Published online Nov 7, 2013. doi: 10.3748/wjg.v19.i41.7197
Revised: August 30, 2013
Accepted: September 3, 2013
Published online: November 7, 2013
Processing time: 180 Days and 3.1 Hours
AIM: To assess the theoretical advantages of magnetic endoscope imaging (MEI) over standard colonoscopies (SCs) and to compare their efficacies.
METHODS: Electronic databases, including PubMed, EMBASE, the Cochrane library and the Science Citation Index, were searched to retrieve relevant trials. In addition, abstracts from papers presented at professional meetings and the reference lists of retrieved articles were reviewed to identify additional studies. The meta-analyses were performed using RevMan 5.1. A random effect model with the Mantel-Haenszel method was used for pooling dichotomous and continuous data. A sensitivity analysis was performed by excluding the trials with a small number of patients and by excluding the trials performed by inexperienced providers.
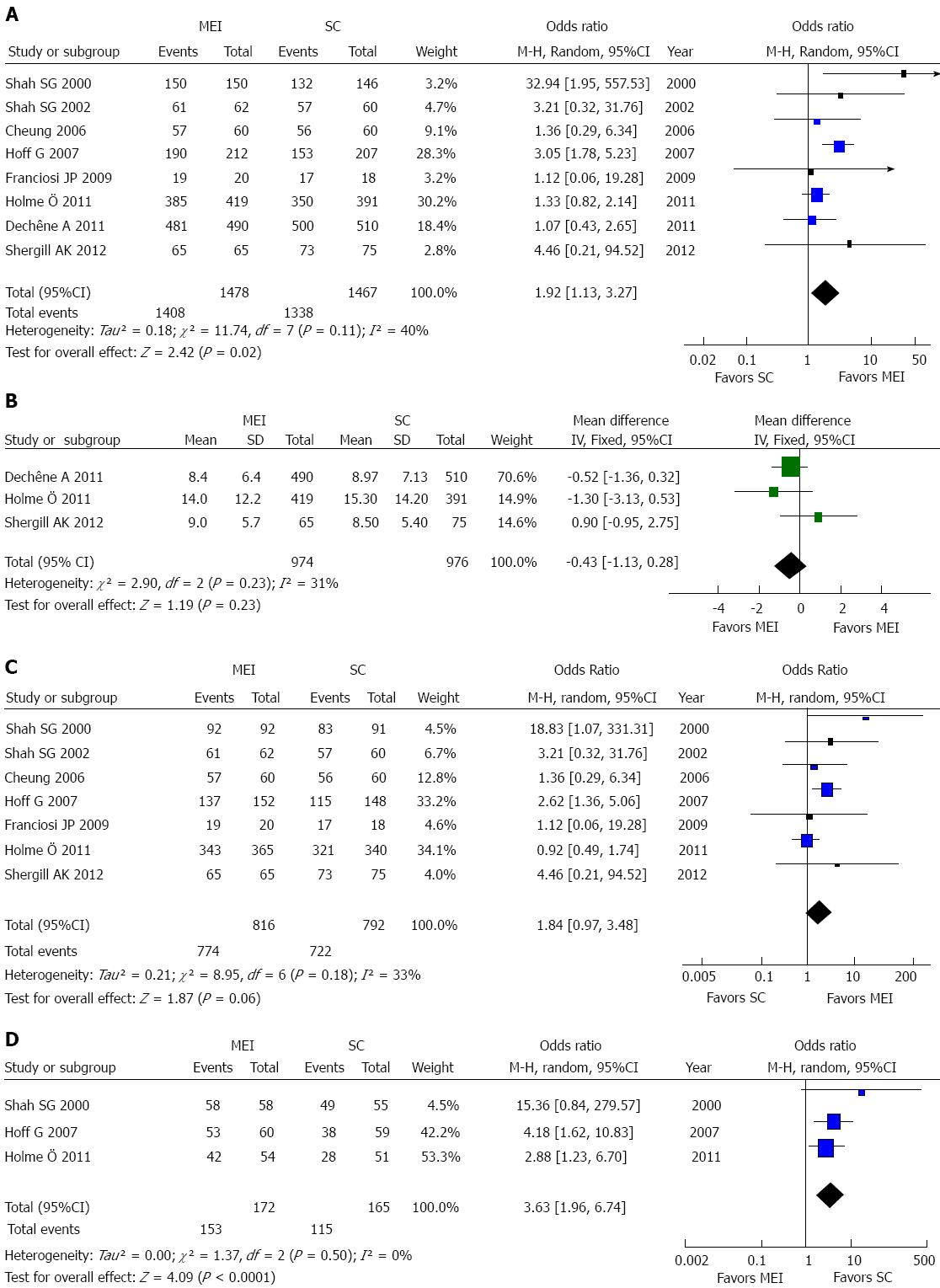
RESULTS: Eight randomized controlled trials (RCTs), including 2967 patients, were included in the meta-analysis to compare cecal intubation rates and times, sedation dose, abdominal pain scores and the use of ancillary maneuvers between MEI and SC. The overall OR was 1.92 (95%CI: 1.13-3.27, eight RCTs), as indicated by the cecal intubation rate of MEI compared with SC, but MEI did not have any distinct advantage over SC for cecal intubation time (MD = -0.07, 95%CI: -0.16-0.02; three RCTs). MEI did not generally result in lower pain scores. Outcomes were also analyzed for the two subgroups based on the endoscopists’ experience level to evaluate cecal intubation rates. MEI presented better outcomes for non-experienced colonoscopists than experienced colonoscopists.
CONCLUSION: The real-time magnetic imaging system is of benefit in training and educating inexperienced endoscopists and improves the cecal intubation rate for experienced and inexperienced endoscopists.
Core tip: This study aimed to assess the theoretical advantages of magnetic endoscopic imaging (MEI) over standard colonoscopy (SC) and to compare the efficacies of MEI and SC. The meta-analyses compared the cecal intubation rate and time, sedation dose used, abdominal pain scores and the use of ancillary maneuvers between MEI and SC. The real-time magnetic imaging system is of benefit in training and educating inexperienced endoscopists, and it improved the cecal intubation rate for both experienced and inexperienced endoscopists.
-
Citation: Chen Y, Duan YT, Xie Q, Qin XP, Chen B, Xia L, Zhou Y, Li NN, Wu XT. Magnetic endoscopic imaging
vs standard colonoscopy: Meta-analysis of randomized controlled trials. World J Gastroenterol 2013; 19(41): 7197-7204 - URL: https://www.wjgnet.com/1007-9327/full/v19/i41/7197.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i41.7197
Colonoscopy is the gold standard and the most common and accurate tool for detecting important structural lesions of the lower gastrointestinal tract and for diagnosing colonic diseases, such as polyps, colorectal cancer and inflammatory bowel disease[1-3]. However, the existence of sharp angulation or looping of the colon increases the difficulty of the procedure and causes distinct discomfort for patients. The failure rate of initially reaching the cecum remains significant at 2%-10%[4-6]. In addition, there is still a small but definite risk of procedure-related complications, notably bleeding and perforation[7,8]. Thus, technological advances in colonoscopy have continued over the last decade[9,10].
Magnetic endoscopic imaging (MEI) is a non-radiographic imaging technique that has been developed in recent years that is capable of displaying real-time three-dimensional images of the colonoscope shaft within the abdominal cavity[11-12]. The MEI system has previously been described in detail[13]. A pulsed low-magnetic field is sequentially produced by a series of electromagnetic generator coils spaced 10 cm apart along a catheter inserted through the accessory channel of the endoscope. The imager view is updated every 0.2 s to make the system essentially real time, and the images are subsequently recorded on a computer disk for subsequent replay or analysis[14]. The MEI system has been shown to be beneficial in increasing the cecal intubation rate[15,16], reducing the number of attempts to straighten loops[16,17], and in reducing the duration of looping, especially with trainees, when compared with no visualization. To date, a few studies have compared MEI with standard colonoscopy (SC); however, the results have not been uniform.
The aim of the present meta-analysis was to evaluate the effect of the two different methods.
First, electronic databases, including PubMed (1966 to June 2012), EMBASE (1980 to June 2012), the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 6 of 12, June 2012), and the Science Citation Index, were searched. The search was performed with the following search terms as free-text terms as well as MeSH terms: colonoscope, colonoscopy, magnetic and magnetic endoscopic imaging. Second, meeting abstracts and the reference lists of the retrieved articles were reviewed for additional relevant studies. No language restrictions were imposed.
The instruments used in the trials included the Olympus CF-1T200L scope (160 cm)[16,17], the ScopeGuide endoscope insertion tube system[18-20], the Olympus CF-Q160DI with the Olympus ScopeGuide system[15,21], the Olympus CF-Q180AL, the Olympus CF-Q160AL and the CF-Q140DL/I with the Olympus ScopeGuide system.
Randomized controlled trials (RCTs) comparing MEI with SC were included in this analysis. Only the most recent study was included if more than one study was published using the same study population. Thirty-five papers were uncontrolled, observational studies and case reports and were thus excluded from the meta-analysis.
All the data were tabulated with standard data abstractions sheets. For each study and each type of intervention, the following characteristics were exacted: study design and conduct, numbers of patients, endoscopist characteristics, instrument features and study outcomes. The study outcomes included the cecal intubation rate, cecal intubation time, sedation dose used, abdominal pain score, and ancillary maneuvers during the procedure (manual pressure used and position changes made).
Two investigators (Chen Y and Xie Q) independently extracted details of the study population, interventions and outcomes. A paper was reviewed if either of the two investigators thought its abstract was relevant. If there were any discrepancies in the information provided in a title and the corresponding abstract, the full article was reviewed for clarification. Differences in opinion were resolved by discussion with the third author of this paper (Chen B).
To avoid the risk of bias in the assessment, two investigators independently used an assessment form recommended by the Cochrane Handbook. Any disagreements were resolved by discussion with a third author until consensus was obtained. We considered the following criteria: (1) Sequence generation: was the allocation sequence adequately generated? (2) Allocation concealment: was the allocation adequately concealed? (3) Blinding: was knowledge of the allocated intervention adequately prevented during the study? (4) Incomplete outcome data: were incomplete outcome data adequately addressed? (5) Selective outcome reporting: were reports of the study free of the suggestion of selective outcome reporting? and (6) Other sources of bias: was the study apparently free of other problems that could place it at a high risk of bias?
Each domain was graded as yes (low risk of bias), no (high risk of bias), or unclear (uncertain risk of bias) according to the criteria.
For rating the strength and quality of the evidence for a given comparison, the Working Group grades of evidence and Summary of Findings tables recommended by the Cochrane Collaboration were used.
For the assessment of publication bias, a funnel plot was constructed if sufficient data were available.
Meta-analyses were conducted for trials comparing MEI with SC using the statistical tool Revman 5.1. Dichotomous data were expressed as an OR, and continuous outcomes were expressed as the mean difference (MD) with a 95%CI. A random effects model was used for the pooling of data.
We used a random effect model with the Mantel-Haenszel method for pooling dichotomous and continuous data. We assessed the heterogeneity of the trial results by calculating the I2 measure of inconsistency with a cutoff point of I2 = 50%.
A sensitivity analysis was performed by excluding the trials with small numbers of patients and by excluding the trials performed by inexperienced providers.
Overall, our searches identified 43 articles that compared MEI with SC. After reading the abstracts and full-texts, we excluded 35 of these articles because they were reviews or were not RCTs or case reports. Finally, eight studies met the criteria for inclusion in the review[9-15,22].
The characteristics of these studies are summarized in Table 1. All of these studies were RCTs, containing a total of 2967 participants (1566 male, 1401 female) of 7 to 90 years of age.
| Study | Number ofpatients (n) | Endoscopists' experience level | Colonos-cope type | Cecal intubation rate | Cecal intubation time | Sedation dose | Pain score | Ancillary maneuvers |
| Shah et al[16] | 296 (male 138, female 158) | Trainees, skilled endoscopists | MEI, SC | Total MEI: 100% (150/150) SC: 90.4% (132/146) Trainees: MEI: 100% (58/58) SC: 89% (49/55) P = 0.0115 Skilled endoscopists: MEI: 100% (92/92) SC: 91% (83/91) P = 0.0032 | Trainees: Median, min MEI: 11.8 (4.3-31.5) SC: 15.3 (4-67) P = 0.0092 Skilled endoscopists: MEI: 8.0 (2.6-40.8) SC: 9.3 (2.5-52.6) P = 0.0484 | Trainees: Mean (SD) Midazolam, mg MEI: 1.2 (0.4) SC: 1.2 (0.4) P = 0.4013 Pethidine, mg MEI: 26 (14.5) SC: 30 (15.5) P = 0.1674 Skilled endoscopists Mean (SD) Midazolam, mg MEI: 1.3 (1.1) SC: 1.6 (1.0) P = 0.0724 pethidine, mg MEI: 30 (23.9) SC: 34 (25.6) P = 0.2036 | Trainees: Mean (SD) 0-100 VAS MEI: 28.5 (20.2) SC: 30.1 (24.4) P = 0.553 Skilled endoscopists: MEI: 28.6 (23.1) SC: 24.8 (24.2) P = 0.30 | Abdominal hand pressure used: Trainees: MEI: 78 SC: 61 Skilled endoscopists: MEI: 93 SC: 147 |
| Shah et al[17] | 122 (male 62, female 60) | Experienced | MEI, SC | MEI: 97% (61/62) SC: 95% (57/60) P = 0.3606 | Median, min MEI: 10.6 (7.6-17.03) SC: 13.1 (9.01-26.47) P = 0.0664 | Midazolam (mg), median MEI: 0.44 (0-1.48) SC: 0.88 (0-1.47) P = 0.2875 Meperidine (mg), median MEI: 16.75 (0-59) SC: 32.5 (0-59) P = 0.2643 | Patient pain score (100 mm VAS) MEI: 19 (9-29) SC: 29 (10-50) P = 0.0662 | Not stated |
| Cheung et al[18] | 120 (male, 64 female 56) | Experienced | MEI, SC | MEI: 95% (57/60) SC: 93% (56/60) P = 1.0 | Median, min MEI: 5 (2-46) SC: 5 (3-15) P = 0.32 | Not stated | Median (range), pain score from patients MEI: 5 (0-10) SC: 4 (0-10) P = 0.13 | Abdominal hand pressure MEI: 0 SC: 0 Position change made MEI: 6.7% SC: 0% P = 0.12 |
| Hoff et al[15] | 419 (male 202, female 217) | Experienced, inexperienced | MEI, SC | MEI: 90% (190/212) SC: 74% (153/207) P < 0.001 experienced: MEI: 90% (137/152) SC: 78% (115/148) P =0.003 Inexperienced: MEI: 88%(53/60) SC: 64%(38/59) P = 0.002 | Mean (95%CI), min MEI: 19.1 (17.2-21.0) SC: 17.6 (15.8-19.5) P = 0.28 | Not stated | Severe pain during Examination: experienced MEI: 7.3% (10/137) SC: 16% (21/132) P = 0.03 Inexperienced MEI: 14% (8/56) SC: 15% (7/47) P = 0.93 | Not stated |
| Franciosi et al[19] | 40 (male 16, female 24) | Experienced | MEI, SC | MEI: 95% (19/20) SC: 94.4% (17/18) P = ns | Mean (range), min MEI: 16.5 (6-52) SC: 12 (6-33) P = ns | Not stated | Median, 0-10 pointscale MEI: 7 (2-10) SC: 19 (3-10) P = ns | Not stated |
| Dechêne et al[20] | 1000 (male 550, female 450) | Experienced, inexperienced | MEI, SC | MEI: 98.2% (481/490) SC: 98.0% (500/510) P = ns | Mean time, (s) MEI: 507 ± 384 (8.45 ± 6.4) SC: 538 ± 428 (8.97 ± 7.13) P = ns Inexperienced: MEI: 613 ± 435 (225) SC: 660 ± 458 (245) P = ns Experienced: MEI: 415 ± 304 (256) SC: 421 ± 361 (255) P = ns | Not stated | Not stated | Position change made MEI: 1.5% (7/481) SC: 3.0% (15/500) P = ns Manual pressure used MEI: 4.2% (20/481) SC: 6.4% (32/500) P = ns |
| Holme et al[21] | 810 (male 378, female 432) | Experienced, inexperienced | MEI, SC | MEI: 91.9% (385/419) SC: 89.5% (350/391) P = 0.28 Inexperienced: MEI: 77.8% (42/54) SC: 56.0% (28/51) P = 0.022 Experienced: MEI: 94.0% (343/365) SC: 96.0% (321/340) P = 0.87 | Mean ± SD MEI: 14.0 ± 12.2 SC: 15.3 ± 14.2 P = 0.67 Experienced: MEI: 11.4 ± 7.2 SC: 12.3 ± 9.4 P = 0.78 Inexperienced: MEI: 31.7 ± 21.3 SC: 35.7 ± 22.1 P = 0.42 | Not stated | No pain during examination: MEI: 24% (82/341) SC: 20.8% (66/318) Severe pain during examination: MEI: 0 SC: 0 | Need for assistance experienced: MEI: 1.1% (4/365) SC: 1.5% (5/340) P = 0.75 Inexperienced: MEI: 18.5% (10/54) SC: 40% (20/51) P = 0.018 |
| Shergill et al[23] | 160 (male 156, female 4) | Experienced | MEI, SC | MEI: 100% (65/65) SC: 97% (73/75) P = 0.19 | Mean ± SD MEI: 9.4 ± 5.7 SC: 8.5 ± 5.4 P = 0.31 | Not stated | Mean (SD) MEI: 3.06 (1.13) SC: 3.12 (1.22) P = 0.60 | Not stated |
The instruments used in the trials included the Olympus CF-1T200L scope (160 cm)[16,17], the ScopeGuide endoscope insertion tube system[18-20], the Olympus CF-Q160DI with the Olympus ScopeGuide system[15,21], the Olympus CF-Q180AL, the Olympus CF-Q160AL and the CF-Q140DL/I with the Olympus ScopeGuide system.
The experience levels of the endoscopists were evaluated either by years of experience (more than six years) or by the number of procedures performed (more than 200 procedures). In the retrieved articles, eight trials evaluated MEI procedures performed by experienced colonoscopists; while four studies evaluated MEI procedures performed by less experienced colonoscopists (four studies included both experienced and less experienced colonoscopists).
Among the eight RCTs that were included in this meta-analysis, an allocation sequence was generated using a computer-generated random number table[15-17,20,23]. Four of the eight trials reported adequate allocation concealment[15,20,21,23], while in another four trials, the allocation concealment was unclear. In all eight trials, all patients were blinded, but the endoscopists were not blinded in any of these trials because of the nature of the interventions.
The quality of the evidence for the outcomes in the included studies is shown in the Summary of Findings tables (Table 2).
| Outcomes | Illustrative comparative risks1 (95%CI) | Relative effect (95%CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard colonoscope | Magnetic endoscope imaging colonoscope | |||||
| Cecal intubation rate | Study population | OR = 1.92 (1.13-3.27) | 2945 (8 studies) | + + + -Moderate1 | ||
| 912 per 1000 | 952 per 1000(921 to 971) | |||||
| Moderate | ||||||
| 939 per 1000 | 967 per 1000(946 to 981) | |||||
| Cecal intubation time | The mean cecal intubation time in the intervention groups was 0.43 lower(0.13 lower to 0.28 higher) | 1934 (3 studies) | + + + +High1 | |||
Cecal intubation rate: There were eight research papers that reported on this topic. MEI with a colonoscope showed a higher cecal intubation rate compared with SC (OR = 1.92, 95%CI: 1.13-3.27, Figure 1A).
Cecal intubation time: Only three studies included the cecal intubation time, and all of these studies were included in the analysis. The meta-analysis of these three trials showed no significant difference in the cecal intubation time between MEI and SC (MD = -0.07, 95%CI: -0.16-0.02; Figure 1B). There was no heterogeneity among these three studies (I2 = 2%, P = 0.36).
Sedation dosage: Five studies reported the sedation dose used during the colonoscopic procedure. One trial used a patient-controlled analgesia (PCA) pump consisting of a mixture of midazolam and meperidine[17]; another one employed a combination of midazolam and pethidine[16]. Franciosi JP et al[19] reported the use of a mixture of midazolam and fentanyl[19], and Dechêne A et al[20] used midazolam, pethidine and propofol together. The other studies used midazolam, pethidine and diazepam[21].
Abdominal pain: Eight studies presented pain scores as the mean and standard deviation or median. However, the scales used for scoring pain were different. In two studies[18,19], a 0 to 10 score scale was used, and the other six studies used a 0 to 100 score scale, a 1 to 7 visual analogue scale, a validated questionnaire or abdominal compression[15-17,20,23]. Due to the differences in the scales, we did not pool the data for these studies.
Ancillary maneuvers: Four trials reported ancillary maneuvers during colonoscopy. Only two trials listed the amount of abdominal pressure applied, and only two trials reported the position changes made during colonoscopy; therefore, these data were not pooled for analysis.
A subgroup analysis was performed to evaluate the cecal intubation rate during colonoscopy according to the experience level of the endoscopists. The cecal intubation rate of MEI with experienced endoscopists was similar to that of SC (OR = 1.84, 95%CI: 0.97-3.48, seven trials, Figure 1C), while the chance of achieving cecal intubation was clearly higher with MEI than SC for inexperienced endoscopists (RR = 3.63, 95%CI: 1.96-6.74, three trials, Figure 1D).
The sensitivity analysis that excluded the studies with a small number of patients (less than 100) resulted in insignificant changes to the ORs and Weighted Mean Difference (WMDs). Additionally, we used the fixed-effect model to reanalyze all the data previously analyzed using the random-effect model. There were no significant changes to the ORs or RRs and WMDs when the fixed-effect model was used.
To detect publication bias, asymmetry was explored using a funnel plot. The distribution of the results of each study in the funnel plot excluded any potential publication bias.
The meta-analysis included eight RCTs published up to June 2012, including a total of 2967 participants who received MEI or SC. MEI has replaced X-ray imaging during colonoscopic procedures in many situations and therefore has a proven benefit for patients and staff[24-26]. MEI exhibited higher cecal intubation rates compared with standard colonoscopy but did not have any distinct advantage over standard colonoscopy in terms of cecal intubation time. Considering the potential advantage of real-time imaging, we were surprised to find that most of the individual studies showed no difference between the MEI and standard groups in the time required to reach the cecum but that the pooled data favored MEI. The increased sample size is the most likely explanation for the difference in the cecal intubation rate. A larger number of participants reduced the sampling error and directly affected the cecal intubation rate between MEI and SC. These results are meaningful in clinical practice. As is known, the failure rate of cecal intubation remains high in day-to-day SC. This means that part of the colon of some patients is not clearly visualized, which can prevent the early diagnosis and treatment of colonic diseases. MEI has increased the intubation rate and has made the early and accurate diagnosis of colonic issues, such as colorectal cancers, polyps and inflammatory bowel disease, possible.
The cecal intubation rate was also analyzed in two subgroups based on the experience level of the endoscopists (experienced and inexperienced). For inexperienced endoscopists, the MEI system appears to be advantageous. The cecal intubation rate for inexperienced endoscopists was higher in patients randomized to MEI than in the standard group. It is possible that inexperienced endoscopists are capable of identifying and minimizing loops with the continuous real-time imaging system. However, experienced endoscopists are likely able to recognize and resolve loops quickly without the need for MEI visualization. Therefore, whether MEI actually makes both inexperienced and experienced physicians better endoscopists remains to be determined.
The individual studies included in this meta-analysis showed concordance in the cecal intubation times between the two groups, and the pooled results for all trials also showed no significance.
There were four complications reported in two studies included in this meta-analysis[15,21], and they all occurred in the standard group. Three patients had a vasovagal reaction with rapid spontaneous recovery, and there was one case of bleeding following a polypectomy. To this point, no safety concerns have been raised with the use of MEI. During the procedure, precise judgment and caution are necessary, especially when advancing through a narrowed colon or pushing through loops.
A potential limitation of the meta-analysis is that these studies could not be performed in a way that would ‘blind’ the endoscopists to the scope used because of the nature of the interventions. Additionally, different models and manufacturers of MEI equipment were used in the studies included in the analysis. Finally, in several studies, specific patient subsets, such as colonic cancer patients and patients who had undergone prior colonic surgery, were excluded.
In conclusion, the present results indicated that the real-time magnetic imaging system is safe and beneficial in training and educating inexperienced endoscopists, as well as improving the cecal intubation rate for both experienced and inexperienced endoscopists. However, only a few studies have reported the advantages of MEI because it is a new technique, and further studies should be performed to confirm the role of the MEI colonoscope.
Colonoscopy is the gold standard and the most common and accurate tool for detecting important structural lesions of the lower gastrointestinal tract and diagnosing colonic diseases, such as polyps, colorectal cancer and inflammatory bowel disease. Magnetic endoscopic imaging (MEI) is a non-radiographic imaging technique that has been developed in recent years that is capable of displaying real-time three-dimensional images of the colonoscope shaft within the abdominal cavity. A pulsed low-magnetic field is sequentially produced by a series of electromagnetic generator coils spaced 10 cm apart along a catheter inserted through the accessory channe-l of the endoscope. The imager view is updated every 0.2 s to make the system essentially real-time, and the images are then recorded on a computer disk for subsequent replay or analysis.
The MEI system, when compared to standard colonoscopie (SC) with no visualization, has been shown to be beneficial in increasing the cecal intubation rate, reducing the number of attempts to straighten loops, and in reducing the duration of looping, especially with trainees. A few studies have compared MEI with SC; however, the results of these studies have not been uniform.
A few studies have compared MEI with SC; however, the results of these studies have not been uniform. Thus, this was the first meta-analysis to assess the theoretical advantages of MEI over SC and to compare the efficacies of MEI and SC. Through this study, we found that the real-time magnetic imaging system is of benefit in training and educating inexperienced endoscopists and improves the cecal intubation rate for experienced and inexperienced endoscopists.
The results indicated that the real-time magnetic imaging system is safe and of benefit in training and educating inexperienced endoscopists, as well as improving the cecal intubation rate for both experienced and inexperienced endoscopists.
The authors report a meta-analysis of trials that have compared MEI colonoscopy with standard colonoscopy for cecal intubation rates and cecal intubation times. Although colonoscopy supported by MEI was first reported in 1993, this technique has not been widely adopted either because it is expensive or because gastroenterologists are uncertain of its benefits.
P- Reviewers: Roy PK, Roberts-Thomson IC S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
| 1. | van Heijningen EM, Lansdorp-Vogelaar I, Kuipers EJ, Dekker E, Lesterhuis W, Ter Borg F, Vecht J, De Jonge V, Spoelstra P, Engels L. Features of adenoma and colonoscopy associated with recurrent colorectal neoplasia based on a large community-based study. Gastroenterology. 2013;144:1410-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Lin OS. Virtual colonoscopy: stamp of approval or word of warning? Lancet. 2013;381:1161-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Ausk KJ, Dominitz JA. Colonoscopy prevents colorectal cancer in both the right and left colon. Gastroenterology. 2011;141:393-396; discussion 396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Church JM. Complete colonoscopy: how often? And if not, why not? Am J Gastroenterol. 1994;89:556-560. [PubMed] |
| 5. | Mitchell RM, McCallion K, Gardiner KR, Watson RG, Collins JS. Successful colonoscopy; completion rates and reasons for incompletion. Ulster Med J. 2002;71:34-37. [PubMed] |
| 6. | Cardin F, Minicuci N, Andreotti A, Pinetti E, Campigotto F, Donà BM, Martella B, Terranova O. Maximizing the general success of cecal intubation during propofol sedation in a multi-endoscopist academic centre. BMC Gastroenterol. 2010;10:123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Korman LY, Overholt BF, Box T, Winker CK. Perforation during colonoscopy in endoscopic ambulatory surgical centers. Gastrointest Endosc. 2003;58:554-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 112] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Ker TS, Wasserberg N, Beart RW. Colonoscopic perforation and bleeding of the colon can be treated safely without surgery. Am Surg. 2004;70:922-924. [PubMed] |
| 9. | Misra SP. Colonoscopy. Endoscopy. 2004;36:957-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Makin GB, Breen DJ, Monson JR. The impact of new technology on surgery for colorectal cancer. World J Gastroenterol. 2001;7:612-621. [PubMed] |
| 11. | Bladen JS, Anderson AP, Bell GD, Rameh B, Evans B, Heatley DJ. Non-radiological technique for three-dimensional imaging of endoscopes. Lancet. 1993;341:719-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 39] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Leung FW. Magnetic endoscope imaging colonoscope: a new modality for hypothesis testing in unsedated colonoscopy. Gastrointest Endosc. 2012;75:1037-1039.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Williams C, Guy C, Gillies D, Saunders B. Electronic three-dimensional imaging of intestinal endoscopy. Lancet. 1993;341:724-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Sathyanarayana S, Schär M, Kraitchman DL, Bottomley PA. Towards real-time intravascular endoscopic magnetic resonance imaging. JACC Cardiovasc Imaging. 2010;3:1158-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Hoff G, Bretthauer M, Dahler S, Huppertz-Hauss G, Sauar J, Paulsen J, Seip B, Moritz V. Improvement in caecal intubation rate and pain reduction by using 3-dimensional magnetic imaging for unsedated colonoscopy: a randomized trial of patients referred for colonoscopy. Scand J Gastroenterol. 2007;42:885-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Shah SG, Brooker JC, Williams CB, Thapar C, Saunders BP. Effect of magnetic endoscope imaging on colonoscopy performance: a randomised controlled trial. Lancet. 2000;356:1718-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Shah SG, Brooker JC, Thapar C, Suzuki N, Williams CB, Saunders BP. Effect of magnetic endoscope imaging on patient tolerance and sedation requirements during colonoscopy: a randomized controlled trial. Gastrointest Endosc. 2002;55:832-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Cheung HY, Chung CC, Kwok SY, Tsang WW, Li MK. Improvement in colonoscopy performance with adjunctive magnetic endoscope imaging: a randomized controlled trial. Endoscopy. 2006;38:214-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Franciosi JP, Mascarenhas M, Semeao E, Flick J, Kelly J, Mamula P. Randomised controlled trial of paediatric magnetic positioning device assisted colonoscopy: a pilot and feasibility study. Dig Liver Dis. 2009;41:123-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Dechêne A, Jochum C, Bechmann LP, Windeck S, Gerken G, Canbay A, Zöpf T. Magnetic endoscopic imaging saves abdominal compression and patient pain in routine colonoscopies. J Dig Dis. 2011;12:364-370. [PubMed] [DOI] [Full Text] |
| 21. | Holme Ö, Höie O, Matre J, Stallemo A, Garborg K, Hasund A, Wiig H, Hoff G, Bretthauer M. Magnetic endoscopic imaging versus standard colonoscopy in a routine colonoscopy setting: a randomized, controlled trial. Gastrointest Endosc. 2011;73:1215-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Coderre S, Anderson J, Rikers R, Dunckley P, Holbrook K, McLaughlin K. Early use of magnetic endoscopic imaging by novice colonoscopists: improved performance without increase in workload. Can J Gastroenterol. 2010;24:727-732. [PubMed] |
| 23. | Shergill AK, McQuaid KR, Deleon A, McAnanama M, Shah JN. Randomized trial of standard versus magnetic endoscope imaging colonoscopes for unsedated colonoscopy. Gastrointest Endosc. 2012;75:1031-1036.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Mazzei MA, Guerrini S, Cioffi Squitieri N, Imbriaco G, Chieca R, Civitelli S, Savelli V, Mazzei FG, Volterrani L. Magnetic resonance imaging: is there a role in clinical management for acute ischemic colitis? World J Gastroenterol. 2013;19:1256-1263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Mezzi G, Arcidiacono PG, Carrara S, Perri F, Petrone MC, De Cobelli F, Gusmini S, Staudacher C, Del Maschio A, Testoni PA. Endoscopic ultrasound and magnetic resonance imaging for re-staging rectal cancer after radiotherapy. World J Gastroenterol. 2009;15:5563-5567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Zhang S, Peng JW, Shi QY, Tang F, Zhong MG. Colorectal neoplasm: magnetic resonance colonography with fat enema-initial clinical experience. World J Gastroenterol. 2007;13:5371-5375. [PubMed] |