Published online Oct 14, 2013. doi: 10.3748/wjg.v19.i38.6505
Revised: July 24, 2013
Accepted: August 20, 2013
Published online: October 14, 2013
Processing time: 116 Days and 20.5 Hours
A patient with stent embedding after placement of an esophageal stent for an esophagobronchial fistula was treated with an ST-E plastic tube inserted into the esophagus to the upper end of the stent using gastroscopy. The gastroscope was guided into the esophagus through the ST-E tube, and an alligator forceps was inserted into the esophagus through the ST-E tube alongside the gastroscope. Under gastroscopy, the stent wire was grasped with the forceps and pulled into the ST-E tube. When resistance was met during withdrawal, the gastroscope was guided further to the esophageal section where the stent was embedded. Biopsy forceps were guided through a biopsy hole in the gastroscope to the embedded stent to remove silicone membranes and connection threads linking the Z-shaped wire mesh. While the lower section of the Z-shaped stent was fixed by the biopsy forceps, the alligator forceps were used to pull the upper section of the metal wire until the Z-shaped metal loops elongated. The wire mesh of the stent was then removed in stages through the ST-E tube. Care was taken to avoid bleeding and perforation. Under the assistance of an ST-E plastic tube, an embedded esophageal metal stent was successfully removed with no bleeding or perforation. The patient experienced an uneventful recovery after surgery. Plastic tube-assisted gastroscopic removal of embedded metal stents can be minimally invasive, safe, and effective.
Core tip: A patient presented with a disordered stent structure as a result of failure of repeated attempts at gastroscopic removal. An ST-E tube was inserted into the esophagus. An alligator forceps was inserted into the ST-E tube alongside a gastroscope. The stent wire was gripped and pulled up into the tube. Biopsy forceps were inserted into the lower section of the stent through the biopsy hole to fix the stent, while the alligator forceps continued to be used to pull up the stent wire until the Z-shaped metal loops became elongated stripes. All the stent wire was removed through the ST-E tube.
- Citation: Peng GY, Kang XF, Lu X, Chen L, Zhou Q. Plastic tube-assisted gastroscopic removal of embedded esophageal metal stents: A case report. World J Gastroenterol 2013; 19(38): 6505-6508
- URL: https://www.wjgnet.com/1007-9327/full/v19/i38/6505.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i38.6505
The use of fully covered self-expandable esophageal metal stents has favorable results in treating a variety of benign and malignant esophageal strictures and esophageal fistulae[1-6]. However, stent placement over a prolonged period can result in hyperplastic tissue overgrowth on both ends of the stent, leading to in-stent re-stenosis[7-9]. Therefore, stents should be removed after an appropriate period after treatment of benign esophageal strictures and fistulae[10-12]. Notable tissue hyperplasia can occur at both stent ends, causing difficulty in stent removal and sometimes requiring surgical treatment. This procedure has a high risk of trauma[13,14]. Therefore, a minimally invasive, low-risk method is needed for removal of embedded esophageal stents. Here, we report our experience with a novel approach to gastroscopic removal of an embedded esophageal stent.
The patient was a 15-year-old girl who had experienced coughing after drinking since early March 2012. The imaging of iodinated contrast-enhanced radiological examination showed an esophagobronchial fistula arising from the left bronchus to the middle portion of the esophagus. Under gastroscopy on May 30, 2012, a fully covered Z-shaped metal stent measuring 2 cm × 6 cm was placed within the esophagus to cover the fistula opening. After the procedure, the coughing after drinking disappeared. However, the patient developed esophageal obstruction. Gastroscopy on August 13, 2012 showed tissue hyperplasia on both stent ends, luminal stenosis, and embedding of both stent ends in the hyperplastic tissue.
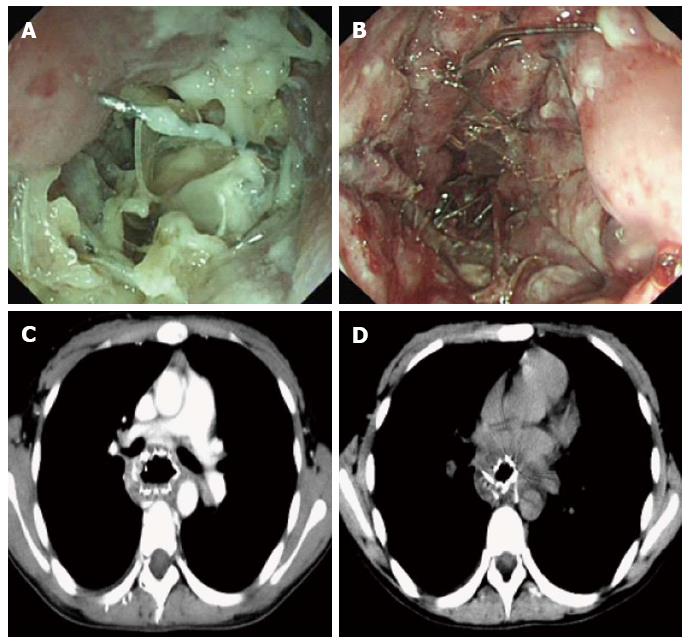
Attempts to remove the stent under endoscopy failed and led to a disorganized stent structure. Enhanced chest computed tomography scan showed the wall of the middle and inferior segment of the esophagus were noticeably thickened. Part of the stent was embedded in the esophageal wall, the boundary between the stent and surrounding fat was blurred, and the upper end of the stent was pressed against the trachea carina (Figure 1). After consultation with thoracic surgeons, we decided to perform gastroscopic removal on August 31, 2012.
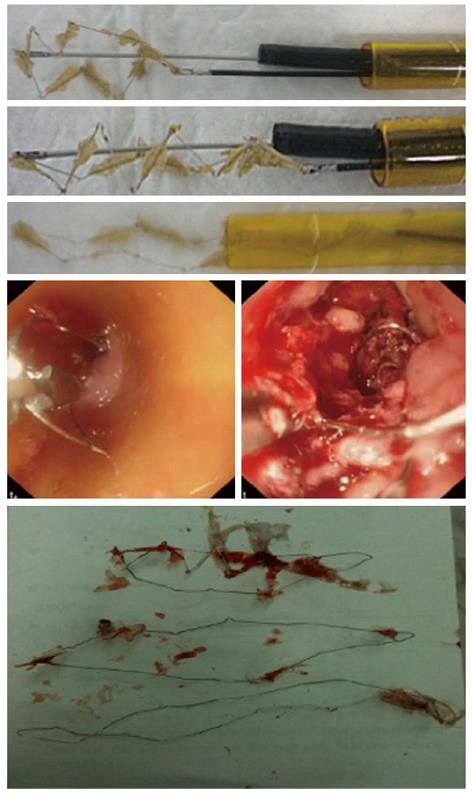
Under the guidance of gastroscopy, an ST-E plastic tube (3 cm × 40 cm) was inserted into the esophagus to the upper end of the stent. A gastroscope was guided into the esophagus through the ST-E tube, and an alligator forceps was inserted into the esophagus through the ST-E tube alongside the gastroscope. Under gastroscopy, the stent wire was gripped with the forceps and pulled into the ST-E tube. When resistance was met during withdrawal, the gastroscope was guided further to the esophageal section where the stent was embedded. Biopsy forceps were sent through a biopsy hole in the gastroscope and inserted near the embedded stent to remove the silicone membranes and connection threads linking the Z-shaped stent wire. Next, while the lower section of the Z-shaped stent was fixed by the biopsy forceps, the alligator forceps were used to pull the upper section of the metal wire until the Z-shaped metal loops elongated. The wire mesh of the stent was then removed in stages through the ST-E tube (Figure 2).
Benign esophagobronchial fistulae are rare and often result from trauma, esophageal spontaneous rupture, tuberculosis, and Crohn’s disease[2,4,5]. Treatment is usually difficult and surgical interventions involve a high risk of trauma. Placement of fully covered self-expanding metal stents has become a viable treatment option. However, stent placement over a prolonged period can result in hyperplastic tissue overgrowth on both ends of the stent, leading to in-stent re-stenosis. Removing embedded stents is difficult. One study attempted to remove a stent by placing a secondary stent within the primary stent[15]. However, in this case, the stent structure was compromised and became disordered during attempts to remove the stent under endoscopy, with the result that sharp parts of the stent were entering the esophageal wall. Thus, placement of another stent might have caused esophageal perforation and damage to surrounding organs.
In our view, two goals must be achieved to successfully remove a structurally disordered Z-shaped metal stent embedded in the esophageal wall under gastroscopy. First, the esophageal entrance and throat must be protected from scratching by the stent wire during removal; second, each of the Z-shaped stent loops needs to be pulled outward until it is elongated. Gastroscopic procedures conducted through a ST-E tube meet these requirements, as the plastic tube fully protects the upper portion of the esophagus and throat from scratching by the stent wire. A two-handed operation is possible with an ST-E tube: with one hand, an alligator forceps is inserted into the esophagus through the ST-E tube alongside the gastroscope. Under the guidance of gastroscopy, the stent wire is gripped and pulled outward into the ST-E tube. If resistance is met during pulling, the gastroscope can be sent further to the esophageal section where the stent is embedded and biopsy forceps guided with the second hand through a biopsy hole in the gastroscope to insert into the embedded stent to remove silicone membranes and connection threads linking the Z-shaped stent. While the lower section of the Z-shaped stent is fixed by the biopsy forceps, the alligator forceps can be used to pull the upper section of the metal wire until the Z-shaped metal loops are elongated, to enable the wire mesh of the stent to be removed through the ST-E tube. The wire mesh of the stent is removed in stages by repeating the above procedures.
In our view, plastic tube-assisted gastroscopy is a minimally invasive, safe, and effective method for removal of esophageal embedded metal stents.
We got the study approval for the paper from Southwest Hospital.
P- Reviewer Fan XM S- Editor Wen LL L- Editor O’Neill M E- Editor Zhang DN
| 1. | Adler DG, Fang J, Wong R, Wills J, Hilden K. Placement of Polyflex stents in patients with locally advanced esophageal cancer is safe and improves dysphagia during neoadjuvant therapy. Gastrointest Endosc. 2009;70:614-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | van Heel NC, Haringsma J, Spaander MC, Bruno MJ, Kuipers EJ. Short-term esophageal stenting in the management of benign perforations. Am J Gastroenterol. 2010;105:1515-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 3. | Bakken JC, Wong Kee Song LM, de Groen PC, Baron TH. Use of a fully covered self-expandable metal stent for the treatment of benign esophageal diseases. Gastrointest Endosc. 2010;72:712-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Blackmon SH, Santora R, Schwarz P, Barroso A, Dunkin BJ. Utility of removable esophageal covered self-expanding metal stents for leak and fistula management. Ann Thorac Surg. 2010;89:931-936; discussion 931-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Leers JM, Vivaldi C, Schäfer H, Bludau M, Brabender J, Lurje G, Herbold T, Hölscher AH, Metzger R. Endoscopic therapy for esophageal perforation or anastomotic leak with a self-expandable metallic stent. Surg Endosc. 2009;23:2258-2262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Vakil N, Morris AI, Marcon N, Segalin A, Peracchia A, Bethge N, Zuccaro G, Bosco JJ, Jones WF. A prospective, randomized, controlled trial of covered expandable metal stents in the palliation of malignant esophageal obstruction at the gastroesophageal junction. Am J Gastroenterol. 2001;96:1791-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Jaganmohan S, Raju GS. Tissue ingrowth in a fully covered self-expandable metallic stent (with videos). Gastrointest Endosc. 2008;68:602-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Fukuda T, Hirota S, Matsumoto S, Yoshikawa T, Motohara T, Nishida Y, Sugimura K. Periodic endoscopic observation of postoperative esophageal stricture due to excessive tissue hyperproliferation after stent placement. Gastrointest Endosc. 2001;53:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Vakil N, Gross U, Bethge N. Human tissue responses to metal stents. Gastrointest Endosc Clin N Am. 1999;9:359-365. [PubMed] |
| 10. | Dua KS, Vleggaar FP, Santharam R, Siersema PD. Removable self-expanding plastic esophageal stent as a continuous, non-permanent dilator in treating refractory benign esophageal strictures: a prospective two-center study. Am J Gastroenterol. 2008;103:2988-2994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 11. | Repici A, Conio M, De Angelis C, Battaglia E, Musso A, Pellicano R, Goss M, Venezia G, Rizzetto M, Saracco G. Temporary placement of an expandable polyester silicone-covered stent for treatment of refractory benign esophageal strictures. Gastrointest Endosc. 2004;60:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 147] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 12. | Siersema PD. Stenting for benign esophageal strictures. Endoscopy. 2009;41:363-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Sharma P, Kozarek R. Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol. 2010;105:258-273; quiz 274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 210] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 14. | Langer FB, Schoppmann SF, Prager G, Riegler FM, Zacherl J. Solving the problem of difficult stent removal due to tissue ingrowth in partially uncovered esophageal self-expanding metal stents. Ann Thorac Surg. 2010;89:1691-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Hirdes MM, Siersema PD, Houben MH, Weusten BL, Vleggaar FP. Stent-in-stent technique for removal of embedded esophageal self-expanding metal stents. Am J Gastroenterol. 2011;106:286-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |