Published online Mar 7, 2013. doi: 10.3748/wjg.v19.i9.1494
Revised: January 13, 2013
Accepted: February 5, 2013
Published online: March 7, 2013
Processing time: 119 Days and 16.7 Hours
Intestinal hemolymphangioma is a rare vascular and lymphatic malformation and is manifested as anaemia and recurrent alimentary tract hemorrhage. Few cases of hemolymphangioma occurring in small intestine, spleen, esophagus and other organs have been reported. We herein report a case of a 37-year-old man with severe rectal bleeding. Digital examination revealed nodular mucosa. No rectal mass was palpated, but bleeding in the ampulla was detected. Colonoscopy revealed an extensive hypervascular submucosal lesion arising from the rectosigmoid junction colon to the distal edge of the anus. Endoscopic ultrasonography demonstrated an extensive anechoic mass with clear edge. Magnetic resonance imaging (MRI) showed a significant thickness of the rectal wall, extending to the distal edge of the anus, with a narrowing lumen. A sphincter-saving rectal surgery was performed. Due to a lack of knowledge of the clinical, endoscopic and radiological features, preoperative recognition of hemolymphangioma is not easy. Computed tomography and MRI are helpful in confirming the diagnosis, and defining the extent and invasion of the lesion. For the low malignant potential tumors, a sphincter-saving rectal surgery is recommended after a full evaluation of the tumor.
- Citation: Chen G, Cui W, Ji XQ, Du JF. Diffuse hemolymphangioma of the rectum: A report of a rare case. World J Gastroenterol 2013; 19(9): 1494-1497
- URL: https://www.wjgnet.com/1007-9327/full/v19/i9/1494.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i9.1494
Hemolymphangioma is very rare, and few cases occurring in the small intestine, spleen, esophagus, chest wall, mediastinum, adrenal gland have been reported[1-6]. Hemolymphangioma occurs predominately in young patients, especially in newborns and infants, and often arises from congenital malformation of vascular and lymphatic system. It is believed that hemolymphangioma is a benign disease without invasive ability. This report describes the first case of a diffuse hemolymphangioma of the rectum.
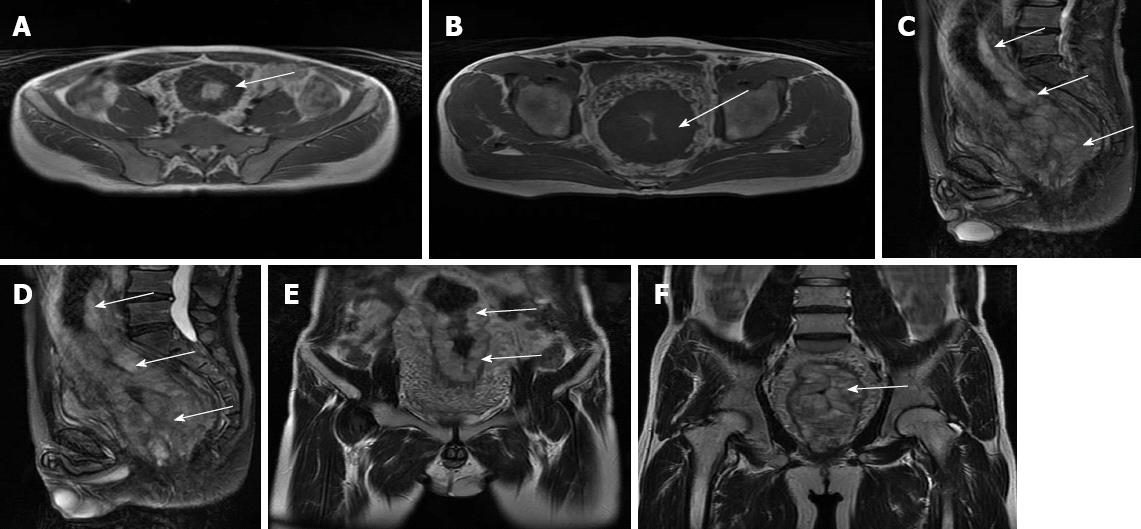
A 37-year-old man was admitted to a local hospital because of massive rectal bleeding in November 2010. He was managed with emergency care, such as blood transfusion. Upon admission, the patient’s hemoglobin was 69 g/L. He had no medical history of abdominal trauma or operation. His major symptoms were rectal bleeding and tenesmus. Because it was hard to distinguish the rectal lesions from haemorrhoids by digital examination, he started on conservative treatments such as local hemostasis. Due to recurrent bleeding, colonoscopy was performed, which showed an extensive hypervascular submucosal lesion arising from the rectosigmoid junction colon to the distal edge of the anus, and exhibiting tortuous submucosal veins and nodular mucosa. Biopsy was not performed to avoid the secondary severe hemorrhage. The endoscopic ultrasonography indicated an extensive anechoic mass with clear edge (Figure 1). He was transferred to our hospital with the diagnosis of a tumor at the rectum by computed tomography (CT) scan in December 2010. Physical examination revealed mild tenderness on the left lower quadrant. Rectal examination revealed nodular mucosa and red blood in the ampulla, but no obvious mass was found. No other abnormalities were found except for anemia shown in laboratory data including tumor markers such as carcino-embryonic antigen. Magnetic resonance imaging (MRI) showed significant a thickness of the rectal wall, extending to the distal edge of the anus, with a narrow lumen (Figure 2).
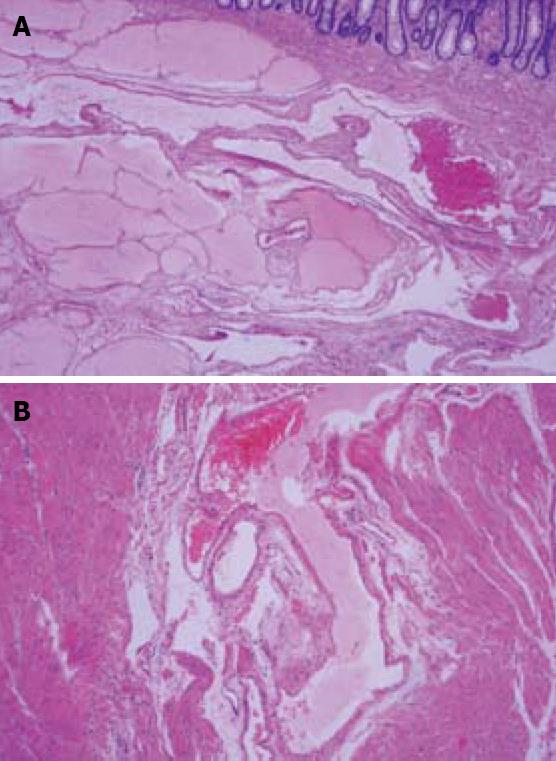
Based on the clinical and imaging evidence, preoperative diagnosis of the lesions was cavernous rectal haemangioma. Laparotomy showed diffuse colorectal proliferative lesions arising from sigmoid colon to anus with no ascites or peritoneal dissemination. A frozen-section examination of the rectal mass indicated a vascular tumor. Subsequently, a sphincter-saving procedure, i.e., low anterior resection of the rectosigmoid colon with hand-sewn transanal colo-anal anastomosis, was performed. The rectal mass weighed 840 g and measured 20 cm × 8 cm × 8 cm (Figures 3 and 4). Gross examination showed a cavernous, soft and compressible tumor. Microscopic examination revealed a tumor which was composed of blood and lymphatic vessels mainly located in submucosa, occupied the entire intestinal wall, and extended into the surrounding fatty tissues (Figure 5). The definitive histological diagnosis was hemolymphangioma of the rectum. No evidence of malignancy was found. The postoperative course was uneventful. The patient was discharged 12 d after surgery. After one year of follow-up, there were no complaints or signs of recurrence.
Hemolymphangioma is a very rare and benign tumor. Its incidence varies from 1.2 to 2.8 per 1000 newborns, and both genders are equally affected[1]. In a literature review until January 2013 (PubMed), no report of hemolymphangioma in the rectum has been published. The primary hemolymphangioma is considered a congenital malformation of the vascular system. The formation of this tumor may be explained by obstruction of the veno-lymphatic communication between dysembryoplastic vascular tissue and the systemic circulation[1]. Secondary hemolymphangioma is usually caused by the injury of lymphatic vessels in trauma or operation, which induces inadequate lymph fluid drainage. Hemolymphangioma often presents as a cystic or cavernous lesion. Microscopically, the tumor consists of abnormal blood and lymphatic vessels with polycystic spaces. These cysts have connective septa covered by endothelium[7,8]. When hemolymphangioma of the intestine exists, the submucosal vascular and lymphatic network is affected, with many dilated, thin-walled and irregular blood and lymph fluid filled spaces, mainly located within the mucosa and submucosa[1]. This tumor could also invade the adjacent structures[8].
Hemolymphangioma of intestine is manifested clinically as recurrent, acute or chronic painless alimentary tract hemorrhage[1]. Differential diagnoses include adenomatous polyps, tumors and hemorrhoids. Clinical examination might show mild tenderness, and nodular mucosa, however, no obvious mass could be detected. Complications like massive rectal bleeding, severe anemia, vessel compression or even pelvic organ infiltration could sometimes occur.
Colonoscopy should be performed to rule out a malignancy or other problems. Elevated blue nodular lesions or dilated vessels are characteristic findings in the colon wall. Biopsy should not be performed because of the high risk of massive bleeding. The endoscopic ultrasonography is recommended because of its characteristic findings and anechoic mass with clear edge. CT and MRI are useful in defining the extent and the invasion of the mass, and planning the surgical strategy[9]. It is very important and crucial for radiologists to recognize these lesions and establish an accurate diagnosis so as to avoid a biopsy which could cause severe hemorrhage. However, accurate diagnosis could not usually be established preoperatively.
Elective treatment should be performed and complete surgical resection of the hemolymphangioma is considered the most effective treatment. A thorough exploration of the abdominal cavity should be performed because of the potential invasion to the surrounding organs. Other options of treatment include sclerotherapy, electrocautery, radium implantation, cryosurgery and laser therapy, but these are non-surgical techniques and may only result in temporary clinical outcomes[10,11]. Angiography and embolization can be applied in cases of acute bleeding, but rebleeding may occur. For the low malignant potential tumors, a sphincter-saving surgery is recommended after a full evaluation of the tumor, followed by sufficient follow-up[12].
In summary, hemolymphangioma of the rectum is an uncommon vascular and lymphatic lesion, presenting with recurrent and painless rectal bleeding. Preoperative imaging examinations such as endoscopic ultrasonography, CT and MRI are helpful in confirming the diagnosis, and in planning the surgical strategy, and a sphincter-saving surgery is recommended after a full evaluation of the tumor.
P- Reviewer Blank G S- Editor Song XX L- Editor A E- Editor Li JY
| 1. | Fang YF, Qiu LF, Du Y, Jiang ZN, Gao M. Small intestinal hemolymphangioma with bleeding: a case report. World J Gastroenterol. 2012;18:2145-2146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Bethouart M, Houcke M, Proye C, Linquette M. Hepatosplenic hemolymphangioma. Lille Med. 1980;25:288-290. [PubMed] |
| 3. | Canavese F, Cortese MG, Proietti L, Costantino S, Rosina M, Nangeroni M, Defilippi C, Di Rosa GP. Bulky-pedunculated hemolymphangioma of the esophagus: rare case in a two-years old girl. Eur J Pediatr Surg. 1996;6:170-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Zhang X, Sheng X, Liu F, Jian R, Li L, Luo R. Hemolymphangioma of the chest wall: A rare case report. Oncol Lett. 2012;3:816-818. [PubMed] |
| 5. | Nataf P, Mestiri T, Martin de Lasalle E, Benomar M, Gandjbakhch I, Cabrol C. Pericardial hemolymphangioma. Apropos of a case. Arch Mal Coeur Vaiss. 1988;81:1137-1140. [PubMed] |
| 6. | Gossot D, Decazes JM, Sarfati E, Dubost C. Cystic hemolymphangioma of the adrenal gland. J Chir (Paris). 1987;124:404-405. [PubMed] |
| 7. | Sun LF, Ye HL, Zhou QY, Ding KF, Qiu PL, Deng YC, Zhang SZ, Zheng S. A giant hemolymphangioma of the pancreas in a 20-year-old girl: a report of one case and review of the literature. World J Surg Oncol. 2009;7:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 8. | Toyoki Y, Hakamada K, Narumi S, Nara M, Kudoh D, Ishido K, Sasaki M. A case of invasive hemolymphangioma of the pancreas. World J Gastroenterol. 2008;14:2932-2934. [PubMed] |
| 9. | Kosmidis I, Vlachou M, Koutroufinis A, Filiopoulos K. Hemolymphangioma of the lower extremities in children: two case reports. J Orthop Surg Res. 2010;5:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Vilallonga R, Espin Basany E, Armengol M. Cavernous hemangioma: unusual benign tumor of the transverse colon. Turk J Gastroenterol. 2009;20:146-149. [PubMed] |
| 11. | Wang LC, Krunic AL, Medenica MM, Soltani K, Busbey S. Treatment of hemorrhagic lymphatic malformation of the tongue with a pulsed-dye laser. J Am Acad Dermatol. 2005;52:1088-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Ugolini G, Rosati G, Montroni I, Manaresi A, Blume JF, Taffurelli M. Diffuse cavernous haemangioma of the rectum and anus: an unusual case of rectal bleeding with challenging management. BMJ Case Rep. 2009;2009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |