INTRODUCTION
Endoscopic submucosal dissection (ESD) was originally developed in Japan as a method of endoscopic “en bloc” resection of superficial gastric cancers. Today, ESD is increasingly used for superficial esophageal cancers and esophageal submucosal tumors (SMTs)[1,2]. With improved ESD technology, it has been used not only for tumors, but also for functional disorders, and has produced good therapeutic effects. In this review, an outline of the current status of minimally invasive endoscopic therapy based on ESD for esophageal diseases is described.
ESD
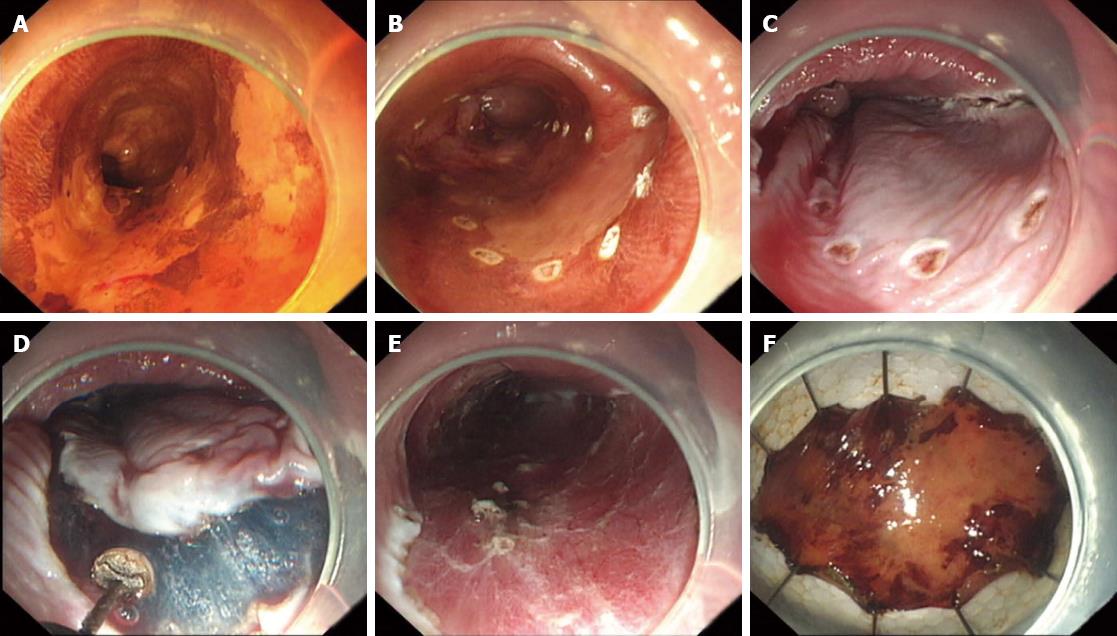
As with candidates suffering from other gastrointestinal tract diseases, patients scheduled for esophageal ESD are assessed using two factors: a small likelihood of lymph node metastasis and technical resectability[3,4]. ESD for lesions in esophageal squamous epithelium is performed as outlined in Figure 1. The lesion is dyed with 2% Lugol’s solution to obtain a clear margin, and several marker dots are made approximately 5-10 mm from the margin of the lesion using argon plasma coagulation (APC). After injection of several milliliters of injection solution into the submucosal layer, the mucosa is incised outside the marker dots with an electric knife (IT knife, hook knife, or HybridKnife). The submucosal tissue underneath the lesion is then gradually dissected with the electric knife. The solution is injected repeatedly, when necessary, during the dissection. Exposed vessels on the artificial ulcer are coagulated with APC or coagulation forceps to prevent delayed bleeding, and metallic clips are always used to close the deeply dissected areas. Although numerous injection solutions have been proposed and tested, saline is the most commonly used in the clinic due to its low cost and ease of use. Indigo carmine is added to obtain a clear layer and epinephrine is used to reduce bleeding. Hyaluronic acid is also used to improve submucosal lift durations[5-7].
Figure 1 Process of endoscopic submucosal dissection.
A: The lesion is dyed with 2% Lugol's solution; B: Marking of the lesion by argon plasma coagulation probes; C: Submucosal injection; D: The mucosa is incised outside the marker dots, and then the submucosal tissue underneath the lesion is gradually dissected; E: The wound after resection; F: The lesion.
ENDOSCOPIC SUBMUCOSAL EXCAVATION
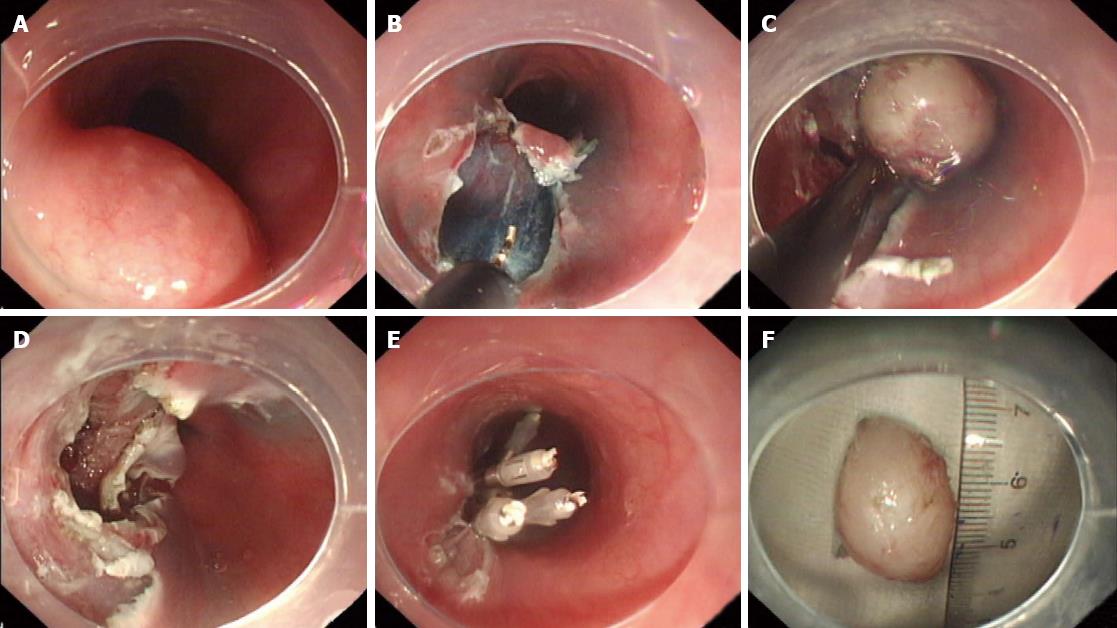
With improved ESD technology, ESD is not only used for mucous layer tumors, but also for muscularis propria tumors of the digestive tract. During this process, ESD is used to remove the submucosa muscularis propria of the tumor and to peel the tumor from the muscularis propria. We consider this application a new technology and named it endoscopic submucosal excavation (ESE). ESE is performed as outlined in Figure 2: (1) Marker dots are made approximately 5 mm away from the lesion; (2) Using a 23-gauge disposable needle, several milliliters of submucosal injection solution are injected around the lesion to lift it off the muscularis propria layer, but only the mucosa is lifted, not the tumor. This step shows that the tumor has originated from the muscularis propria layer; (3) The mucosa is then incised outside the marker dots using the electric knife; (4) The submucosal connective tissue beneath the lesion is gradually dissected from the muscularis propria layer with the electric knife to show the lesion; and (5) The electric knife is used to peel the muscularis propria layer along the edge of the lesion. Finally, the lesion is resected completely from the muscularis propria layer using the electric knife[8,9].
Figure 2 Process of endoscopic submucosal excavation.
A: A round-shaped submucosal tumor; B: Removal of the mucosa; C: Dissecting the tumor from the muscular layer; D: The wound after resection; E: Sealing the wound with metallic clips; F: The lesion.
SUBMUCOSAL TUNNELING ENDOSCOPIC RESECTION
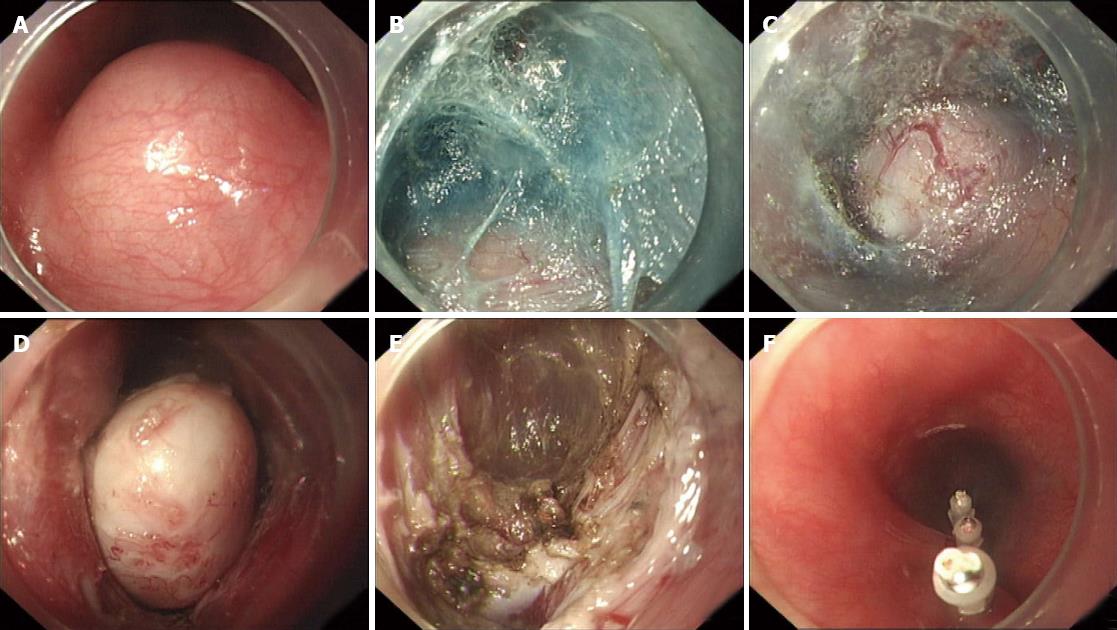
ESE was developed to allow en bloc resection of SMTs which originated from the muscularis propria layer under direct vision. However, the surgical area in the esophagus is limited and the esophageal adventitia is very thin. If perforation occurs and the mucosal defect cannot be completely closed, serious complications such as esophageal fistula will occur. We performed a new endoscopic technique for the treatment of SMTs, called submucosal tunneling endoscopic resection (STER), which can reduce the risk of postoperative GI tract leakage and secondary infection. The procedure for STER is as follows: (1) Submucosal injection of diluted indigo carmine or methylene blue is needed to locate SMTs in the cardia when they are difficult to identify; (2) A submucosal tunnel is created to expose the tumor. A fluid cushion is obtained using an injection needle 5 cm proximal to the SMT. A 2-cm, longitudinal mucosal incision is made using the electric knife at the esophageal mucosa as the entry point. A submucosal longitudinal tunnel is created with the electric knife between the submucosal and muscular layers. Tunneling ends 1-2 cm distal to the tumor to ensure a satisfactory endoscopic view of the SMT and enough working space for resection; (3) Resection of the SMT is performed under direct endoscopic visualization. During the procedure, safe and complete resection of the tumor, without interruption of the tumor capsule, is the highest priority; and (4) Closure of the mucosal incision site. After tumor resection and hemostasis with APC or hot biopsy forceps in the tunnel, the gastroscope is withdrawn through the natural orifice. Most commonly, the mucosal incision site is closed with 4 to 6 hemostatic clips[10,11] (Figure 3).
Figure 3 Process of submucosal tunneling endoscopic resection.
A: The tumor; B: A submucosal tunnel was created; C: Revealing the submucosal tumor; D: Dissecting the tumor from the muscular layer in the submucosal tunnel; E: The wound after resection; F: Closure of the mucosal incision site with clips.
PERORAL ENDOSCOPIC MYOTOMY
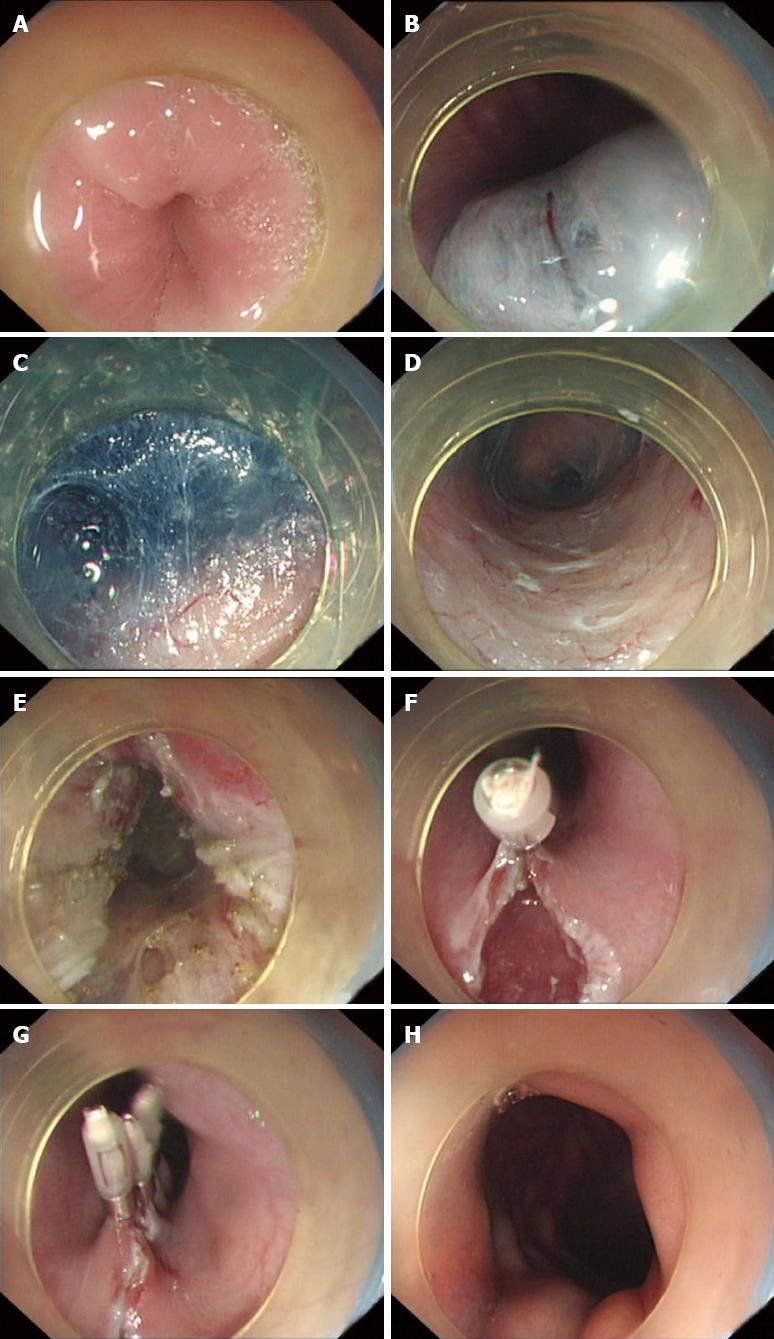
Peroral endoscopic myotomy has recently been described as a scarless and less invasive surgical myotomy option for the treatment of achalasia[12,13]. Briefly, submucosal injection and an initial mucosal incision are first performed at the 5- to 6-o’clock position on the posterior esophagus, approximately 10 cm proximal to the esophagogastric junction (EGJ). A submucosal tunnel is created passing over the EGJ and approximately 3 cm into the proximal stomach. The myotomy is initiated 2 cm distal to the mucosal entry point, approximately 6-8 cm above the EGJ, and is extended for a distance of 2-3 cm toward the stomach. After careful hemostasis, the mucosal incision site is closed with 4 to 6 hemostatic clips[14-16] (Figure 4).
Figure 4 Process of peroral endoscopic myotomy.
A: The esophagogastric junction (EGJ) before surgery; B: Submucosal injection and an initial mucosal incision; C-D: A submucosal tunnel was created; E: The muscle was incised; F-G: The mucosal incision site was closed with clips; H: EGJ after surgery.
THORACOSCOPE-ASSISTED TUNNEL ENDOSCOPIC RESECTION
With the development of ESD technology, endoscopy is used to treat large esophageal SMTs. Thus, endoscopic treatment is risky and of limited value in patients with huge esophageal or extraluminal SMTs. Minimally invasive thoracoscopic treatment also has its advantages, however, for esophageal SMTs larger than 3 cm, use of the thoracoscope involves a risk of tearing the mucosa when separating tumors, causing serious complications such as GI leakage. Laparoscopic-endoscopic cooperative surgery has been introduced[17,18]. Recently, we developed combined thoracoscopic and endoscopic therapy to treat esophageal SMTs originating from the muscularis propria. The indications for thoracoscope-assisted tunnel endoscopic resection are: (1) Tumors larger than 5 cm; and (2) U-shaped tumors larger than 3 cm and which extend to more than 1/2 of the esophagus circumference. This type of tumor is difficult to treat by endoscopic or thoracoscopic treatment alone. The detailed steps of this procedure are as follows: The patient lies in the left lateral position, the thoracoscope is introduced and any adhesion or pleural effusion in the pleural cavity is checked; (1) Thoracoscopic exploration of the tumor; (2) Submucosal injection is administered and a submucosal tunnel is created to expose the tumor using the ESD technique under endoscopy, which is the same as the STER procedure; (3) If the tumor is so large that it can not be removed from the tunnel by endoscopy, the thoracoscopic electric hook is used to separate the esophagus and open the muscular layer over the tumor by blunt dissection. In addition, the submucosal “tunnel” is under surveillance by endoscopy to avoid esophageal mucosa injury; (4) Under endoscopic surveillance in the submucosal tunnel, the esophageal muscular layer is sutured by thoracoscopy, and insufflation in the tunnel is performed to observe whether there is any leakage in the thoracic cavity. The endoscope is withdrawn from the submucosal tunnel after hemostasis and metallic clips are used to close the mucosal entry; (5) Endoscopy is used to identify mucosal rupture. The esophagus is insufflated to observe any leakage in the thoracic cavity and then thoracoscopy is used to suture the pleura mediastinalis; and (6) A drainage tube is placed in the chest cavity if there is no obvious bleeding[19] (Figure 5).
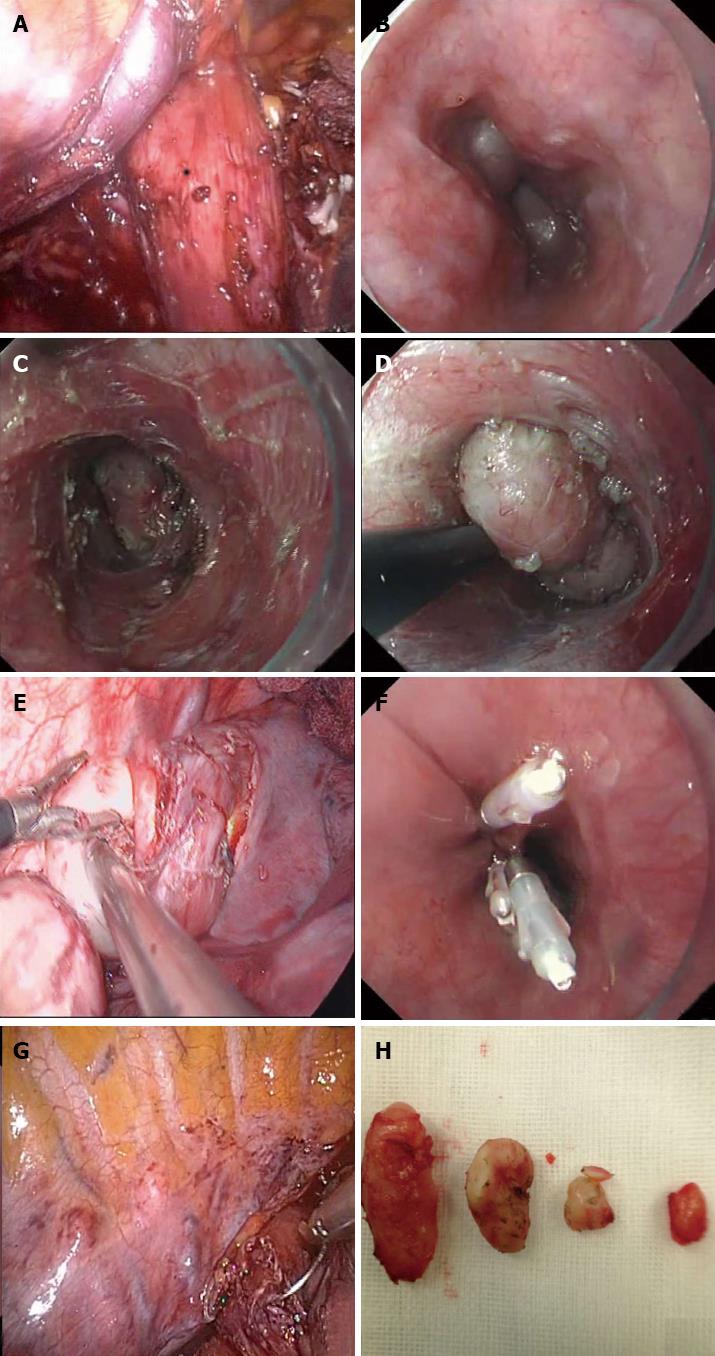
Figure 5 Process of thoracoscope-assisted tunnel endoscopic resection.
A: Thoracoscopic exploration of the tumor; B: Endoscopic exploration of the tumor; C-D: A submucosal tunnel was created to expose the tumor under endoscopy, which was the same as the submucosal tunneling endoscopic resection procedure; E: The thoracoscopic electric hook was used to separate the esophagus and open the muscular layer over the tumor by blunt dissection, we removed the large tumor from the chest; F: Use of metallic clips to close the mucosal entry; G: Use of thoracoscopy to suture the pleura mediastinalis; H: The lesions.
The main complications consist of bleeding, perforation and esophageal stricture, most of which were treated by endoscopy and surgery was not required[20-22]. With the development of endoscopic techniques and the improvement in people’s health consciousness, the model of the diagnosis and treatment of some esophageal diseases is changing. Patients benefit from minimally invasive endoscopic therapy based on ESD, which results in reduced pain, rapid resumption of normal activity, and shorter hospital stay.
P- Reviewers: Ciaccio EJ, Kobayashi N, Toyokawa T S- Editor: Qi Y L- Editor: Webster JR E- Editor: Ma S