Published online Mar 14, 2014. doi: 10.3748/wjg.v20.i10.2721
Revised: November 1, 2013
Accepted: November 28, 2013
Published online: March 14, 2014
Processing time: 158 Days and 20.9 Hours
We present a case of afferent loop syndrome (ALS) occurring after pancreaticoduodenectomy (PD) in a patient who had previously undergone total gastrectomy (TG), and review the English-language literature concerning reconstruction procedures following PD in patients who had undergone TG. The patient was a 69-year-old man who had undergone TG reconstruction by a Roux-en-Y method at age 58 years. The patient underwent PD for pancreas head adenocarcinoma. A jejunal limb previously made at the prior TG was used for pancreaticojejunostomy and hepaticojejunostomy. Despite normal patency of the hepaticojejunostomy, he suffered from repeated postoperative cholangitis which was brought on by ALS due to shortness of the jejunal limb (15 cm in length). We therefore performed receliotomy in which the hepaticojejunostomy was disconnected and reconstructed using a new Y limb 40-cm in length constructed in a double Roux-en-Y fashion. The refractory cholangitis resolved immediately after the receliotomy and did not recur. Review of the literature revealed the lack of any current consensus for a standard procedure for reconstruction following PD in patients who had previously undergone TG. This issue warrants further attention, particularly given the expected future increase in the number of PDs in patients with a history of gastric cancer.
Core tip: We present a case of afferent loop syndrome occurring after pancreaticoduodenectomy (PD) in a patient who had previously undergone total gastrectomy, and review the English-language literature concerning reconstruction procedures following PD in patients who had undergone total gastrectomy (TG). Review of the literature revealed the lack of any current consensus for a standard procedure for reconstruction following PD in patients who had previously undergone TG. This issue warrants further attention, particularly given the expected future increase in the number of PDs in patients with a history of gastric cancer.
- Citation: Yokoyama S, Sekioka A, Ueno K, Higashide Y, Okishio Y, Kawaguchi N, Hagihara T, Yamada H, Kamimura R, Kuwahara M, Ichimiya M, Utsunomiya H, Uyama S, Kato H. Pancreaticoduodenectomy following total gastrectomy: A case report and literature review. World J Gastroenterol 2014; 20(10): 2721-2724
- URL: https://www.wjgnet.com/1007-9327/full/v20/i10/2721.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i10.2721
There is no general consensus regarding the method of reconstruction following pancreaticoduodenectomy (PD) in patients who have undergone total gastrectomy (TG). Here, we present a case of afferent loop syndrome (ALS) occurring after PD in a patient who previously underwent TG. The ALS was considered to be due to shortness of the jejunal limb used for hepatico- and pancreatico-jejunostomy and was resolved by revision of the hepaticojejunostomy using a newly-made jejunal limb with sufficient length. In this paper, we detail the postoperative course of this patient, and review the English-language literature concerning methods of reconstruction following PD in patients who have undergone TG.
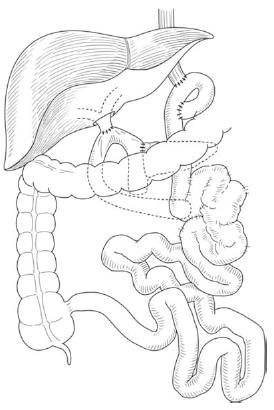
The patient was a 69-year-old man who had undergone TG for gastric cancer which was reconstructed by the Roux-en-Y method at the age of 58. The patient underwent PD for adenocarcinoma of the pancreas head. The surgery was uneventful. We used the jejunal limb made at the previous TG for pancreaticojejunostomy and hepaticojejunostomy. As a result, the length of the afferent loop was only 15-20 cm (Figure 1).
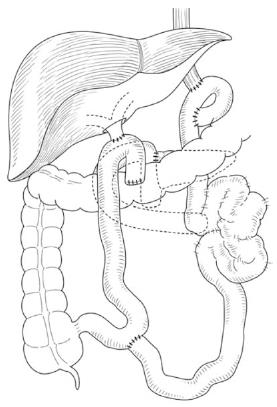
Although the immediate postoperative course was uneventful, the patient suffered from repeated episodes of cholangitis from 14 d after surgery. This was in spite of normal patency of the hepaticojejunostomy, as confirmed by cholangiography via an external biliary stent tube. Based on the findings of an upper gastrointestinal study, which revealed reflux of contrast medium into the biliary tree through the hepaticojejunostomy, ALS was diagnosed. Because the ALS was considered to be due to shortness of the jejunal limb, we performed receliotomy, in which the hepaticojejunostomy was disconnected and reconstructed using a new Y limb 40-cm in length in a double Roux-en-Y fashion 6 wk after the previous surgery (Figure 2). Following receliotomy, no further episodes of cholangitis were observed. The patient was discharged from hospital 4 wk after the receliotomy and remains well without symptoms at 6 mo after receliotomy.
A PubMed search on July 2013 for articles published since 1965 with the key words “pancreaticoduodenectomy” and “following total gastrectomy” yielded 18 articles in the English-language literature. These publications were all reviewed. Only four papers describing five cases of PD following TG were found, which together with our present case results in a total of six reported cases[1-5] (Table 1). Previous TG was performed for gastric cancer in all six cases. The reconstruction method used following TG was Roux-en-Y in five cases and Billroth II in one. The interval between TG and PD ranged from 15 to 132 mo, with a median of 56 mo. PD was performed for pancreatic adenocarcinoma in four cases, pancreatic gastrinoma in one, and distal bile duct carcinoma in one. Of these six, a jejunal limb already constructed in the previous TG was used for pancreatic and biliary reconstruction in three cases (including our own case). In the other three cases, a newly-made jejunal limb was used for pancreatic and biliary reconstruction in a Roux-en-Y fashion. ALS was observed in two of the three cases in which a jejunal limb made in a previous TG was used for pancreatic and biliary reconstruction.
| No. | Gastrectomy | Pancreaticoduodenectomy | Ref. | ||||||||
| Age | Indication | Type of Gastrectomy | Anastomosis | Age | Interval (mo) | Indication | Reconstruction | Operative time (min) | Complication | ||
| 1 | 65 | Gastric cancer | Total | Roux-en-Y | 69 | 43 | Pancreatic cancer | Roux-en-Y2 | 509 | Afferent loop syndrome | [1] |
| 2 | 45 | Gastric ulcer | Total | Roux-en-Y | 46 | 15 | Pancreatic Gastrinoma | New- | 503 | None | [2] |
| Roux-en-Y | |||||||||||
| 3 | 61 | Gastric cancer | Total1 | Roux-en-Y | 71 | 120 | Pancreatic cancer | New- | N/A | Pancreatic fistula | [3] |
| Roux-en-Y | |||||||||||
| 4 | 64 | Gastric cancer | Total | Roux-en-Y | 68 | 48 | Bile duct cancer | Roux-en-Y2 | 445 | None | [4] |
| 5 | 58 | Gastric cancer | Total | Roux-en-Y | 69 | 124 | Pancreatic cancer | Roux-en-Y2 | 568 | Afferent loop syndrome | Our case |
| 6 | 36 | Gastric cancer | Total | Billroth-II | 56 | 56 | Pancreatic cancer | New- | 672 | None | [5] |
| Roux-en-Y | |||||||||||
Pancreaticoduodenectomy in patients with a history of major abdominal surgery is a challenging task. Notably, PD in patients with previous TG is difficult, and can be limited by adhesions and anatomical complexity around the pancreas subsequent to the previous TG procedure. In our patient, we performed PD with resection of the duodenal part of a previous afferent loop, and used the remaining part of the afferent loop for pancreatico- and hepaticojejunostomy. We applied this procedure to reduce the number of intestinal anastomoses. As a result, however, the jejunal limb used was markedly short, resulting in the development of refractory cholangitis due to ALS.
There is no consensus regarding the standard procedure for reconstruction following PD for patients with previous TG. Furthermore, our patient was seriously affected by a resultant mistake in choosing a reconstruction procedure following PD. We therefore conducted a review of the literature, with a focus on reconstruction procedures following PD in patents who had previously undergone TG. This review demonstrated that it is difficult to state that usage of a jejunal limb previously made at a prior TG should be avoided, as only a few cases of PD in patients with previous TG have been reported, although ALS, which is reportedly rare after PD[2], was observed in two of three cases where an already-made jejunal limb was used for pancreatic and biliary reconstruction. In contrast, ALS was not observed in any of the other three cases in which a jejunal limb for reconstruction was newly made. Furthermore, ALS in our patient was remedied by receliotomy, in which the hepaticojejunostomy was disconnected and reconstructed using a new Y limb 40-cm in length, which was constructed in a double Roux-en-Y fashion. We therefore consider that jejunal limbs should be reconstructed following PD in patients with previous TG in which the jejunal limb is markedly short.
Because the outcomes of treatment for gastric cancer, for which gastrectomy is most commonly performed, have improved, the number of PD procedures in patients with previous gastrectomy is expected to increase[6,7]. We hope that high-volume centres will conduct studies of sufficient size to allow the establishment of a standard reconstruction procedure for this condition.
Although the early postoperative course was uneventful, the patient suffered from repeated episodes of cholangitis from 14 d after surgery.
A case of afferent loop syndrome (ALS) occurring after pancreaticoduodenectomy (PD) in a patient who had previously undergone total gastrectomy (TG).
Based on the findings of an upper gastrointestinal study, which revealed reflux of contrast medium into the biliary tree through the hepaticojejunostomy, ALS was diagnosed.
Because ALS was considered to be due to shortness of the jejunal limb, we performed receliotomy, in which the hepaticojejunostomy was disconnected and reconstructed using a new Y limb 40 cm in length in a double Roux-en-Y fashion 6 wk after the previous surgery.
Only four papers describing five cases of pancreaticoduodenectomy following total gastrectomy were found, which together with the present case results in a total of six reported cases.
This study demonstrates that jejunal limbs should be reconstructed following PD in patients with previous TG in which the jejunal limb is markedly short.
The high-volume centres will conduct studies of sufficient size to allow the establishment of a standard reconstruction procedure for PD following TG.
P- Reviewers: Klinge U, Smyrniotis V S- Editor: Qi Y L- Editor: Webster JR E- Editor: Liu XM
| 1. | Aimoto T, Uchida E, Nakamura Y, Katsuno A, Chou K, Tajiri T, Naito Z. Malignant afferent loop obstruction following pancreaticoduodenectomy: report of two cases. J Nippon Med Sch. 2006;73:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Doi R, Fujimoto K, Imamura M. Effects of preceding gastrectomy on the outcome of pancreatoduodenectomy. J Gastrointest Surg. 2004;8:575-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Noguchi K, Okada K, Kawamura H, Ishizu H, Homma S, Kataoka A. Operative procedure for pancreatoduodenectomy in a patient who had previously undergone total gastrectomy, distal pancreatectomy, and splenectomy. Am Surg. 2012;78:103-105. [PubMed] |
| 4. | Oida T, Kano H, Mimatsu K, Kawasaki A, Kuboi Y, Fukino N, Kida K, Amano S. Jejunal scarf-covering method in pancreaticojejunostomy after total gastrectomy. Case Rep Gastroenterol. 2012;6:472-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Mizuno S, Isaji S, Ohsawa I, Kishiwada M, Hamada T, Usui M, Sakurai H, Tabata M. Pancreaticoduodenectomy with resection of the splenic artery and splenectomy for pancreatic double cancers after total gastrectomy. Preservation of the pancreatic function via the blood supply from the posterior epiploic artery: report of a case. Surg Today. 2012;42:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Sasako M. Gastric cancer eastern experience. Surg Oncol Clin N Am. 2012;21:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Rausei S, Dionigi G, Sano T, Sasako M, Biondi A, Morgagni P, Garofalo A, Boni L, Frattini F, D’Ugo D. Updates on surgical management of advanced gastric cancer: new evidence and trends. Insights from the First International Course on Upper Gastrointestinal Surgery--Varese (Italy), December 2, 2011. Ann Surg Oncol. 2013;20:3942-3947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |