCP) revealed pancreatitis, cholecystolithiasis, cholecystitis, cholangiectasis, and digital subtraction angiography (DSA) showed obvious arteriovenous fistula of the right liver.
The hepatic artery was selected and embolized by spring orbs.
MRCP is an evolving technique for noninvasive imaging of diseases of the biliary tree and pancreatic duct. DSA is a widely used fluoroscopy technique for vascular imaging, which produces a sequence of projection X-ray images of blood vessels that is used in diagnosis and treatment.
The author reports a rare case of a patient who suffered from four complications over 11 d after ultrasound-guided percutaneous liver biopsy. This rare clinical condition has seldom been reported in the literature.
In this manuscript, the author reported an interesting case of a patient who suffered from four complications over 11 d after ultrasound-guided percutaneous liver biopsy. This case is rare and seldom reported in the literature.
P- Reviewers: Casciaro S, Markic D, Streba CT S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
| 1. | Oh HC, Lee SK, Lee TY, Kwon S, Lee SS, Seo DW, Kim MH. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 108] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Edden Y, St Hilaire H, Benkov K, Harris MT. Percutaneous liver biopsy complicated by hemobilia-associated acute cholecystitis. World J Gastroenterol. 2006;12:4435-4436. [PubMed] |
| 3. | Albuquerque W, Arantes V, de Paula Farah K, Lambertucci JR. Acute pancreatitis and acute cholecystitis caused by hemobilia after percutaneous ultrasound-guided liver biopsy. Endoscopy. 2005;37:1159-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Lim JH, Lee SJ, Lee WJ, Lim HK, Choo SW, Choo IW. Iodized oil retention due to postbiopsy arterioportal shunt: a false positive lesion in the investigation of hepatocellular carcinoma. Abdom Imaging. 1999;24:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Lee SJ, Lim JH, Lee WJ, Lim HK, Choo SW, Choo IW. Transient subsegmental hepatic parenchymal enhancement on dynamic CT: a sign of postbiopsy arterioportal shunt. J Comput Assist Tomogr. 1997;21:355-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Tillotson CL, Geller SC, Kantrowitz L, Eckstein MR, Waltman AC, Athanasoulis CA. Small bowel hemorrhage: angiographic localization and intervention. Gastrointest Radiol. 1988;13:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Burgess AN, Evans PM. Lower gastrointestinal haemorrhage and superselective angiographic embolization. ANZ J Surg. 2004;74:635-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Horiguchi J, Naito A, Fukuda H, Nakashige A, Ito K, Kiso T, Mori M. Morphologic and histopathologic changes in the bowel after super-selective transcatheter embolization for focal lower gastrointestinal hemorrhage. Acta Radiol. 2003;44:334-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |