Published online Nov 21, 2013. doi: 10.3748/wjg.v19.i43.7696
Revised: September 19, 2013
Accepted: September 29, 2013
Published online: November 21, 2013
Processing time: 124 Days and 17 Hours
AIM: To analyzed whether laparoscopy-assisted percutaneous endoscopic gastrostomy (PEG) could be a valuable option for patients with complicated anatomy.
METHODS: A retrospective analysis of twelve patients (seven females, five males; six children, six young adults; mean age 19.2 years) with cerebral palsy, spastic quadriparesis, severe kyphoscoliosis and interposed organs and who required enteral nutrition (EN) due to starvation was performed. For all patients, standard PEG placement was impossible due to distorted anatomy. All the patients qualified for the laparoscopy-assisted PEG procedure.
RESULTS: In all twelve patients, the laparoscopy-assisted PEG was successful, and EN was introduced four to six hours after the PEG placement. There were no complications in the perioperative period, either technical or metabolic. All the patients were discharged from the hospital and were then effectively fed using bolus methods.
CONCLUSION: Laparoscopy-assisted PEG should become the method of choice for gastrostomy tube placement and subsequent EN if PEG placement cannot be performed safely.
Core tip: Enteral nutrition (EN) is a life-saving procedure, preventing complications associated with malnutrition. The best solution for EN is percutaneous endoscopic gastrostomy (PEG). In some cases, however, creating such access is impossible. In those cases, laparoscopy-assisted PEG should become the method of choice for gastrostomy tube placement and subsequent EN if PEG placement cannot be performed safely.
- Citation: Hermanowicz A, Matuszczak E, Komarowska M, Jarocka-Cyrta E, Wojnar J, Debek W, Matysiak K, Klek S. Laparoscopy-assisted percutaneous endoscopic gastrostomy enables enteral nutrition even in patients with distorted anatomy. World J Gastroenterol 2013; 19(43): 7696-7700
- URL: https://www.wjgnet.com/1007-9327/full/v19/i43/7696.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i43.7696
Tube enteral feeding is the method of choice when an oral diet is insufficient or impossible for more than seven days, even in patients without apparent malnutrition[1]. Tube enteral feeding is also strongly recommended if the latter is present or imminent[1]. All these patients should be administered enteral nutrition (EN), and when the oral diet cannot be continued, tube feeding is the best option. Since its introduction by Gauderer in 1980, percutaneous endoscopic gastrostomy (PEG) has become the method of choice for EN in all age groups[2]. The primary goal of EN is to improve the patient’s well-being by preventing or reversing malnutrition and avoiding its consequences. EN is particularly important in pediatric patients because they need to not only survive but also grow. Neurological disorders place children at a very high risk of malnutrition; hence, this group of patients benefits very quickly from EN. Unfortunately, neurological disorders are very often accompanied by serious distortions in body anatomy.
Problems, such as severe kyphoscoliosis, interposed organs or other forms of distorted anatomy, may prevent effective and safe PEG placement due to an inability to guarantee the three principles of safe PEG placement: endoscopic gastric distension, endoscopically visible focal finger invagination and transillumination[3,4]. In such cases, surgical gastrostomy, which is an invasive procedure, is often the only option for EN. However, less invasive measures would be preferable over surgical gastronomy. Our study aimed to determine whether laparoscopy-assisted PEG placement is a useful option for EN in patients with distorted anatomy and who are unable to undergo PEG placement.
This study was a retrospective analysis of twelve patients (seven females, five males; mean age 19.2 years), who were treated at the pediatric surgery center in Bialystok, Poznan and Skawina, Poland. Six patients were children, and the remaining six were adults. In all patients, malnutrition requiring nutritional support was diagnosed (body mass index < 14 m2/kg), and tube feeding was recognized as the method of choice for EN. In all four patients, PEG placement was impossible due to spastic quadriparesis, severe kyphoscoliosis and interposed organs. Informed consent was collected from all patients. The patients and procedure characteristics are presented in Table 1.
| No. | Gender | Age (yr) | Reason of LAPEG | BMI before the procedure/albumin concentration (g/dL) | BMI after 12 mo follow up | Time from insertion of the gastroscope to the peg placement (total operation length)/min | Time form insertion laparoscope to removal of the laparoscope/min |
| 1 | F | 7 | Tay-Sachs disease | 11.9/2.9 | 14.5 | 22 | 16 |
| 2 | M | 5 | drug-resistant epilepsy | 13.9/3.9 | 15.2 | 17 | 13 |
| 3 | M | 15 | cerebral palsy | 13.2/4.5 | 15.2 | 15 | 9 |
| 4 | F | 3 | Patau syndrome | 13.8/5.1 | 16.0 | 21 | 12 |
| 5 | M | 17 | cerebral palsy | 12.6/3.3 | 18.4 | 24 | 14 |
| 6 | M | 11 | cerebral palsy | 13.2/3.7 | 17.1 | 22 | 9 |
| 7 | F | 22 | Wilson’s disease | 12.0/28 | 13.5 | 21 | 17 |
| 8 | F | 31.5 | Gaucher’s disease | 14.5/29.5 | 14.5 | 18 | 12 |
| 9 | M | 26.2 | cerebral palsy | 15.5/27.0 | 15.2 | 16 | 8 |
| 10 | F | 33.2 | SLA | 14.0/25.0 | 17.0 | 12 | 11 |
| 11 | F | 34 | SLA | 11.0/2.3 | 14.5 | 14 | 11 |
| 12 | F | 24.7 | cerebral palsy | 11.5/2.9 | 15.0 | 13 | 7 |
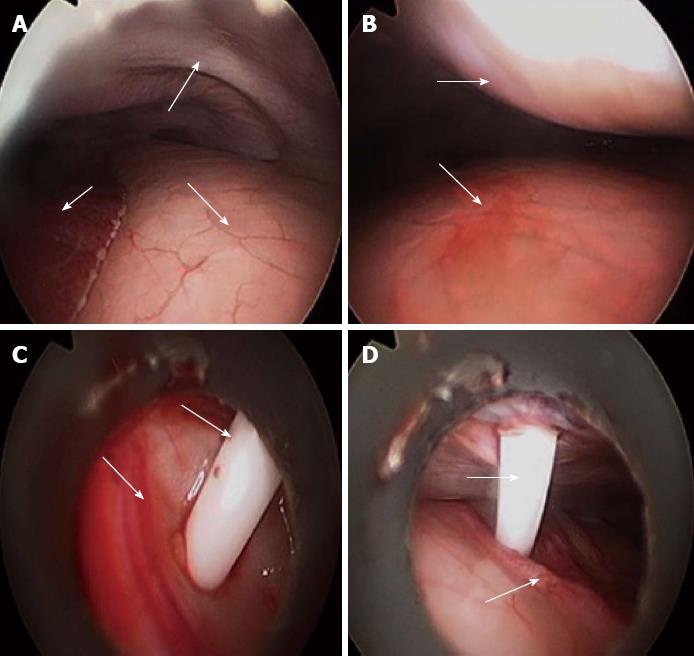
PEG tube insertion was performed under general anesthesia. A single dose of intravenous antibiotics was given. The patient was positioned in the supine position. After sterilizing the skin on the anterior abdominal wall, a 5-mm port was inserted under the umbilicus using Hasson’s open technique[5]. Pneumoperitoneum was established via a trocar, using carbon dioxide. The intra-abdominal pressure in our patients was 10 mmHg. The peritoneal cavity and the abdominal and gastric walls were inspected for suitable sites for the gastrostomy. After insertion of the gastroscope into the stomach and air insufflation, the gastrostomy site was selected under laparoscopic and endoscopic guidance. The skin was incised above the gastrostomy site with a length of 0.5 cm. A trocar with a needle was pushed through this point into the stomach under complete laparoscopic and endoscopic visualization. The PEG was made using the ‘pull’ technique: a thread was inserted through the trocar after removing the needle and was then snared. The endoscope was withdrawn by the snare holding the thread. A suitably sized PEG tube was then connected to the thread, and the thread was pulled from the skin incision, pulling the tube into patient’s mouth through the esophagus. The PEG tube was retained in the stomach with an internal bolster. An external bolster was placed loosely on the skin[2,3]. All the procedures were uneventful and without any intraoperative complications.
The laparoscopy-assisted PEG insertion was successful in all twelve patients. The mean length of the procedure was 16.5 min. A Flocare PEG tube (Nutricia Ltd., Poland) with a diameter of 14 Cherrier was used as the gastric catheter.
No postoperative complications were observed, and EN was commenced four to six hours after the PEG placement using the bolus method (5 mL × 100 mL). The mean length of the hospital stay was 1.5 d. All the patients were discharged from the hospital and then effectively fed using bolus methods at long-term facilities. The follow-up at twelve months did not reveal any complications. The nutritional status of the patients improved significantly, with the mean BMI reaching 17.5 m2/kg (Table 1).
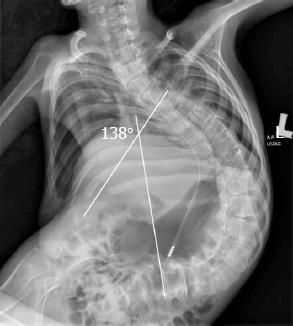
Tube feeding is the method of choice when EN is recommended[1]. In most cases, PEG tube insertion is a safe procedure and does not lead to complications[3,6]. Fatal outcomes have been reported due to comorbidities when the PEG was inserted in the setting of severe disease[3,7]. However, the safe placement of a PEG tube requires a permeable esophagus and transillumination of the stomach through the abdominal wall. Impaired coagulation, severe ascites, peritonitis and local esophageal and general gastrointestinal obstructions are considered to be absolute contraindications[3,4,8]. Severe kyphoscoliosis with interposed organs and distorted anatomy are considered to be relative contraindications[8-10] (Figure 1). In patients with severe kyphoscoliosis, the PEG tube cannot be placed in the usual locations due to organ displacement. In our patients, the contraindications for PEG included the translocation of the stomach into the left lower quadrant of the abdomen (3 patients) or into the middle part of the abdomen (1 patient) (Figure 2). Therefore, in patients with severe kyphoscoliosis, patients suffering from hepatomegaly, splenomegaly, obesity or an intra-abdominal or peritoneal tumor, patients with previous abdominal surgery, especially involving the stomach, and patients with advanced esophageal cancer, when transillumination of the stomach is not achieved, there is an indication for laparoscopic, fluoroscopic or sonographic guidance during the PEG tube placement.
The technique for the laparoscopic-assisted PEG procedure was described for the first time by Raaf et al[11] in 1993. In 1995, Stringel et al[12] reported a laparoscopic-assisted PEG procedure in 2 children in whom attempts at a simple PEG had failed. There are also other alternative methods for PEG placement when transillumination is not possible. Radiologic techniques have been used successfully in these patients since 1981[13,14]. The gastric tubes can be placed under ultrasound or fluoroscopic guidance[15-17]. Recently, the placement of the gastric tubes has used Computed tomography (CT) fluoroscopy guidance, even in combination with simultaneous gastroscopy[18].
Historically, gastroesophageal reflux was also considered to be a contraindication, as concluded by Yaseen et al[19]. Recent trials have shown that gastroesophageal reflux might actually improve after PEG placement because the PEG creates a type of anterior pseudo-gastropexy[20,21].
Major complications related to PEG include the following: colonic perforation, esophageal tear, small bowel injury, hepatic or splenic injury, tube migration with or without intestinal obstruction, gastrointestinal bleeding and site or generalized infection. These complications have been reported with variable incidences (5%-17%) in published series[3,4,7,22]. The most severe complication, with an incidence of 0.0008%-0.04%, is esophageal perforation[4,23]. Predisposing factors include anatomic anomalies in up to 50% of cases[3]. Patients with displacement of the transverse colon over the anterior gastric wall are predisposed to colonic injury during the PEG procedure[3,23,24]. Colonic injury usually presents with peritonitis, and surgery is then required. Additionally, interposition of the splenic flexure between the anterior abdominal and gastric walls may result in gastro-colo-cutaneous fistulae after PEG placement without direct visual monitoring. The PEG tube is placed through the large bowel into the stomach. Such patients may be almost completely asymptomatic except for transient fever and ileus. The management involves PEG tube removal and spontaneous closure of the fistula[4,25]. Small bowel injuries are rather rare because the greater omentum separates the small bowel from the upper abdomen. Small bowel volvulus around the PEG usually presents with a small bowel obstruction caused by a gap between the gastric and abdominal walls[4]. Hepatic and splenic PEG-related injuries are also rare. In hemodynamically stable patients, a CT scan can confirm the diagnosis. Hemodynamically unstable patients require emergent surgical exploration, placement of hemostatic sutures in the liver or a splenectomy. Severe hemorrhage is a rare complication of PEG (0.02%-0.06%) and is usually due to anticoagulation, antiplatelet therapy or an anatomic anomaly, as observed in our patients[3,23]. We did not notice any major complications from the PEG tube insertion in our patients. In our opinion, only continuous laparoscopic monitoring can ensure that the omentum, colon and small bowel will not be interposed between the stomach and the anterior abdominal wall during gastrostomy fixation in extremely malnourished children with severe kyphoscoliosis.
Minor complications, such as superficial skin infections, superficial granulation tissue formation and tube leak, are common and may occur in up to 50% of patients[3,4,9,26]. Minor skin infections usually respond to enteral antibiotics, and granulation tissue usually responds to local cautery with silver nitrate swabs. We did not notice any skin infections, tube leaks or granulation tissue formation in our patients. The patients’ families and caregivers were taught how to flush the tube after feeding to avoid tube obstruction.
With respect to the laparoscopy, we use Hasson’s open method and an optical access trocar to achieve pneumoperitoneum[5]. In our opinion, this method decreases the risk of injuries compared with the blind insertion of the Veress needle; however, Hasson’s method may cause air leaks and prolong the operative time. In our cases, the mean duration of the operation time from the insertion of the laparoscope to the removal of the laparoscope did not differ significantly from that of the classic PEG procedure. We did not have continuous air leaks, and the operating time was not prolonged much because of the laparoscopy. Therefore, we have continued to use this technique as the preferred method for inducing pneumoperitoneum in children. Under laparoscopic observation, the stomach can be punctured in the correct location, avoiding the colon or the liver on its way into the gastric lumen. In our study, the laparoscopic-assisted PEG procedures were performed without difficulty. There was no need to maneuver or relocate the interposed organs during the laparoscopy. This procedure, for which the technical aspects are presented in Figure 2, allowed for successful EN. The subsequent EN helped our patients recover from starvation and decreased their malnutrition-related complication ratio.
In conclusion, the laparoscopy-assisted PEG procedure is a valuable method for gastrostomy tube placement in patients in whom an upper endoscopy is possible but PEG cannot be performed safely. In our opinion, laparoscopy-assisted PEG should become the method of choice for children and adults with distorted anatomy.
Enteral nutrition (EN) is a life-saving procedure that prevents the complications associated with malnutrition. Percutaneous endoscopic gastrostomy (PEG) is the method of choice for this type of intervention because the procedure enables tube feeding.
PEG placement is not always possible due to technical difficulties, such as interposed organs or kyphosis. This study aimed to analyze whether laparoscopy-assisted PEG could be a valuable option in those patients in whom the standard procedure is impossible due to distorted anatomy.
For all the patients, the laparoscopy-assisted PEG tube placement was successful, and the EN was started four to six hours after its placement, proving that this technique is safe and effective.
Laparoscopy-assisted PEG should become the method of choice for gastrostomy tube placement and subsequent EN if PEG placement cannot be performed safely.
This is an interesting article of case series of laparoscopy-assisted PEG.
P- Reviewers: Li XL, Nishiwaki S, Radaelli F S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
| 1. | Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, Jauch KW, Kemen M, Hiesmayr JM, Horbach T. ESPEN Guidelines on Enteral Nutrition: Surgery including organ transplantation. Clin Nutr. 2006;25:224-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 736] [Cited by in RCA: 659] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 2. | Gauderer MW. Percutaneous endoscopic gastrostomy and the evolution of contemporary long-term enteral access. Clin Nutr. 2002;21:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | El-Matary W. Percutaneous endoscopic gastrostomy in children. Can J Gastroenterol. 2008;22:993-998. [PubMed] |
| 4. | Strassler HE. A combination of dental procedures gives patients the desired smile. Dent Off. 1991;11:4, 7. [PubMed] |
| 5. | Humphrey GM, Najmaldin A. Modification of the Hasson technique in paediatric laparoscopy. Br J Surg. 1994;81:1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Catto-Smith AG, Jimenez S. Morbidity and mortality after percutaneous endoscopic gastrostomy in children with neurological disability. J Gastroenterol Hepatol. 2006;21:734-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Gauderer MW. Percutaneous endoscopic gastrostomy: a 10-year experience with 220 children. J Pediatr Surg. 1991;26:288-292; discussion 292-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 130] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Löser C, Aschl G, Hébuterne X, Mathus-Vliegen EM, Muscaritoli M, Niv Y, Rollins H, Singer P, Skelly RH. ESPEN guidelines on artificial enteral nutrition--percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005;24:848-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 362] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 9. | DeLegge RL, DeLegge MH. Percutaneous endoscopic gastrostomy evaluation of device materials: are we “failsafe”? Nutr Clin Pract. 2005;20:613-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Broscious SK. Preventing complications of PEG tubes. Dimens Crit Care Nurs. 1995;14:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Raaf JH, Manney M, Okafor E, Gray L, Chari V. Laparoscopic placement of a percutaneous endoscopic gastrostomy (PEG) feeding tube. J Laparoendosc Surg. 1993;3:411-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Stringel G, Geller ER, Lowenheim MS. Laparoscopic-assisted percutaneous endoscopic gastrostomy. J Pediatr Surg. 1995;30:1209-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Preshaw RM. A percutaneous method for inserting a feeding gastrostomy tube. Surg Gynecol Obstet. 1981;152:658-660. [PubMed] |
| 14. | Lim A Po IF, van Overhagen H, Nicolai JJ. [Gastrostomy tubes inserted with radiologic techniques]. Ned Tijdschr Geneeskd. 2003;147:373-377. [PubMed] |
| 15. | Hoffer EK. US-guided percutaneous gastrostomy: a portable technique. J Vasc Interv Radiol. 1996;7:431-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Ahlers CM, Schneider J, Lachmann R, Herber S, Düber C, Pitton MB. Fluoroscopy-guided removal of pull-type gastrostomy tubes. Cardiovasc Intervent Radiol. 2008;31:1252-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Chaves DM, Kumar A, Lera ME, Maluf F, Artifon EL, Moura EG, Halwan B, Ishioka S, Sakai P. EUS-guided percutaneous endoscopic gastrostomy for enteral feeding tube placement. Gastrointest Endosc. 2008;68:1168-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Spelsberg FW, Hoffmann RT, Lang RA, Winter H, Weidenhagen R, Reiser M, Jauch KW, Trumm C. CT fluoroscopy guided percutaneous gastrostomy or jejunostomy without (CT-PG/PJ) or with simultaneous endoscopy (CT-PEG/PEJ) in otherwise untreatable patients. Surg Endosc. 2013;27:1186-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Yaseen M, Steele MI, Grunow JE. Nonendoscopic removal of percutaneous endoscopic gastrostomy tubes: morbidity and mortality in children. Gastrointest Endosc. 1996;44:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Wilson GJ, van der Zee DC, Bax NM. Endoscopic gastrostomy placement in the child with gastroesophageal reflux: is concomitant antireflux surgery indicated? J Pediatr Surg. 2006;41:1441-1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Samuel M, Holmes K. Quantitative and qualitative analysis of gastroesophageal reflux after percutaneous endoscopic gastrostomy. J Pediatr Surg. 2002;37:256-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Khattak IU, Kimber C, Kiely EM, Spitz L. Percutaneous endoscopic gastrostomy in paediatric practice: complications and outcome. J Pediatr Surg. 1998;33:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 137] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Gonvers JJ, Burnand B, Froehlich F, Pache I, Thorens J, Fried M, Kosecoff J, Vader JP, Brook RH. Appropriateness and diagnostic yield of upper gastrointestinal endoscopy in an open-access endoscopy unit. Endoscopy. 1996;28:661-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Guloglu R, Taviloglu K, Alimoglu O. Colon injury following percutaneous endoscopic gastrostomy tube insertion. J Laparoendosc Adv Surg Tech A. 2003;13:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 25. | Berger SA, Zarling EJ. Colocutaneous fistula following migration of PEG tube. Gastrointest Endosc. 1991;37:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Ségal D, Michaud L, Guimber D, Ganga-Zandzou PS, Turck D, Gottrand F. Late-onset complications of percutaneous endoscopic gastrostomy in children. J Pediatr Gastroenterol Nutr. 2001;33:495-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 2.5] [Reference Citation Analysis (0)] |