Published online Oct 14, 2013. doi: 10.3748/wjg.v19.i38.6465
Revised: July 28, 2013
Accepted: August 16, 2013
Published online: October 14, 2013
Processing time: 145 Days and 22.1 Hours
AIM: To explore the association between consumption of spicy foods and prevalence of irritable bowel syndrome (IBS) among Iranian adults.
METHODS: In this cross-sectional study, data from 4763 Iranian adult participants were used. Consumption of spicy foods was estimated using a dietary habits questionnaire that included a question on spicy foods consumption: “how frequently do you use spicy foods (pepper, curry, ginger, cinnamon and turmeric) during a week?” Participants could respond to the question by choosing one of these choices: never, 1-3 times, 4-6 times, 7-9 times, or more than 10 times per week. A modified Persian version of the Rome III questionnaire was used to determine the prevalence of IBS.
RESULTS: IBS was prevalent in 21.7% (18.6% of men and 24.1% of women) of the study population. After controlling for potential confounders including dietary behaviors, those consuming spicy foods ≥ 10 times per week were 92% more likely to have IBS compared with those who never consumed spicy foods (OR = 1.92; 95%CI: 1.23-3.01, Ptrend < 0.01). The association remained significant even after taking lactose intolerance into account (OR = 1.85; 95%CI: 1.18-2.90, Ptrend < 0.01). Stratified analysis by gender revealed that the association between consumption of spicy foods and IBS was not significant in men; however, a significant association was found among women after taking potential cofounders, including meal regularity and lactose intolerance, into account. Women who consumed spicy foods ≥ 10 times per week were two times more likely to have IBS compared with those who never consumed spicy foods (OR = 2.03; 95%CI: 1.09-3.77, Ptrend = 0.02).
CONCLUSION: Consumption of spicy foods is directly associated with IBS, particularly in women. Further, prospective studies are warranted to (1) examine this association in other populations; and (2) evaluate whether dietary interventions, for example a reduction in spice consumption, would improve IBS symptoms.
Core tip: The role of dietary habits, including consumption of spicy foods, in the development of functional gastrointestinal disorders remains controversial. In this cross-sectional study in a large sample of Iranian adults, we found that women with high consumption of spicy foods had a two-fold increased risk of developing irritable bowel syndrome compared with women who reported not to consume spicy foods. The results underline the need for further studies to characterize potential relationships between diet-related practices and the risk of functional gastrointestinal disorders, in order to design appropriate, and effective, diet-based interventions.
- Citation: Esmaillzadeh A, Keshteli AH, Hajishafiee M, Feizi A, Feinle-Bisset C, Adibi P. Consumption of spicy foods and the prevalence of irritable bowel syndrome. World J Gastroenterol 2013; 19(38): 6465-6471
- URL: https://www.wjgnet.com/1007-9327/full/v19/i38/6465.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i38.6465
Functional gastrointestinal disorders (FGIDs) are characterized by chronic and recurrent gastrointestinal (GI) symptoms with ambiguous pathophysiology[1]. The most common FGID is irritable bowel syndrome (IBS), which is characterized by abdominal pain and changes in stool consistency and/or frequency[2-5]. It has been estimated that 5%-10% of the adult population in Asian countries[6] and 10%-20% of the population in developed countries[7] are affected by IBS. In Iran, the prevalence of IBS has been reported to be 1.1%-25% based on different studies[8]. Since there is no established medical therapy to alter the natural history of IBS in the longer term, the disorder represents a considerable financial burden to the health service, owing to medical consultations and consumption of other valuable resources[9].
Diet appears to play an important role in the etiology of FGIDs[10-12]. Dietary intake of carbohydrates and fatty foods along with caffeine, alcohol and spices have been linked to IBS[13,14]. Consumption of other foods and nutrients has also been implicated in the induction of symptoms in IBS[15-20]. Some studies have suggested that IBS symptoms might result from food sensitivities rather than altered diet composition[10].
The consumption of spicy foods has received attention in relation to FGIDs[21,22]. Earlier studies have shown that chili, with its pungent ingredient, capsaicin, exacerbates abdominal pain and burning in IBS patients. In contrast, chronic consumption of chili has been found to result in an improvement in IBS-related symptoms[11]. Six-week administration of four pills per day each containing 150 mg of red pepper powder was reported to be effective in improving the intensity of abdominal pain in IBS patients[21]. Other studies have also reported the beneficial effects of spicy foods in the management of FGID symptoms[22]. However, most previous studies have focused on chili and its ingredients, and no information is available on other spicy foods. Furthermore, earlier investigations have mostly used high doses of spices as a treatment, and limited data are available examining the habitual consumption of spicy foods and its relationship to the prevalence of IBS.
The traditional Iranian diet contains large amounts of spicy foods, including turmeric, saffron, and ginger, providing an opportunity to assess consumption of spicy foods in relation to health. In addition, few data exist about the association between diet and FGIDs, and available evidence has mostly been reported from small samples, thus, no data are available from large populations. The Study on the Epidemiology of Psychological, Alimentary Health and Nutrition (SEPAHAN), which has been performed in a large group of Iranian adults, provides a unique opportunity to investigate the epidemiological aspects of FGIDs and their relationship with different lifestyles, including nutritional factors[23]. Here, we present the sub-study that aimed to explore the association between consumption of spicy foods and the prevalence of IBS among Iranian adults.
This cross-sectional study was carried out within the framework of the SEPAHAN project. This project was conducted in two main phases in a large sample of Iranian adults working in 50 different healthcare centers across Isfahan province, Iran[23]. In the first phase of SEPAHAN, questionnaires on demographic information, medical history, anthropometric measures, lifestyle and nutritional factors were sent to 10087 persons, and 8691 subjects returned the completed questionnaires (response rate: 86.16%). In the second phase, another set of questionnaires was sent out to obtain data on gastrointestinal health of participants. After linking data from both phases and considering missing data, 4763 people who provided complete information on diet and FGIDs were included in the current analysis. The Bioethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran, approved the study.
We used a dietary habits questionnaire that contained detailed questions about meal frequencies, regularity of meals and drinking fluids before and after meals, as well as a question relating to the consumption of spicy foods: “how often do you use spicy foods (chili pepper, curry, ginger, cinnamon, and turmeric) during a week?” Participants could respond to this question by choosing one of the following choices: never, 1-3 times, 4-6 times, 7-9 times, or more than 10 times per week. Responses to this question were used as the main exposure variable in the current study.
A modified Persian version of the Rome III questionnaire, as part of the main comprehensive questionnaire, was used for the identification of FGIDs, including IBS[23]. During the face validation of the questionnaire, we found that most participants were unable to distinguish between the descriptors used in the original Rome III questionnaire (never, less than one day a month, one day a month, two to three days a month, one day a week, more than one day a week, every day). We, therefore, modified the rating scales to consist of only four descriptors (i.e., never or rarely, sometimes, often, always)[23]. Participants were also asked about the presence of each symptom in the previous three months. IBS was defined according to Rome III criteria as recurrent abdominal pain or discomfort at least sometimes in the previous 3 months associated with two or more of the following criteria: (1) improvement with defecation at least sometimes; (2) pain onset associated with a change in stool frequency; and (3) pain onset associated with a change in form (appearance) of stool at least sometimes.
Standard questionnaires were distributed to collect information on age, gender and educational status. Weight, height and the presence of diabetes mellitus were evaluated by a self-administered questionnaire. Data on smoking were collected through self-reported responses to the questionnaire and participants were categorized as non-smokers, ex-smokers and current smokers. The use of dietary supplements (yes/no) and oral contraceptive pills (OCP) (yes/no) as well as patterns of tea consumption (never or less than 1 cup/mo, 1-3 cups/mo, 1-3 cups/wk, 4-6 cups/wk, 1 cup/d, 2-4 cups/d, 5-7 cups/d, 8-11 cups/d, or at least 12 cups/d) were also assessed by a pre-tested questionnaire. Fluid intake was evaluated through questions on the consumption of water, soft drinks, yogurt drink (“dough”) and other beverages, before, after or during meals, which participants could answer as never, sometimes, often, or always. Regularity of meals was also assessed and quantified as never, sometimes, often, or always having regular meals. Study subjects were also categorized in terms of dental status as fully dentate, lost 1-3 teeth, lost 4-5 teeth, or lost half or more teeth. Quality of chewing was also evaluated (How thoroughly do you chew food?), with responses including: not very well, well, or very well. We also asked participants to describe their feelings/symptoms after milk intake. Lactose intolerance was defined as the existence of abdominal pain, bloating, diarrhea or belching after milk consumption[24].
We categorized participants based on their reported frequency of consumption of spicy foods i.e., never, 1-3 times, 4-6 times, 7-9 times, or 10 times or more during a week. Comparison of continuous variables across different categories of spicy foods consumption was performed using one-way analysis of variance. Distribution of study participants in terms of categorical variables across different categories of intake of spicy foods was compared using χ2 test. To assess the relationship between spicy foods consumption and IBS, logistic regression analysis was performed in different models. First, we adjusted for age (continuous) and gender (categorical). We further controlled for smoking (non-smoker, ex-smoker and current smoker), dietary supplement (yes/no) and OCP use (yes/no), self-reported diabetes (yes/no) and body mass index (continuous) in the second model. Additional adjustments were made for meal regularity (never, sometimes, often and always), quality of chewing foods (not very well, well and very well), intra-meal fluid intake (never, sometimes, often and always), dental status (fully dentate, lost 1-3 tooth, lost 4-5 tooth, lost half or more tooth) and pattern of tea consumption (never or < 1 cup/mo, 1-3 cups/mo, 1-3 cups/wk, 4-6 cups/wk, 1 cup/d, 2-4 cups/d, 5-7 cups/d, 8-11 cups/d or at least 12 cups/d). In the final model, a further adjustment was made for lactose intolerance (yes/no). In all analyses, the category of never consuming spicy foods was considered as the reference category. To assess the trend of odds ratios across increasing categories of spicy foods intake, we applied Mantel-Haenszel extension chi-square. A stratified analysis by gender was also performed to examine gender-specific associations. All analysis was performed using SPSS version 16 (SPSS Corp, Chicago, IL, United States). P values less than 0.05 were considered statistically significant.
IBS was prevalent among 21.7% (18.6% of men and 24.1% of women) of the study population. General characteristics of study participants across different categories of spicy food consumption are summarized in Table 1. Those consuming spicy foods ≥ 10 times/wk were younger, had lower weight and were more likely to be women, married and highly educated compared with those who never consumed spicy foods. High consumption of spicy foods was associated with a lower prevalence of smoking and high prevalence of dietary supplement consumption and OCP use. There was no significant difference in the prevalence of self-reported diabetes among different groups of spicy food intake.
| Consumption of spicy foods (times/wk) | ||||||
| Never | 1-3 | 4-6 | 7-9 | ≥10 | 1P value | |
| Age (yr) | 38.0 ± 8.3 | 37.4 ± 8.4 | 36.5 ± 7.8 | 35.1 ± 7.3 | 33.9 ± 7.6 | < 0.001 |
| Weight (kg) | 70.3 ± 15.2 | 70.7 ± 13.4 | 68.2 ± 12 | 66.9 ± 14.0 | 65.4 ± 11.7 | < 0.001 |
| BMI (kg/m2) | 25.1 ± 5.3 | 25.2 ± 5.0 | 24.9 ± 4.0 | 25.0 ± 5.0 | 24.5 ± 3.8 | 0.16 |
| Female | 38.10% | 41.30% | 63.50% | 73.50% | 76.50% | < 0.001 |
| Marriage | 78.70% | 81.10% | 82.70% | 79.00% | 81.60% | 0.03 |
| University degree | 44.90% | 50.50% | 62.00% | 65.50% | 65.20% | < 0.001 |
| Current smokers | 6.30% | 4.20% | 4.00% | 1.40% | 1.60% | 0.01 |
| Supplement use | 4.10% | 6.10% | 8.30% | 9.10% | 9.80% | < 0.001 |
| OCP use | 1.00% | 1.60% | 3.00% | 4.70% | 4.40% | < 0.001 |
| Self-reported diabetes | 1.70% | 1.80% | 1.90% | 1.70% | 1.40% | 0.72 |
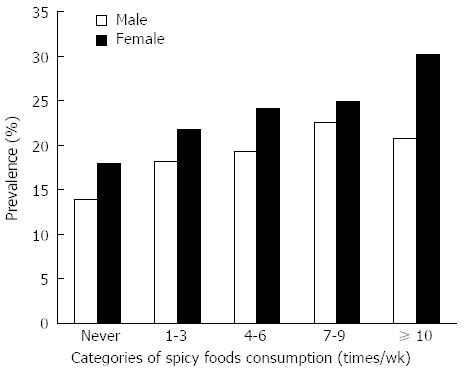
The prevalence of IBS across different categories of spicy foods consumption in the entire study population and each gender is shown in Figure 1. Consumption of spicy foods was associated with an increased prevalence of IBS among women, so that those consuming spicy foods ≥ 10 times/wk were more likely to have IBS compared with those who never consumed spicy foods (30.2% vs 18.0%, P < 0.05). A trend for greater prevalence of IBS with consumption of spicy foods was also seen in men; however, a slight drop in its prevalence was evident in the top category.
Multivariable adjusted odds ratio (OR) for IBS in the entire study population among different categories of spicy foods intake are illustrated in Table 2. Increased consumption of spicy foods was associated with a greater chance of having IBS in the crude model. After controlling for age and gender, those consuming spicy foods ≥10 times/wk were two times more likely to have IBS compared with those who never consumed spicy foods. The association remained significant even after taking other cofounders into account (OR = 1.92, 95%CI: 1.23-3.01). Further adjustment for dietary behaviors and lactose intolerance slightly attenuated the association, but it remained significant (OR = 1.85, 95%CI: 1.18-2.90).
| Consumption of spicy foods (times/wk) | Ptrend | |||||
| Never | 1-3 | 4-6 | 7-9 | ≥10 | ||
| Crude | 1.00 | 1.34 (0.95-1.88) | 1.57 (1.12-2.21) | 1.75 (1.21-2.52) | 2.12 (1.45-3.10) | < 0.001 |
| Model I | 1.00 | 1.35 (0.92-1.97) | 1.48 (1.00-2.18) | 1.58 (1.04-2.39) | 1.99 (1.30-3.06) | < 0.001 |
| Model II | 1.00 | 1.28 (0.87-1.88) | 1.44 (0.98-2.13) | 1.45 (0.95-2.20) | 1.94 (1.26- 2.98) | < 0.001 |
| Model III | 1.00 | 1.21 (0.81-1.80) | 1.35 (0.90-2.01) | 1.35 (0.87-2.07) | 1.92 (1.23-3.01) | < 0.01 |
| Model IV | 1.00 | 1.20 (0.80-1.78) | 1.33 (0.89-1.98) | 1.32 (0.86-2.03) | 1.85 (1.18-2.90) | < 0.01 |
Stratified analysis by gender revealed that the association between consumption of spicy foods and IBS was not significant in men, even after controlling for cofounders (Table 3); however, a significant association was found among women after taking potential cofounders, including meal regularity and lactose intolerance, into account. Those who consumed spicy foods ≥10 times/wk were twice as likely to have IBS compared with those who never consumed spicy foods (OR = 2.03, 95%CI: 1.09-3.77, Ptrend = 0.02).
| Consumption of spicy foods (times/wk) | Ptrend | |||||
| Never | 1-3 | 4-6 | 7-9 | ≥10 | ||
| Men | ||||||
| Crude | 1.00 | 1.38 (0.88-2.17) | 1.48 (0.92-2.37) | 1.81 (1.03-3.16) | 1.62 (0.85-3.08) | 0.07 |
| Model I | 1.00 | 1.32 (0.79-2.22) | 1.34 (0.78-2.31) | 1.78 (0.95-3.32) | 1.78 (0.87-3.60) | 0.10 |
| Model II | 1.00 | 1.27 (0.75-2.14) | 1.35 (0.78-2.33) | 1.69 (0.89-3.19) | 1.8 (0.88-3.67) | 0.17 |
| Model III | 1.00 | 1.16 (0.67-2.01) | 1.26 (0.71-2.24) | 1.55 (0.79-3.04) | 1.65 (0.78-3.48) | 0.22 |
| Model IV | 1.00 | 1.18 (0.68-2.05) | 1.27 (0.71-2.27) | 1.55 (0.79-3.04) | 1.64 (0.78-3.48) | 0.29 |
| Women | ||||||
| Crude | 1.00 | 1.26 (0.75-2.12) | 1.44 (0.87-2.40) | 1.5 (0.89-2.55) | 1.96 (1.14-3.37) | < 0.01 |
| Model I | 1.00 | 1.38 (0.78-2.43) | 1.58 (0.90-2.78) | 1.57 (0.87-2.81) | 2.14 (1.18-3.88) | < 0.01 |
| Model II | 1.00 | 1.32 (0.75-2.35) | 1.53 (0.87-2.68) | 1.43 (0.79-2.52) | 2.05 (1.12-3.73) | < 0.01 |
| Model III | 1.00 | 1.3 (0.72-2.33) | 1.45 (0.81-2.59) | 1.38 (0.75-2.52) | 2.13 (1.15-3.95) | 0.01 |
| Model IV | 1.00 | 1.26 (0.70-2.27) | 1.41 (0.79-2.52) | 1.34 (0.73-2.44) | 2.03 (1.09-3.77) | 0.02 |
We found that consumption of spicy foods was associated with increased prevalence of IBS among Iranian adults. This association remained significant even after adjustment for potential confounders, including dietary behaviors. After stratified analysis by sex, the associations remained significant only in women. To the best of our knowledge, our study is among the first population-based studies that assessed habitual intake of spicy foods as a major exposure variable in relation to IBS.
Associations between the consumption of spicy foods and FGIDs, including IBS, have been examined previously[11,13,14,21,22]. However, most studies have attempted to use spices to alleviate pain in these patients[4,25,26], and limited data are available on the relationship between habitual consumption of spicy foods and symptoms of IBS[11]. Furthermore, prior studies have mostly focused on pepper[11,13,14,21,22], and effects of other spicy foods on IBS remain to be identified. In the current study, we found a significant, and direct, association between consumption of spicy foods and IBS. Our findings are in line with a population-based study in China, which showed a significant association between excessive intake of pepper and prevalence of IBS in adolescents[14]. The link between spicy food consumption and IBS symptoms is also supported by an acute, meal-based study[27], in which administration of a standard meal containing 2 g chili, either mixed into the meal or given separately in capsules, caused more abdominal pain and burning in IBS patients than in healthy participants. In contrast, in other studies, ingestion of 4 enteric-coated pills per day (each containing 150 mg of capsaicin-equivalent) for 6 wk, significantly improved abdominal pain and bloating in IBS patients[21]; ginger was found to be the most common type of complementary and alternative medicine used for IBS treatment[4]; cinnamon administration has been found to reduce the number of IBS symptoms[25]; and beneficial effects of turmeric on abdominal pain and discomfort in IBS patients have also been reported[26]. While the causes for the discrepant study outcomes are not clear, there are a number of potential reasons. Different spices may have different modes of action; almost all studies that reported beneficial effects of individual spices used high doses in the form of supplements, and study designs and methodologies varied markedly between studies. It appears that the current study is the first observational study in an adult population, in which habitual consumption of spicy foods has been linked to IBS, although, due to the use of a single question to assess spicy food intake, it is not possible to distinguish between the potential effects of individual spices.
The mechanisms through which consumption of spicy foods might affect IBS are unknown. The effect of red pepper has been related to its pungent ingredient, capsaicin, which can modify gastrointestinal sensation via transient potential vanilloid 1 (TRPV1) receptors[11,27]. Increased TRPV1 receptors are associated with visceral hypersensitivity in the proximal gut and colon[11,27]. It seems that capsaicin intake in IBS patients can lead to hypersensitivity, which in turn can result in TRPV1 up-regulation[4,11,28]. However, few studies have postulated that intermittent and chronic ingestion of capsaicin or capsaicin containing chili can improve FGID symptoms by desensitization of TRPV1 receptors[11]. This can be explained by the action of capsaicin, which when administered chronically, depletes nerve terminals of substance P, while acute application leads to maximal release of transmitters, resulting in pain. Further research is required to prove this hypothesis. The mechanisms of other spices remain to be identified.
This study has several strengths. Firstly, it is a large population-based study, which examined habitual intake of spicy foods, rather than the effects of high doses of spices. Earlier studies have mostly been performed in small sample sizes. Secondly, we performed rigorous statistical analyses, including adjustments for several potential contributing factors to IBS. Therefore, the associations we identified are independent of many factors, including dietary behaviors. Nevertheless, the findings need to be interpreted in the light of some limitations. We used a pre-tested questionnaire for assessing dietary intakes of spicy foods; misclassification is a potential concern in our study as in any epidemiological studies. In addition, high consumption of spicy foods was associated with a complex pattern of lifestyles that may not have been accurately captured and controlled in our analysis, resulting in residual confounding. The significant direct association of spicy foods intake and IBS may be attributed to the other factors (e.g., having irregular meals, not chewing foods very well, etc.) associated with higher intake of these foods. That said, the apparently 1 direct effect of spicy food consumption persisted in multivariate models accounting for known potential confounders. Furthermore, some intermediate factors might lead to changes in diet and may, therefore, confound the association between spicy food intake and IBS. In addition, the observed association may not apply to other sections of the Iranian population, including the young, elderly or those from different socio-economic backgrounds. However, participants in the current study were selected from different areas of Isfahan province with diverse socioeconomic status and their dietary intakes covered a broad range of dietary habits. Given these characteristics, it is unlikely that this type of bias could explain the observed associations between spicy food intake and IBS.
In conclusion, we found evidence indicating that spicy food consumption was positively associated with IBS, particularly in women. Further studies, in particular of a prospective nature, are required to examine this association in more detail and to potentially develop novel dietary approaches to manage IBS and other FGIDs.
We wish to thank all staff of Isfahan University of Medical Sciences (MUI) who participated in our study. We also appreciate staff of the Public Relation Unit, MUI and other authorities of MUI for their excellent cooperation.
The relationship between dietary factors and irritable bowel syndrome (IBS) remains yet to be clearly defined. Some research suggests that carbohydrate, protein, fiber, or water all may play a role. However, currently there are many controversial findings regarding the relationship between diet-related practices and different gastrointestinal disorders including IBS.
While some studies have indicated that acute chili ingestion can aggravate abdominal pain and burning symptoms in functional gastrointestinal disorders, chronic ingestion of chili was found to improve functional dyspepsia and gastroesophogeal reflux disease symptoms in small controlled studies. It is worth noting that most previous studies focused on one type of spice (e.g., chili pepper), and there are few studies that have investigated the relationships between habitual intake of spicy foods and functional gastrointestinal disorders.
In a large cross-sectional study, information on habitual spicy food intake and symptoms related to IBS were gathered from 4763 adults using standard questionnaires. Individuals with a high intake of spicy foods (≥ 10 times/wk) had an almost two-fold increased risk of having IBS compared with those who reported a lower intake of spicy foods. After taking into account different variables that might distort the association between spicy food intake and IBS, the relationship was significant only among women.
The findings of the current study, if confirmed in well-designed prospective studies, may assist with the design of novel dietary therapies that take into account, and modify, the dietary intake of spicy foods and, thus, may be useful in the management of IBS related symptoms.
In this interesting manuscript, the authors explored the association between consumption of spicy foods and prevalence of IBS among Iranian adults. They performed a cross-sectional study from 4763 Iranian adult participants. Consumption of spicy foods was estimated using a dietary habits questionnaire, and the prevalence of IBS was estimated using a modified Persian version of the Rome III questionnaire. The study has concluded that consumption of spicy foods is directly associated with IBS, particularly in women. This article is interesting and the readers will get some beneficial information from this.
P- Reviewer Jiang M S- Editor Wen LL L- Editor O’Neill M E- Editor Zhang DN
| 1. | Corazziari E. Definition and epidemiology of functional gastrointestinal disorders. Best Pract Res Clin Gastroenterol. 2004;18:613-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 100] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 2. | Chang L. Review article: epidemiology and quality of life in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004;20 Suppl 7:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 245] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 3. | Thompson WG. Irritable bowel syndrome: pathogenesis and management. Lancet. 1993;341:1569-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | van Tilburg MA, Palsson OS, Levy RL, Feld AD, Turner MJ, Drossman DA, Whitehead WE. Complementary and alternative medicine use and cost in functional bowel disorders: a six month prospective study in a large HMO. BMC Complement Altern Med. 2008;8:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 90] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3413] [Cited by in RCA: 3381] [Article Influence: 177.9] [Reference Citation Analysis (1)] |
| 6. | Choi MG, Jung HK. Health related quality of life in functional gastrointestinal disorders in Asia. J Neurogastroenterol Motil. 2011;17:245-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Camilleri M. Peripheral mechanisms in irritable bowel syndrome. N Engl J Med. 2012;367:1626-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 229] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 8. | Jahangiri P, Jazi MS, Keshteli AH, Sadeghpour S, Amini E, Adibi P. Irritable Bowel Syndrome in Iran: SEPAHAN Systematic Review No. 1. Int J Prev Med. 2012;3:S1-S9. [PubMed] |
| 9. | Ford AC, Talley NJ. Irritable bowel syndrome. BMJ. 2012;345:e5836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Saito YA, Locke GR, Weaver AL, Zinsmeister AR, Talley NJ. Diet and functional gastrointestinal disorders: a population-based case-control study. Am J Gastroenterol. 2005;100:2743-2748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Gonlachanvit S. Are rice and spicy diet good for functional gastrointestinal disorders? J Neurogastroenterol Motil. 2010;16:131-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (2)] |
| 12. | Pilichiewicz AN, Horowitz M, Holtmann GJ, Talley NJ, Feinle-Bisset C. Relationship between symptoms and dietary patterns in patients with functional dyspepsia. Clin Gastroenterol Hepatol. 2009;7:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Williams EA, Nai X, Corfe BM. Dietary intakes in people with irritable bowel syndrome. BMC Gastroenterol. 2011;11:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Zhou HQ, Li DG, Song YY, Zong CH, Hu Y, Xu XX, Lu HM. [Risk factors of irritable bowel syndrome in adolescents in China]. Zhonghua Er Ke Zazhi. 2008;46:136-138. [PubMed] |
| 15. | Miwa H. Life style in persons with functional gastrointestinal disorders--large-scale internet survey of lifestyle in Japan. Neurogastroenterol Motil. 2012;24:464-71, e217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 16. | Heizer WD, Southern S, McGovern S. The role of diet in symptoms of irritable bowel syndrome in adults: a narrative review. J Am Diet Assoc. 2009;109:1204-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 17. | Gerkens A. [Irritable bowel syndrome: diet and complementary medicine therapies?]. Rev Med Brux. 2012;33:430-435. [PubMed] |
| 18. | Böhn L, Störsrud S, Simrén M. Nutrient intake in patients with irritable bowel syndrome compared with the general population. Neurogastroenterol Motil. 2013;25:23-30.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 19. | Ligaarden SC, Lydersen S, Farup PG. Diet in subjects with irritable bowel syndrome: a cross-sectional study in the general population. BMC Gastroenterol. 2012;12:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Niec AM, Frankum B, Talley NJ. Are adverse food reactions linked to irritable bowel syndrome? Am J Gastroenterol. 1998;93:2184-2190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 99] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 21. | Bortolotti M, Porta S. Effect of red pepper on symptoms of irritable bowel syndrome: preliminary study. Dig Dis Sci. 2011;56:3288-3295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Bortolotti M, Coccia G, Grossi G, Miglioli M. The treatment of functional dyspepsia with red pepper. Aliment Pharmacol Ther. 2002;16:1075-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 108] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 23. | Adibi P, Keshteli AH, Esmaillzadeh A, Afshar H, Roohafza H, Bagherian-Sararoudi R, Daghaghzadeh H, Soltanian N, Feinle-Bisset C, Boyce P. The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): Overview of methodology. J Res Med Sci. 2012;17:S292-S298. |
| 24. | Keith JN, Nicholls J, Reed A, Kafer K, Miller GD. The prevalence of self-reported lactose intolerance and the consumption of dairy foods among African American adults are less than expected. J Natl Med Assoc. 2011;103:36-45. [PubMed] |
| 25. | Hawrelak JA, Myers SP. Effects of two natural medicine formulations on irritable bowel syndrome symptoms: a pilot study. J Altern Complement Med. 2010;16:1065-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Bundy R, Walker AF, Middleton RW, Booth J. Turmeric extract may improve irritable bowel syndrome symptomology in otherwise healthy adults: a pilot study. J Altern Complement Med. 2004;10:1015-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Gonlachanvit S, Mahayosnond A, Kullavanijaya P. Effects of chili on postprandial gastrointestinal symptoms in diarrhoea predominant irritable bowel syndrome: evidence for capsaicin-sensitive visceral nociception hypersensitivity. Neurogastroenterol Motil. 2009;21:23-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 28. | Shah SK, Abraham P, Mistry FP. Effect of cold pressor test and a high-chilli diet on rectosigmoid motility in irritable bowel syndrome. Indian J Gastroenterol. 2000;19:161-164. [PubMed] |