Published online Aug 28, 2013. doi: 10.3748/wjg.v19.i32.5309
Revised: June 16, 2013
Accepted: July 18, 2013
Published online: August 28, 2013
Processing time: 139 Days and 2.3 Hours
AIM: To evaluate trans-anal reinforcing sutures in low anterior resection using the double-stapled anastomosis technique for primary rectal cancers performed at a single institution.
METHODS: The data of patients who received trans-anal reinforcing sutures were compared with those of patients who did not receive them after low anterior resection. Patients who underwent laparoscopic low anterior resection and the double-stapled anastomosis technique for primary rectal cancer between January 2008 and December 2011 were included in this study. Patients with no anastomosis, a hand-sewn anastomosis, high anterior resection, or preoperative chemoradiation were excluded. The primary outcomes measured were the incidence of postoperative anastomotic complications and placement of a diverting ileostomy.
RESULTS: Among 110 patients, the rate of placement of a diverting ileostomy was significantly lower in the suture group (SG) compared with the non-suture control group (CG) [SG, n = 6 (12.8%); CG, n = 19 (30.2%), P = 0.031]. No significant difference was observed in the rate of anastomotic leakage [SG, n = 3 (6.4%); CG, n = 5 (7.9%)].
CONCLUSION: Trans-anal reinforcing sutures may reduce the need for diverting ileostomy. A randomized prospective study with a larger population should be performed in the future to demonstrate the efficacy of trans-anal reinforcing sutures.
Core tip: We have performed trans-anal reinforcing sutures after the double-stapled anastomotic technique to intensify the anastomotic line and to reduce leakage. As a result, we found that the rate of placement of a diverting ileostomy was significantly reduced in cases of performing the trans-anal reinforcing sutures although there was no significant decrease of anastomotic leakage.
- Citation: Baek SJ, Kim J, Kwak J, Kim SH. Can trans-anal reinforcing sutures after double stapling in lower anterior resection reduce the need for a temporary diverting ostomy? World J Gastroenterol 2013; 19(32): 5309-5313
- URL: https://www.wjgnet.com/1007-9327/full/v19/i32/5309.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i32.5309
Anastomotic leakage is a major problem in patients who undergo rectal cancer surgery. This complication is associated with reoperation, prolonged hospital stay, and high morbidity and mortality. In addition, it can adversely influence functional and oncologic outcomes[1-4]. An anastomotic leakage rate of 2.5%-12% has been reported[5-8]. Leakage can be the result of a combination of technical, local, and systemic factors. Several risk factors, including old age, male sex, smoking, diabetes, obesity, preoperative chemotherapy, and a more distal tumor location, are associated with anastomotic leakage after rectal cancer surgery[9-12]. In particular, the technical aspects of anastomosis are also very important. Leakage rates have also been used as an indicator of surgical quality[13,14].
Since being introduced by Griffen et al[15] and Knight et al[16], the double-stapled anastomotic technique has been widely used in colorectal surgery because it allows the anastomosis to be made very low in the pelvis and preserves the anal sphincter[17]. However, this technique creates stapled corners known as “dog ears”, which are made by crossing at least two staple lines and become potentially vulnerable areas[18]. The staple line may also be weakened through friction created by hard stools, increasing the risk of anastomotic failure[19].
To address these problems, various methods, such as the single-stapled, double-pursestring method, and bioabsorbable staple-line reinforcement, have been suggested[18,20]. The trans-anal reinforcing suture is another such improvement that has been proposed. We hypothesized that placing the sutures along the staple line, including the corners, can reinforce the anastomosis and reduce anastomotic leakage. Therefore, we are currently using trans-anal reinforcing sutures for low anterior resection. The aim of this study was to determine the effect of trans-anal reinforcing sutures in terms of anastomotic complications and diverting stoma placement.
Between January 2008 and December 2011, patients who underwent rectal resection at Korea University Anam Hospital for primary rectal cancer were enrolled in this study. The patients who underwent laparoscopic low anterior resection and double stapled anastomosis and had an anastomotic line located within 5-6 cm of the anal verge where trans-anal suturing is possible were included. The exclusion criteria were as follows: intersphincteric resection and coloanal anastomosis, total abdominal colectomy and ileo-rectal anastomosis, abdominoperineal resection, Hartmann’s operation, transanal resection and high anterior resection, and a history of receiving chemoradiotherapy preoperatively.
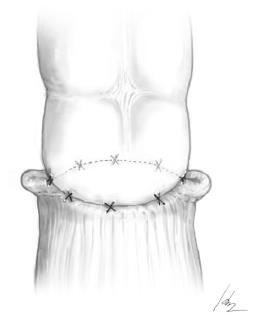
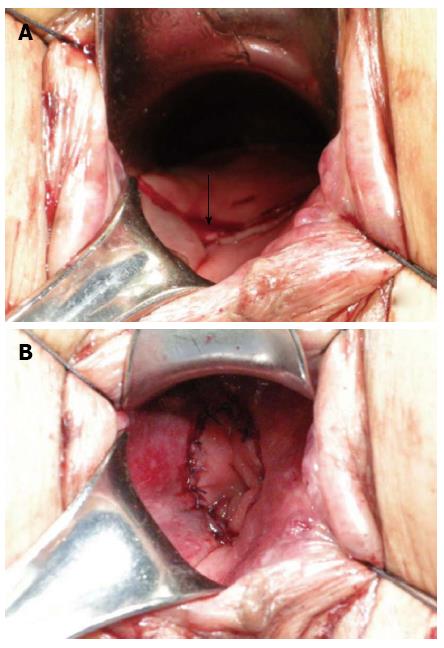
We have been utilizing trans-anal reinforcing sutures since January 2010. A schematic view of the procedure and trans-anal view are shown in Figures 1 and 2. After rectal division using an endo-linear cutter (Echelon, Ethicon), end-to-end anastomosis is performed using a circular stapler (CDH 29 mm, Ethicon), and trans-anal reinforcing sutures are used via the anal canal. Six to eight interrupted sutures are placed along the staple line circumferentially, and two corners made by crossing circular and linear staple lines are always included. An air leakage test is performed for all patients after anastomosis and trans-anal reinforcing suture, if done. Temporary diverting ileostomy is considered in cases with several operative or preoperative risk factors such as: a positive air leakage test, insufficient vascular supply at colonic section, several stapling for rectal division, incomplete circular stapling donut, underlying cardiovascular disease, rectal wall muscle injury, and stool spillage. We do not perform ostomy in all male patients.
Clinical anastomotic leakage is defined in the event of clinical symptoms of sepsis, including abdominal pain, tenderness, fever, or leukocytosis. All patients diagnosed with anastomotic leakage in this study were identified within 30 d. Clinical leakage signs were discharge of gas, pus, or feces through the abdominal drain, rectum, or vagina, fecal peritonitis, abscess at the level of the anastomosis, and fluid/air bubbles surrounding the anastomosis on computed tomography (CT). Asymptomatic anastomotic leakages were not considered because routine contrast enemas were not performed after surgery. Patients who developed leakage were treated conservatively with antibiotics, received CT or ultrasonography guided drainage, or were treated with reoperation under general anesthesia.
All data were prospectively collected in a database and analyzed under the approval of the Institutional Review Board. Patient demographics, tumor characteristics, operative records, and postoperative courses were compared between patients who had trans-anal reinforcing sutures and those who did not. Statistical analysis was performed using SPSS version 12.0 (Chicago, IL). Student’s t-test was used to compare continuous variables. χ2 test was used to compare discrete variables. P < 0.05 was considered statistically significant.
In total, 110 patients underwent laparoscopic low anterior resection with double-stapled anastomosis for primary rectal cancer [47 in the suture group (SG), and 63 in the non-suture control group (CG)]. Relevant patient characteristics and surgical histories are shown in Table 1. No significant difference was observed in sex, age, or body mass index (BMI) between groups. There was also no difference in mean tumor level (9.7 cm vs 9.7 cm from the anal verge, P = 0.974), mean length of operation (198.3 min vs 212.1 min, P = 0.305) or estimated blood loss (174.5 mL vs 188.4 mL, P = 0.823) between groups. The number of temporary diverting ileostomies performed was significantly higher in the control group [SG, n = 6 (12.8%); CG, n = 19 (30.2%), P = 0.031].
| Suture group (n = 47) | Control group (n = 63) | P value | |
| Sex | 0.196 | ||
| Male | 29 (61.7) | 31 (49.2) | |
| Female | 18 (38.3) | 32 (50.8) | |
| Age (yr) (range) | 64.1 ± 9.8 (39-80) | 61.4 ± 11.0 (42-82) | 0.199 |
| BMI (kg/m2) (range) | 24.1 ± 3.1 (18.5-33.7) | 23.5 ± 2.7 (17.9-28.8) | 0.272 |
| Tumor level (cm above AV) (ranges) | 9.7 ± 3.9 (2-15) | 9.7 ± 3.6 (4-15) | 0.974 |
| Diverting ileostomy | 6 (12.8) | 19 (30.2) | 0.031 |
| Length of the operation (min) (ranges) | 198.3 ± 75.7 (90-477) | 212.1 ± 65.0 (75-335) | 0.305 |
| Estimated blood loss (mL) (ranges) | 174.5 ± 348.0 (0-2000) | 188.4 ± 301.5 (0-1500) | 0.823 |
The postoperative courses are outlined in Table 2. No significant differences were observed in the time to postoperative flatus (1.5 d vs 1.5 d, P = 0.809), stool passage (4.1 d vs 3.8 d, P = 0.675), feeding (2.8 d vs 2.3 d, P = 0.103), or postoperative hospital stay (11.0 d vs 9.8 d, P = 0.321). The incidence of anastomotic leakage, which was not significant between groups (P = 0.759), was 6.4% in the SG (n = 3) and 7.9% in the CG (n = 5). Two patients in each group required reoperation for anastomotic leakage, while others were treated conservatively. There were no differences in other complications between the two groups.
| Suture group (n = 47) | Control group (n = 63) | P value | |
| Flatus (d) (range) | 1.5 ± 0.9 (0-4) | 1.5 ± 1.2 (0-7) | 0.809 |
| Stool (d) (range) | 4.1 ± 2.5 (0-10) | 3.8 ± 1.7 (1-7) | 0.675 |
| Feed (d) (range) | 2.8 ± 1.1 (1-6) | 2.3 ± 1.8 (1-13) | 0.103 |
| Postoperative HS (d), (range) | 11.0 ± 5.6 (4-36) | 9.8 ± 6.7 (5-44) | 0.321 |
| Complications | 4 (8.5) | 7 (11.1) | 0.656 |
| Anastomotic leakage | 3 (6.4) | 5 (7.9) | 0.759 |
| Conservative management | 1 | 3 | |
| Reoperation | 2 | 2 | |
| Intra-abdominal bleeding | 0 | 1 (1.6) | 0.390 |
| Postoperative ARF | 1 (2.1) | 1 (1.6) | 0.390 |
The occurrence of anastomotic leakage is a major concern in rectal cancer surgery. The consensus is that the main causes of anastomotic leakage are ischemia and tension. Among the risk factors for anastomotic leakage, the technical aspects of surgery are very important as they are the only known factors that may be corrected. In the double-stapled anastomotic technique, at least two staple lines cross each other, creating vulnerable corners. Some reports have concluded that the anastomotic technique used is not an important factor in anastomotic leakage, however some controversy still exists[21].
Various attempts to modify the technical aspects in order to reduce the problem of the double-stapled anastomotic technique have been attempted. Marecik et al[18] used the single-stapled, double pursestring technique for colorectal anastomosis in 160 patients who underwent anterior resection of the upper- or mid-rectum, which resulted in an extremely low rate of anastomotic leakage (0.6%). Mukai et al[22] reported good results in two cases in which trans-anal reinforcing sutures after double-stapling for lower rectal cancer were used. Gadiot et al[19] compared 76 patients who received anti-traction sutures and 77 who did not, and found that the need for placement of a diverting ostomy was significantly lower in patients who received sutures.
In our study, there was no significant difference in anastomotic leakage between those who received trans-anal reinforcing sutures and those who did not. However, the need for temporary diverting ileostomy was significantly lower in the suture group, which is the most important outcome in this study. Although some controversy exists as to whether or not proximal diversion affects leak rates[12,23,24], diverting ileostomy may play a role in moderating symptoms or signs of anastomotic leakage to subclinical levels. Consequently, leakage rates may be underestimated in patients who undergo diverting ileostomy. Thus, the actual rate of anastomotic leakage in the control group, which had more ileostomies, was possibly higher than presented.
Meanwhile, trans-anal reinforcing sutures could reduce the need for placement of a diverting ileostomy. It may be due to the decrease in positive air leakage although we cannot present absolute numbers because we believe that the other risk factors for anastomotic leakage were similar between groups. Less air leakage means that trans-anal reinforcing sutures can reduce potential anastomotic leakage by serving as a mechanical safety mechanism. We believe this procedure can be a useful method for the prevention of mechanical failure by reducing anastomotic tension. Therefore, the need for less ileostomy in the suture group is clinically meaningful.
In addition, this procedure can provide emotional stability to surgeons. The placement of stoma usually depends on the surgeon’s subjectivity. Apart from the cases where stoma definitely need to be made, many diverting stoma are made due only to the surgeon’s insecurity. Although the trans-anal reinforcing sutures may not prevent definite major anastomotic leakage or may not reduce diverting stoma made due to the evident risk, it is believed that this procedure has a positive effect in that it decreases the number of unnecessary stoma by indirectly enhancing surgeons’ emotional stability.
While diverting ileostomy is an important procedure for patients at risk for anastomotic leakage, it also carries the potential for many complications and is inconvenient for patients[25-27]. Complications related to ostomy include herniation, retraction, prolapse, stenosis, stoma ischemia, mucocutaneous suture line, and skin problems such as irritant contact dermatitis, inflammatory damage, or allergic reaction. Moreover, systemic complications such as dehydration may occur. In addition, surgery is required at least once more, which can impact patient quality of life and may result in poor cosmesis[28]. Therefore, unnecessary placement of an ileostomy should be avoided. If a simple procedure such as trans-anal reinforcing sutures can reduce the incidence of ileostomies, its use should be considered.
In our results, there was no significant difference between the suture group and the non-suture group in terms of operation time as it takes about 5-0 min to perform the trans-anal reinforcing sutures. Considering that the main disadvantages of using the single-stapled technique include the extra time needed and the potential for pelvic contamination[18], the trans-anal reinforcing suture method is easy and efficacious without additional time or complexity. As this procedure is not different from the one used at the time of trans-anal excision or hemorrhoid surgery, thus it is very familiar to surgeons and a specific learning curve for it may not be necessary even in male patients with narrow pelvises. The only precaution that may need to be taken concerns a risk of vaginal fistula in cases of deep sutures of the female anterior part. This risk should be kept in mind.
Another advantage of trans-anal reinforcing sutures is that anastomotic bleeding can be prevented. Anastomotic bleeding may occur at the staple line and sometimes requires hemostasis with endoscopy or surgery. Thus, routine trans-anal inspection and suturing could aid in the detection of anastomotic bleeding and thereby prevent the increase in rectal pressure due to blood collection.
Our study has several limitations. First, there may have been selection bias in the decision to place a diverting ileostomy since the decision for ileostomy is solely the surgeon’s. Our results showed that the incidence of temporary diverting ileostomy was significantly lower in the suture group. Even so, one advantage of this procedure is that it may reduce the number of unnecessary diverting ileostomies made due to the surgeon’s excessive anxiety. Second, this study was not randomized, and there was a difference between the two groups when the surgeries were performed. The time difference may be the result of bias due to the surgeon’s experience and may have affected the results of the procedures or the postoperative courses. However, the effects of this bias may not be significant since the surgeon performing the procedures in this study was very experienced and had performed a large volume of cases prior to the study period. Third, the sample size was relatively small. Thus, a randomized prospective study should be conducted in a larger population in the future.
In conclusion, our study demonstrates that trans-anal reinforcing sutures can be performed easily and safely in patients undergoing low anterior resection using the double-stapled anastomosis technique for primary rectal cancer. This procedure may reduce the number of diverting ileostomies performed. A prospective randomized trial is necessary to evaluate the effect of trans-anal reinforcing sutures on anastomotic leakage as well as the necessity of the placement of stomas.
Anastomotic leakage is a major problem in patients who undergo rectal cancer surgery. This complication is associated with reoperation, prolonged hospital stay, and high morbidity and mortality. In addition, it can adversely influence functional and oncologic outcomes. Leakage can be the result of a combination of technical, local, and systemic factors. Several risk factors, including old age, male sex, smoking, diabetes, obesity, preoperative chemotherapy, and a more distal tumor location, are associated with anastomotic leakage after rectal cancer surgery.
To address these problems, various methods, such as the single-stapled, double-pursestring method, and bioabsorbable staple-line reinforcement, have been suggested. The trans-anal reinforcing suture is another such improvement that has been proposed.
This study was conducted to determine the effect of trans-anal reinforcing sutures in terms of anastomotic complications and diverting stoma placement.
This study demonstrates that trans-anal reinforcing sutures can be performed easily and safely in patients undergoing low anterior resection using the double-stapled anastomosis technique for primary rectal cancer.
This paper addresses an important issue which is of interest to most surgeons. Anastomotic breakdown carries a major morbidity and mortality. Any procedure that attempts to reduce this is welcome.
P- Reviewers Abou-Zeid AA, Amin I, Michot F S- Editor Zhai HH L- Editor O’Neill M E- Editor Zhang DN
| 1. | Bell SW, Walker KG, Rickard MJ, Sinclair G, Dent OF, Chapuis PH, Bokey EL. Anastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence. Br J Surg. 2003;90:1261-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 246] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Jung SH, Yu CS, Choi PW, Kim DD, Park IJ, Kim HC, Kim JC. Risk factors and oncologic impact of anastomotic leakage after rectal cancer surgery. Dis Colon Rectum. 2008;51:902-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 192] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 3. | Bruce J, Krukowski ZH, Al-Khairy G, Russell EM, Park KG. Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg. 2001;88:1157-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 510] [Article Influence: 21.3] [Reference Citation Analysis (1)] |
| 4. | Nesbakken A, Nygaard K, Lunde OC. Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer. Br J Surg. 2001;88:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 257] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 5. | Schlachta CM, Mamazza J, Gregoire R, Burpee SE, Poulin EC. Could laparoscopic colon and rectal surgery become the standard of care? A review and experience with 750 procedures. Can J Surg. 2003;46:432-440. [PubMed] |
| 6. | Matthiessen P, Hallböök O, Andersson M, Rutegård J, Sjödahl R. Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis. 2004;6:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 431] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 7. | Goriainov V, Miles AJ. Anastomotic leak rate and outcome for laparoscopic intra-corporeal stapled anastomosis. J Minim Access Surg. 2008;4:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | McArdle CS, McMillan DC, Hole DJ. Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg. 2005;92:1150-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 352] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 9. | Law WI, Chu KW, Ho JW, Chan CW. Risk factors for anastomotic leakage after low anterior resection with total mesorectal excision. Am J Surg. 2000;179:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 268] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 10. | Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T, Rutten HJ, van de Velde CJ. Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg. 2005;92:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 507] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 11. | Alberts JC, Parvaiz A, Moran BJ. Predicting risk and diminishing the consequences of anastomotic dehiscence following rectal resection. Colorectal Dis. 2003;5:478-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 128] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM, Tang R. Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg. 2005;241:9-13. [PubMed] |
| 13. | Isbister WH. Anastomotic leak in colorectal surgery: a single surgeon’s experience. ANZ J Surg. 2001;71:516-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Collopy BT. Colorectal anastomotic leak rates are measures of technical skill in surgery. ANZ J Surg. 2001;71:508-510. [PubMed] |
| 15. | Griffen FD, Knight CD, Whitaker JM, Knight CD. The double stapling technique for low anterior resection. Results, modifications, and observations. Ann Surg. 1990;211:745-51; discussion 751-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 125] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Knight CD, Griffen FD. An improved technique for low anterior resection of the rectum using the EEA stapler. Surgery. 1980;88:710-714. [PubMed] |
| 17. | Baran JJ, Goldstein SD, Resnik AM. The double-staple technique in colorectal anastomoses: a critical review. Am Surg. 1992;58:270-272. [PubMed] |
| 18. | Marecik SJ, Chaudhry V, Pearl R, Park JJ, Prasad LM. Single-stapled double-pursestring anastomosis after anterior resection of the rectum. Am J Surg. 2007;193:395-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Gadiot RP, Dunker MS, Mearadji A, Mannaerts GH. Reduction of anastomotic failure in laparoscopic colorectal surgery using antitraction sutures. Surg Endosc. 2011;25:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Portillo G, Franklin ME. Clinical results using bioabsorbable staple-line reinforcement for circular stapler in colorectal surgery: a multicenter study. J Laparoendosc Adv Surg Tech A. 2010;20:323-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Moore JW, Chapuis PH, Bokey EL. Morbidity and mortality after single- and double-stapled colorectal anastomoses in patients with carcinoma of the rectum. Aust N Z J Surg. 1996;66:820-823. [PubMed] |
| 22. | Mukai M, Fukasawa M, Kishima K, Iizuka S, Fukumitsu H, Yazawa N, Tajima T, Nakamura M, Makuuchi H. Trans-anal reinforcing sutures after double stapling for lower rectal cancer: report of two cases. Oncol Rep. 2009;21:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Walker KG, Bell SW, Rickard MJ, Mehanna D, Dent OF, Chapuis PH, Bokey EL. Anastomotic leakage is predictive of diminished survival after potentially curative resection for colorectal cancer. Ann Surg. 2004;240:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 343] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 24. | Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN. Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Colorectal Dis. 2005;7:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 254] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 25. | Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D. Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum. 2006;49:1011-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 98] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 26. | Mala T, Nesbakken A. Morbidity related to the use of a protective stoma in anterior resection for rectal cancer. Colorectal Dis. 2008;10:785-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Giannakopoulos GF, Veenhof AA, van der Peet DL, Sietses C, Meijerink WJ, Cuesta MA. Morbidity and complications of protective loop ileostomy. Colorectal Dis. 2009;11:609-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 28. | Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M. Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum. 2008;51:218-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |