Published online Jan 7, 2014. doi: 10.3748/wjg.v20.i1.258
Revised: October 10, 2013
Accepted: October 17, 2013
Published online: January 7, 2014
Processing time: 161 Days and 21.1 Hours
AIM: To investigate the feasibility and clinical application of transumbilical single-incision endoscopic splenectomy using conventional laparoscopic instruments.
METHODS: Between 2010 and 2012, transumbilical single-incision endoscopic splenectomy was performed in 10 patients in our department, of whom 4 had refractory idiopathic thrombocytopenic purpura, 4 had enlarged splenic cyst and 2 had splenic hematoma. A 2.5-cm curved incision was made at the lower umbilicus edge, and a 10 mm laparoscope was inserted into the middle of the incision. A 5-mm harmonic scalpel was placed on the right side, and a 5-mm auxiliary instrument on the left side of the laparoscope. Splenic ligaments were incised with a harmonic scalpel, and the splenic pedicle was cut with an Endo-gastrointestinal anastomosis. The spleen was dissected and placed in a large retrieval bag, blended, and then removed.
RESULTS: All transumbilical single-incision endoscopic splenectomies were performed successfully with mean operative time of 80 ± 5 min and mean blood loss of 150 ± 20 mL. Conversion to laparotomy or multi-port laparoscopic surgery was not required in all cases. All patients were discharged on postoperative days 4-6. During the postoperative hospitalization period, no painkillers were required. No intra-abdominal complications such as infection, ascites, gastric leakage, pancreatic leakage, or wound infection occurred in any case during the 6-mo follow-up.
CONCLUSION: Transumbilical single-incision endoscopic splenectomy using conventional laparoscopic instruments is technically feasible and safe in selected patients.
Core tip: Laparoscopic splenectomy has been recognized worldwide and has gradually replaced conventional laparotomy. It is the first choice of splenectomy for diseased spleens < 20 cm in diameter, especially for spleens with hematological diseases. Minimally invasive surgery has developed with the increasing demand for better cosmetic outcomes. For this reason, single-incision endoscopic techniques have emerged and become the latest research focus of minimally invasive surgery. In this report, we demonstrated our successful performance of transumbilical single-incision endoscopic cholecystectomy in 10 patients with benign lesions using conventional laparoscopic instruments.
- Citation: Liang ZW, Cheng Y, Jiang ZS, Liu HY, Gao Y, Pan MX. Transumbilical single-incision endoscopic splenectomy: Report of ten cases. World J Gastroenterol 2014; 20(1): 258-263
- URL: https://www.wjgnet.com/1007-9327/full/v20/i1/258.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i1.258
Since the first laparoscopic splenectomy was performed by Delaitre et al[1], this innovative technique has been recognized worldwide and has gradually replaced conventional laparotomy[2]. However, minimally invasive surgery has developed with the increasing demand for better cosmetic outcomes. For this reason, single-incision endoscopic surgery (SIES) has emerged and become the latest research focus of minimally invasive surgery. Ma et al[3] confirmed the feasibility of SIES in an animal model. Barbaros et al[4] and Targarona et al[5] each reported cases of transumbilical SIES, which ushered in its clinical application. In this report, we demonstrated our successful performance of SIES in 10 patients with benign lesions using conventional laparoscopic instruments. (Table 1)
| No. | Age | Sex | Cause | Blood loss (mL) | Specimen weight (g) | Time (min) | Transfer to OS or MLS | Complications |
| 1 | 16 | Male | Refractory ITP | 150 | 195 | 92 | No | No |
| 2 | 19 | Female | enlarged splenic cyst | 80 | 181 | 88 | No | No |
| 3 | 17 | Male | Refractory ITP | 210 | 223 | 90 | No | No |
| 4 | 17 | Male | Refractory ITP | 190 | 230 | 81 | No | No |
| 5 | 19 | Female | Splenic hematoma | 120 | 215 | 80 | No | No |
| 6 | 13 | Male | Enlarged splenic cyst | 130 | 185 | 84 | No | No |
| 7 | 14 | Female | Refractory ITP | 120 | 212 | 90 | No | No |
| 8 | 15 | Male | Enlarged splenic cyst | 190 | 225 | 86 | No | No |
| 9 | 14 | Male | Splenic hematoma | 180 | 210 | 85 | No | No |
| 10 | 16 | Female | Refractory ITP | 160 | 190 | 84 | No | No |
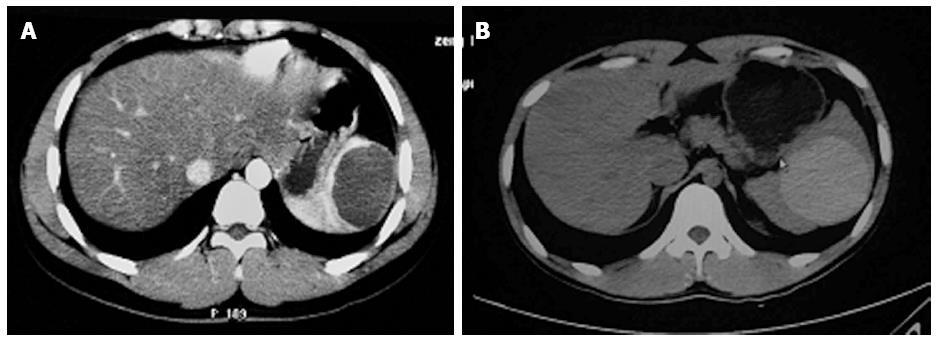
In this retrospective study, we included the patients who underwent SIES in our department between June 2010 and February 2012. Patient inclusion criteria were: (1) refractory ITP; (2) splenic cyst or hematoma diagnosed by computed tomography scan (Figure 1); (3) no symptoms of hemorrhagic shock; (4) no significant complications in other organs or systems; and (5) no contraindications for laparoscopy.
Major surgical equipment included: (1) a 10 mm 30° laparoscope and matching acquisition system (Olympus, Japan); (2) a linear cutting stapler (Ethicon60 Endo-Surgery, United States) and matching stapler reloads (ECR60W, stapler length 60 mm, 2.5 mm); (3) a 5-mm harmonic scalpel (Johnson and Johnson, United States); (4) ordinary laparoscopic instruments (5 mm and 12 mm trocars, separating pliers, atraumatic grasping forceps, coagulation rods, and suction device); and (5) 5-mm and 10-mm titanium clamps and matching titanium clips (Hem-o-lock: Kangji Medical Appliance Co. Ltd. China). No purpose-built instruments for SIES, such as Tri-Port, R-Port, Gel-Port, flexible laparoscope and graspers with articulation, were used.
After induction of general anesthesia and endotracheal intubation, the patients were placed in a 30° right lateral supine position with the head slightly tilted and the legs apart. The operating surgeon stood between the parted legs, while the camera operator stood at the patient’s right side. A 2.5-cm curved incision penetrating only the skin was made along the lower border of the umbilicus, and then a Veress needle was punctured through the peritoneum to establish pneumoperitoneum and the pressure was maintained at 14 mmHg.
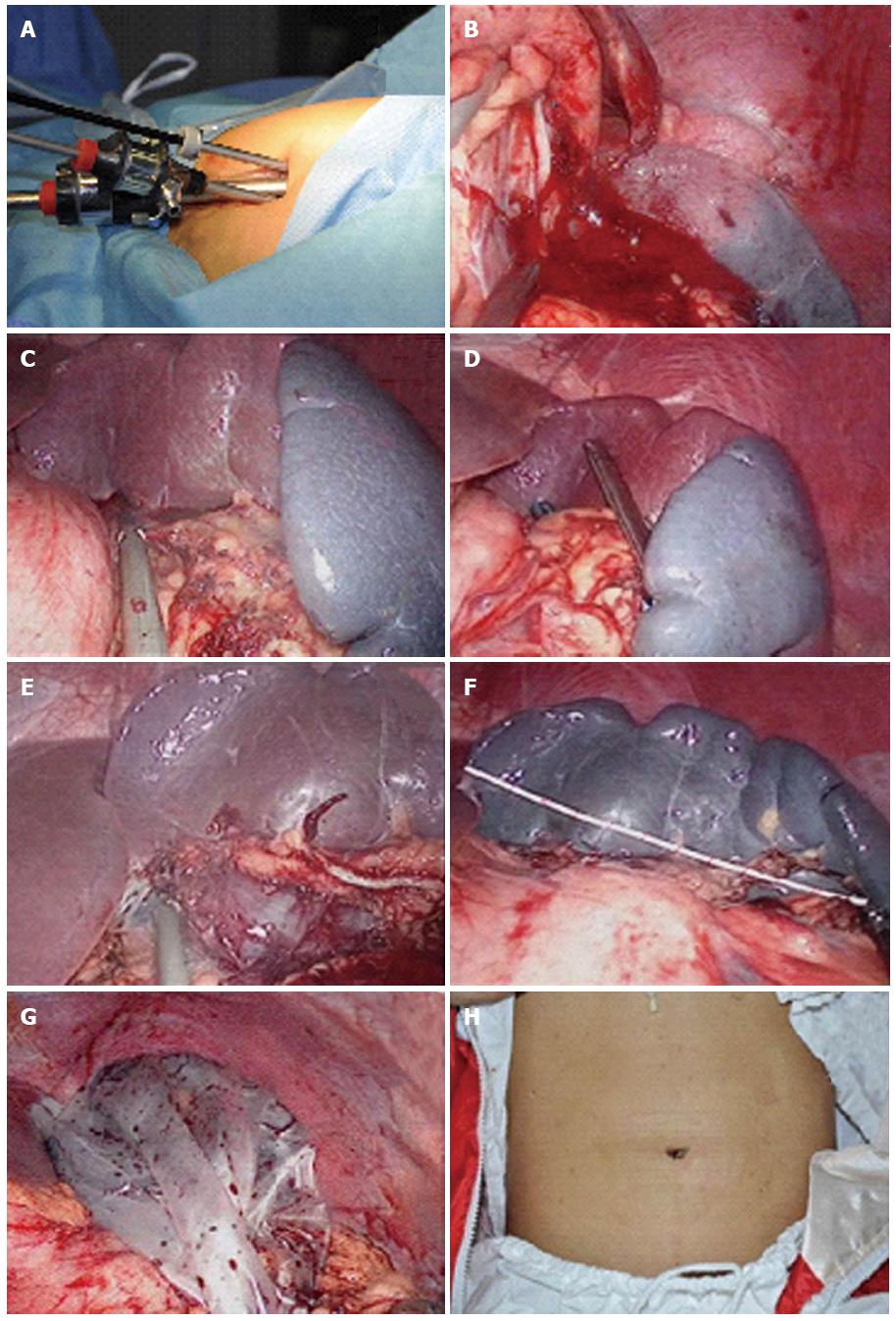
A 10-mm trocar was inserted in the middle of the incision and a 30° 10 mm laparoscope was inserted. Two 5-mm trocars were placed to both sides of the laparoscope and used to insert a grasper and a 5-mm ultrasound scalpel. The 3 trocars were arranged in an inverted triangle shape, and a small amount of muscle and fascia was kept between each port to prevent the leakage (Figure 2).
Next, the splenocolic, splenorenal, splenophrenic, and phrenicosplenic ligaments were all dissected with a harmonic scalpel. When approaching the splenic pedicle, one 5-mm trocar was exchanged for a 12-mm one to permit insertion of the endoscopic stapler to cut the splenic pedicle off (Figure 2). The spleen was dissected and placed in a retrieval bag, morcellated, and then removed through the operating port. The pneumoperitoneum was re-established and the surgical site examined for active bleeding. Once hemostasis was confirmed, an abdominal drainage tube was placed on the splenic bed through the operating port, all instruments were removed, the incision was sutured, and the drainage tube was fixed.
Transumbilical single-incision endoscopic splenectomies were accomplished successfully in all cases. The mean surgical time was 86 ± 5 min, and mean blood loss was 150 ± 20 mL. The mean weight of the resected spleens was 206 ± 16 g, as measured after being retracted from the abdomen. Conversion to laparotomy or conventional multi-port laparoscopic surgery was not required in all cases. All patients ambulated on the day of surgery, and the drainage tubes were removed on postoperative day (POD) 2. All 10 patients were discharged on PODs 4-6. During the hospitalization, no painkillers were required. No intra-abdominal infection, ascites, gastric leakage, pancreatic leakage, or wound infection or hematoma occurred in any case. At the follow-up 6 mo postoperatively, abdominal ultrasound examination did not reveal splenic venous thrombosis, splenic arteriovenous fistula, or ascites in the splenic fossa. Finally, the wounds healed without occurrence of hernia and the cosmetic result was excellent. (Figure 2)
In transumbilical SIES, the incision is hidden in the natural umbilical skin fold so that the postoperative scar is almost invisible. This surgical technique is therefore called a “no scar surgery”. It has advantages of less traumatic and better cosmetic outcomes than multi-port laparoscopy[6,7]. At present, SIES has been applied in all areas of abdominal surgery, including general surgery, hepatobiliary surgery, urology, and obstetrics and gynecology. Since August 2009, we have performed more than 500 cases of single-incision laparoscopic cholecystectomy and 15 cases of single-incision laparoscopic liver surgery, which has provided a solid foundation for the implementation of SIES. Because of the operating difficulties and high surgical risks, SIES remains in the preliminary exploration stage. Less than 50 cases of SIES have been completed worldwide to date, and most were reported as case reports[7-9].
We believe that the dissection of the splenic ligaments, especially the splenophrenic and phrenicosplenic ligaments, is fundamental to the success of the operation. Dissection of splenic ligaments in SIES is similar to that in conventional laparoscopy. The ligaments are normally dissected in the order of splenocolic, splenorenal, splenophrenic, and phrenicosplenic ligaments, although this order can be adjusted according to the actual intraoperative conditions. The splenophrenic ligament is very short, and the phrenicosplenic ligament is usually located at a higher position. In addition, the left lobe of the liver often covers these ligaments and because of the limited operating devices and mutual interference between devices, the exposure of splenophrenic and phrenicosplenic ligaments is very difficult. Srikanth et al[10] used a 2-0 polypropylene suture through the muscle of the fundus of the stomach for pulling the stomach from externally to expose the phrenicosplenic ligament. However, this suture may increase the risk of gastric perforation and its clinical value needs to be verified. In addition, the short gastric vessels run within the phrenicosplenic ligament, which are easily damaged by an inappropriate maneuver. During our surgical procedure for first patient, the phrenicosplenic ligament was over-stretched due to a lack of experience, which resulted in a slight tear of the ligament near the upper pole of the spleen (Figure 2). Although the bleeding was not severe and stopped with a titanium clamp, it still contaminated the operative field and caused certain troubles and risks for the subsequent procedures. This is the primary reason why the blood loss was greater and the operative time longer for the first case. In the other cases, we used atraumatic grasping forceps to hold the gastric end of the phrenicosplenic ligament and tilted the left lobe of the liver gently, and then incised the phrenicosplenic ligament near the splenic end with an ultrasonic scalpel. The results were satisfactory, and the damage to the stomach was effectively prevented.
A proper transection of the splenic pedicle is also the key to surgical success. There are many blood vessels within the splenic pedicle. If the pedicle is damaged, it is extremely difficult to stop bleeding and an emergency laparotomy is often required. Therefore, intraoperative exposure of the splenic pedicle is very important. As the spleen is easily damaged, pulling the spleen directly with a clamp to expose the splenic pedicle is clearly undesirable. Misawa et al[11] used a “tug-exposure technique” to expose the splenic pedicle, and have successfully performed 10 cases of SIES. We used a traumatic grasper to slowly probe from the lower pole to the bottom of the spleen, and then gently tilted the spleen upwards to expose the splenic pedicle. The entire procedure should be very gentle in order to avoid tearing the spleen or the pedicle. Currently, there are 2 primary ways available to incise the splenic pedicle. One is to use a linear cutting stapler to cut and ligate the pedicle, and the other is to use titanium or bio-absorbable clips to clamp the vessels or use a silk string to ligate the blood vessels, and then cut the splenic pedicle. The former method significantly simplifies the isolation and ligation of the splenic pedicle. We used this method in our cases (Figure 2), which did not encounter bleeding or complications.
Because the spleen is easily damaged and splenomegaly may be present, in order to easily place it into the specimen bag, we recommend first to change the operating table angle and the patient’s position (Figure 2) and subsequently, cut the tissues between the ports to make a single large port so that the specimen can be easily taken out. In our 10 patients, the spleens had major diameters of 12 to 14 cm (Figure 2) and because the lesions were benign, the specimens were removed after being blended. If malignancy is suspected, the specimen should be removed intact after the incision is appropriately extended.
SIES has some well-recognized advantages such as good cosmetic results, less pain, and faster recovery. However, it also has some drawbacks such as equipment crowding, mutual interference between devices, a linear perspective view due to the coaxial parallel between equipment and the endoscope, and therefore the lack of an “operation triangle”[12,13]. Recently, Monclova et al[8] concluded that reduced port splenectomy( RPAS) was a good alternative to traditional laparoscopic splenectomy and SIES. They thought that RPAS improved the cosmetic results as compared to laparoscopic splenectomy but reduced the technical challenges of SIES. However, we thought that SIES and RPAS will both be alternatives to conventional laparoscopic splenectomy in the future. As SIES has an amazing cosmetic result[14-16], we thought SIES will finally be a feasible technique with the improvement of surgical instruments and the accumulation of experience.
In summary, we believe that SIES will definitely take a certain position in splenic surgery with the improvement of equipment and technology. Large randomized controlled studies are required to confirm whether it can eventually replace conventional multi-port laparoscopy to become the gold standard for splenectomy.
Laparoscopic splenectomy has been recognized worldwide and has gradually replaced conventional laparotomy. However, minimally invasive surgery has developed with the increasing demand for better cosmetic outcomes. For this reason, single-incision endoscopic splenectomy (SIES), with advantages of less traumatic and better cosmetic outcomes than multi-port laparoscopy surgery, has emerged and become the latest research focus of minimally invasive surgery.
In transumbilical single-incision endoscopic splenectomy, the incision is hidden in the natural umbilical skin fold so that the postoperative scar is almost invisible. The research hotspot discussed here is that single-incision endoscopic splenectomy was feasible in selected patients and would finally be an alternative to multi-port splenectomy.
It should be the largest series of cases repot to explore the safety and efficacy of this innovative technique in the management of benign splenectomy diseases since the first case of single-incision endoscopic splenectomy was reported.
This study results suggest that transumbilical single-incision endoscopic splenectomy is technically feasible and safe using conventional laparoscopic instruments in selected patients.
SIES is a complementary approach to laparoscopic splenectomy, in which all operating procedures are completed through a single incision in the navel. However, unlike the traditional multi-port laparoscopic approach, laparo-endoscopic single-site surgery leaves only a single small scar.
This manuscript is focused in an interesting topic, the single-incision-splenectomy. The authors can talk about the feasibility and reproducibility of the technique.
P- Reviewers: Noguera JF, Puy RV S- Editor: Gou SX L- Editor: Wang TQ E- Editor: Wu HL
| 1. | Delaitre B, Maignien B. [Splenectomy by the laparoscopic approach. Report of a case]. Presse Med. 1999;20:2263. [PubMed] |
| 2. | Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, Lechner K, Rhodes M, Silecchia G, Szold A. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2008;22:821-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 193] [Article Influence: 11.4] [Reference Citation Analysis (1)] |
| 3. | Ma YZ, Zhu JF, Han QH, Wang YK. The experimental study of transumbilical laparoscopic splenectomy. Zhongguo Weichuang Waike Zazhi. 2009;9:3 Available from: http//www.cqvip.com/QK/84021X/200904/30161111.html. |
| 4. | Barbaros U, Dinççağ A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg. 2009;13:1520-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Targarona EM, Balague C, Martinez C, Pallares L, Estalella L, Trias M. Single-port access: a feasible alternative to conventional laparoscopic splenectomy. Surg Innov. 2009;16:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, He GL, Xu TC, Zhou CJ, Liu HY. Single-incision vs three-port laparoscopic cholecystectomy: prospective randomized study. World J Gastroenterol. 2013;19:394-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Pan M, Jiang Z, Cheng Y, Xu X, Zhang Z, Zhou C, He G, Xu T, Liu H, Gao Y. Single-incision laparoscopic hepatectomy for benign and malignant hepatopathy: initial experience in 8 Chinese patients. Surg Innov. 2012;19:446-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Monclova JL, Targarona EM, Vidal P, Peraza Y, Garcia F, Otero CR, Pallares L, Balague C, Trias M. Single incision versus reduced port splenectomy--searching for the best alternative to conventional laparoscopic splenectomy. Surg Endosc. 2013;27:895-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Targarona EM, Pallares JL, Balague C, Luppi CR, Marinello F, Hernández P, Martínez C, Trias M. Single incision approach for splenic diseases: a preliminary report on a series of 8 cases. Surg Endosc. 2010;24:2236-2240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Srikanth G, Wasim MD, Sajjad A, Shetty N. Single-incision laparoscopic splenectomy with innovative gastric traction suture. J Minim Access Surg. 2011;7:68-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Misawa T, Sakamoto T, Ito R, Shiba H, Gocho T, Wakiyama S, Ishida Y, Yanaga K. Single-incision laparoscopic splenectomy using the “tug-exposure technique” in adults: results of ten initial cases. Surg Endosc. 2011;25:3222-3227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Froghi F, Sodergren MH, Darzi A, Paraskeva P. Single-incision Laparoscopic Surgery (SILS) in general surgery: a review of current practice. Surg Laparosc Endosc Percutan Tech. 2010;20:191-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Best SL, Tracy CR, Cadeddu JA. Laparoendoscopic single-site surgery and natural orifice transluminal endoscopic surgery: future perspectives. BJU Int. 2010;106:941-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Hong TH, Lee SK, You YK, Kim JG. Single-port laparoscopic partial splenectomy: a case report. Surg Laparosc Endosc Percutan Tech. 2010;20:e164-e166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Rottman SJ, Podolsky ER, Kim E, Kern J, Curcillo PG. Single port access (SPA) splenectomy. JSLS. 2010;14:48-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Hansen EN, Muensterer OJ. Single incision laparoscopic splenectomy in a 5-year-old with hereditary spherocytosis. JSLS. 2010;14:286-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |