Published online Aug 21, 2013. doi: 10.3748/wjg.v19.i31.5118
Revised: February 20, 2013
Accepted: April 9, 2013
Published online: August 21, 2013
Processing time: 214 Days and 9.1 Hours
AIM: To investigate the effect of rikkunshito on laryngopharyngeal reflux (LPR) symptoms and gastric emptying in patients with proton-pump inhibitor (PPI)-refractory LPR.
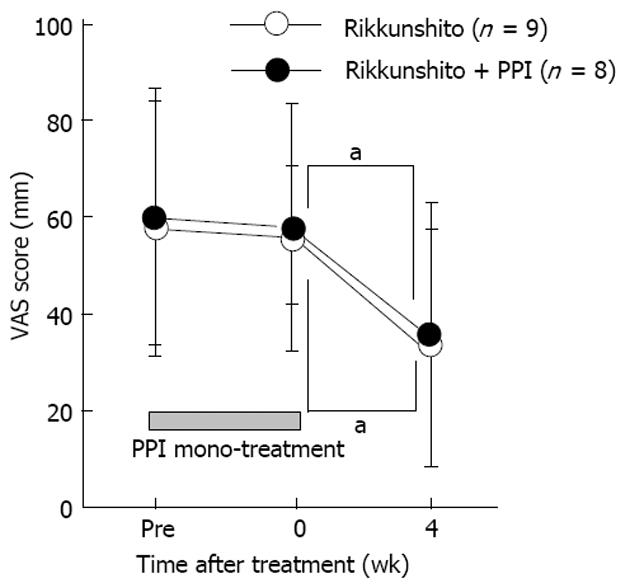
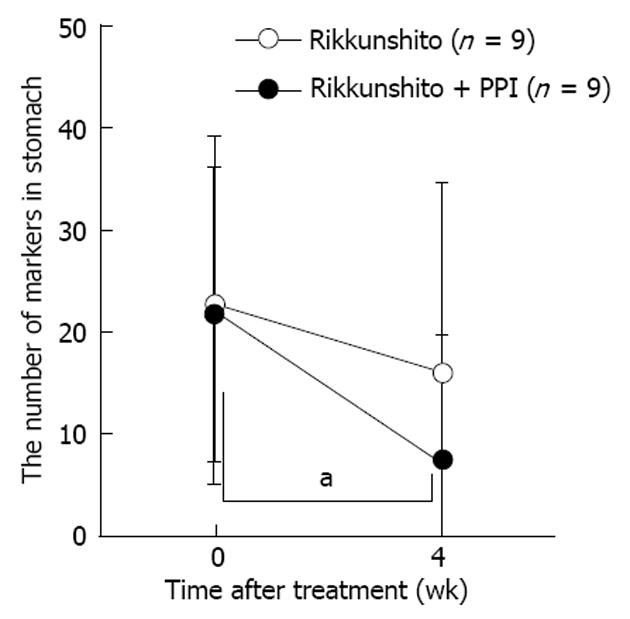
METHODS: In total, 22 patients with LPR were enrolled. Following a 2-wk treatment with PPI monotherapy, PPI-refractory LPR patients were randomly divided into two treatment groups (rikkunshito alone or rikkunshito plus the PPI, lansoprazole). LPR symptoms were assessed using a visual analog scale (VAS) score, gastrointestinal symptoms were assessed using the gastrointestinal symptom rating scale (GSRS), and gastric emptying was assessed using the radio-opaque marker method prior to and 4 wk following treatments.
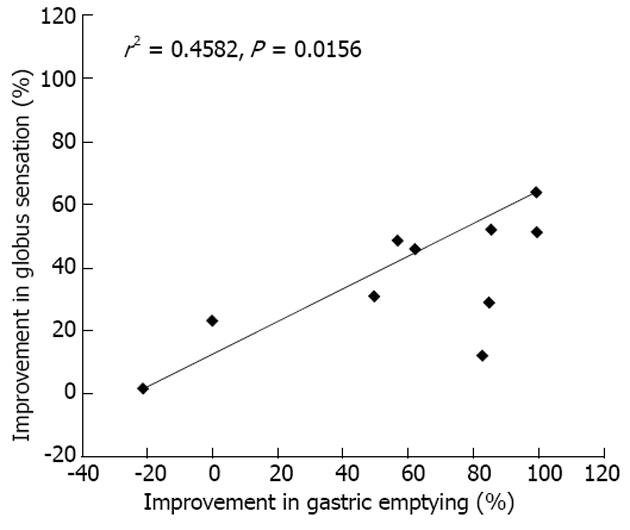
RESULTS: The 4-wk treatment with rikkunshito alone and with rikkunshito plus the PPI significantly decreased the globus sensation VAS scores. The VAS score for sore throat was significantly decreased following treatment with rikkunshito plus PPI but not by rikkunshito alone. Neither treatment significantly changed the GSRS scores. Rikkunshito improved delayed gastric emptying. We found a significant positive correlation between improvements in globus sensation and in gastric emptying (r2 = 0.4582, P < 0.05).
CONCLUSION: Rikkunshito improved globus sensation in patients with PPI-refractory LPR, in part, because of stimulation of gastric emptying. Thus, rikkunshito is an effective treatment for PPI-refractory LPR.
Core tip: Regarding the treatment of laryngopharyngeal reflux (LPR) symptoms such as globus sensation and a scratchy feeling, proton pump inhibitors (PPIs) are considered the mainstay. We investigated the effects of rikkunshito on globus sensation and gastric emptying in patients with PPI-refractory LPR.
- Citation: Tokashiki R, Okamoto I, Funato N, Suzuki M. Rikkunshito improves globus sensation in patients with proton-pump inhibitor-refractory laryngopharyngeal reflux. World J Gastroenterol 2013; 19(31): 5118-5124
- URL: https://www.wjgnet.com/1007-9327/full/v19/i31/5118.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i31.5118
Symptoms or complaints of globus sensation (“globus”), a “lump in the throat” feeling located between the upper edge of the sternum and the cricoid region, are common. Recently, gastroesophageal reflux disease (GERD) has been identified as a major cause of globus[1-3]. Stomach acid reflux produces a number of extraesophageal symptoms in the laryngopharynx, commonly referred to as laryngopharyngeal reflux (LPR)[1,2], which include a hoarse voice, cough, a scratchy feeling in the throat, and globus[1-3]. However, the etiology of globus remains unclear. Recent studies have suggested the condition may be caused by hypertonicity in the upper esophageal sphincter (UES)[4,5]. We have demonstrated that elevated UES pressure resulting from gastroesophageal reflux without direct exposure of the hypopharynx to acid can cause the globus sensation[6].
Proton-pump inhibitors (PPIs) are considered the mainstay treatment for LPR[7]. However, LPR requires more aggressive and prolonged therapy than GERD, and PPIs do not improve extraesophageal symptoms in the laryngopharynx in all cases[7,8]. Furthermore, increasing evidence suggests that duodeno-gastroesophageal reflux may be related to several laryngeal disorders[9]. Thus, stimulation of gastric emptying or esophageal clearance in addition to inhibition of gastric acid secretion may be an effective treatment for LPR. Ezzat et al[10] reported that adding prokinetics, such as cisapride and itopride, to PPIs to treat LPR reduced the recurrence of symptoms. However, few studies have investigated the efficacy of prokinetics in the treatment of LPR.
Rikkunshito, a traditional Japanese medicine, is widely used to treat upper gastrointestinal symptoms such as gastroesophageal reflux[11,12] and dyspepsia[13,14]. Rikkunshito has been shown to accelerate gastric emptying in functional dyspeptic patients[13,14] and rats[15]. Furthermore, rikkunshito improved upper gastrointestinal symptoms in PPI-refractory GERD patients[12]. Thus, we investigated the effects of rikkunshito on globus sensation and gastric emptying in patients with PPI-refractory LPR.
In total, 22 patients with PPI-refractory LPR were enrolled at Tokyo Medical University Hospital, from March, 2007 to December, 2008. PPI-refractory LPR was defined as the presence of LPR symptoms (globus sensation, sore throat, excessive throat clearing) despite therapy using a standard dose of PPI for 2 or more weeks. Enrolled patients met the following inclusion criteria: (1) 20-76 years of age; (2) received standard-dose therapy with a PPI for at least 2 wk prior to commencement of the study; (3) a score of three or higher than the average gastrointestinal symptom rating scale (GSRS) score for acid reflux, abdominal pain, or indigestion; (4) had LPR symptoms (globus sensation, sore throat, or excessive throat clearing); and (5) provided written informed consent for study participation. Exclusion criteria were: (1) use of an antipsychotic drug, skeletal muscle relaxant, anti-ulcer drug (with the exception of a PPI), digestive drug, or antacid within 2 wk of the start of the present study; (2) patients who had globus sensation, laryngopharyngeal pain, or chronic cough due to an organic disease; (3) cervical spine disease; (4) sinusitis; (5) bronchial asthma; (6) patients with serious complications; (7) a history of drug hypersensitivity; (8) females who were pregnant or wished to become pregnant during the study or follow-up period, and lactating females; and (9) patients who were considered unsuitable by the chief investigator.
This prospective, randomized, comparative parallel group study examined the efficacy and safety of a therapeutic strategy using rikkunshito in patients with PPI-refractory LPR. The study was conducted according to ethical guidelines for clinical studies and with consideration of patients’ human rights and privacy. The protocol was approved by the Institutional Review Board of Tokyo Medical University.
All patients were treated with a standard-dose PPI for at least 2 wk prior to obtaining written informed consent. After obtaining written informed consent, LPR symptoms and gastrointestinal symptoms were evaluated using a visual analog scale (VAS) score and the GSRS scores. Following treatment with the PPI, lansoprazole (30 mg/d, qd), for at least 2 wk, patients with PPI-refractory LPR who met the inclusion and none of the exclusion criteria were enrolled in the study. Enrolled patients were randomly divided into two groups using the envelope method: rikkunshito (7.5 g/d, tid) alone and rikkunshito (7.5 g/d, tid) plus a standard dose of lansoprazole (30 mg/d). We used a powdered extract of rikkunshito (Tsumura & Co., Tokyo, Japan) obtained by spray drying a hot water extract mixture of the following eight crude herbs: Atractylodis lanceae Rhizoma (4.0 g), Ginseng radix (4.0 g), Pinelliae tuber (4.0 g), Hoelen (4.0 g), Zizyphi fructus (2.0 g), Aurantii nobilis pericarpium (2.0 g), Glycyrrhizae radix (1.0 g), and Zingiberis rhizoma (0.5 g). LPR symptoms, gastrointestinal symptoms, and gastric emptying were evaluated before and after a 4-wk treatment regimen using rikkunshito or rikkunshito plus PPI.
LPR symptoms of globus sensation, sore throat, and excessive throat clearing were assessed using a VAS scale. Gastrointestinal symptoms were assessed using the GSRS, a 15-item questionnaire used to assess general gastrointestinal symptoms[16]. Each GSRS item is rated on a seven-point Likert scale, from no discomfort (1) to very severe discomfort (7). According to a factor analysis, the 15 GSRS items are divided into five domains: abdominal pain (abdominal pain, hunger pain, and nausea), reflux syndrome (heartburn and acid regurgitation), diarrhea syndrome (diarrhea, loose stools, urgent need for defecation), indigestion syndrome (borborygmus, abdominal distension, eructation, increased flatus), and constipation syndrome (constipation, hard stools, feeling of incomplete evacuation).
Radio-opaque markers were used to evaluate gastric emptying according to the method proposed by Cremonini et al[17]. Briefly, 18 subjects swallowed a capsule containing 40 radio-opaque markers (Sitzmarks, Konsyl Pharmaceuticals, Fort Worth, TX, United States) before and after 4 wk treatment with rikkunshito or rikkunshito plus PPI. A plain abdominal radiograph was obtained 3 h after intake of the capsule, and the number of markers in the stomach was counted.
Safety and tolerability were assessed by recording all adverse events, and changes in hematological and clinical laboratory variables were measured at the screening visit. An adverse event was defined as any unfavorable or unintended sign, whether or not it was considered to be causally related to the drugs used in this study.
Treatment compliance was defined as the percentage of the test drug used. A treatment compliance of at least 66.6% was considered acceptable.
Within-group treatment responses in were evaluated according to pre- and post-treatment VAS and GSRS scores using a paired t test or the Wilcoxon signed-rank test. Mean the pre- and post-treatment scores were compared between groups using the Wilcoxon rank-sum test. Between-group age and demographic factors were compared using the Wilcoxon rank-sum test, and the distributions of sex and smoking status were compared using Fisher’s exact test. We calculated the correlation between change in globus sensation and change in gastric emptying values using the non-parametric Spearman’s r correlation. P values < 0.05 were considered to indicate statistical significance. All data are expressed as mean ± SD.
We found no marked differences in age, sex, or smoking status between the groups (Table 1). No difference was found between pre- and post-PPI monotherapy for globus sensation (VAS score, 58.7 ± 25.2 and 56.7 ± 20.1, respectively) or gastrointestinal symptoms (overall GSRS score, 2.2 ± 0.9 and 2.0 ± 0.7, respectively) in the enrolled patients.
| Rikkunshito | Rikkunshito + PPI | |
| Number of patients | 11 | 11 |
| Mean age (range) | 55.9 (39-76) | 56.6 (25-76) |
| Sex (male/female) | 4/7 | 4/7 |
| Smoking (yes/no) | 5/6 | 3/8 |
The 4-wk treatment regimen significantly decreased the globus sensation VAS scores in both treatment groups (Figure 1). Furthermore, the post-treatment VAS scores were not significantly different between treatment groups.
The effects of rikkunshito alone or rikkunshito plus PPI treatments on sore throat and excessive throat clearing in patients with PPI-refractory LPR are shown in Table 2. The VAS scores for sore throat and excessive throat clearing did not decrease following the 2-wk PPI monotherapy. The VAS score for sore throat decreased after treatment with rikkunshito plus PPI but not after rikkunshito alone. The VAS score for excessive throat clearing did not change in either treatment group.
| Week | Visual analog scale score (mean ± SD) | |||
| A: Rikkunshito | B: Rikkunshito + PPI | P (A vs B) | ||
| Sore throat | (n = 4) | (n = 5) | ||
| -2 | 35.4 ± 21.6 | 44.3 ± 30.5 | 0.730 | |
| 0 | 24.0 ± 28.1 | 45.2 ± 28.4 | 0.234 | |
| 4 | 24.8 ± 32.8 | 31.8 ± 30.2a | 0.538 | |
| Excessive throat clearing | (n = 4) | (n = 8) | ||
| -2 | 48.0 ± 12.8 | 40.8 ± 32.5 | 1.000 | |
| 0 | 37.2 ± 21.5 | 45.7 ± 25.0 | 0.514 | |
| 4 | 39.8 ± 34.9 | 25.7 ± 24.2 | 0.569 | |
Neither the rikkunshito alone nor rikkunshito plus PPI treatment group showed a significant change in the overall GSRS or five subscale scores following the 4-wk treatment period (Table 3).
| Week | Rikkunshito (mean ± SD) | Test1P value | Rikkunshito + PPI (mean ± SD) | Test1P value | Test2P value | |
| Overall scores | -2 | 2.25 ± 1.06 | 0.232 | 2.19 ± 0.73 | 0.375 | 1.000 |
| 0 | 2.12 ± 0.85 | - | 1.96 ± 0.50 | - | 0.778 | |
| 4 | 1.83 ± 0.84 | 0.148 | 1.73 ± 0.37 | 0.195 | 0.736 | |
| Subscale scores | ||||||
| Reflux syndrome | -2 | 2.25 ± 1.06 | 0.055 | 2.79 ± 0.91 | 0.170 | 0.369 |
| 0 | 2.23 ± 1.60 | - | 2.45 ± 1.42 | - | 0.540 | |
| 4 | 1.94 ± 1.16 | 1.000 | 1.94 ± 0.86 | 0.106 | 0.801 | |
| Abdominal pain | -2 | 2.27 ± 1.29 | 0.168 | 2.33 ± 1.12 | 0.058 | 0.658 |
| 0 | 1.87 ± 0.86 | - | 1.77 ± 0.85 | - | 0.914 | |
| 4 | 1.59 ± 0.78 | 0.250 | 1.50 ± 0.40 | 0.223 | 0.805 | |
| Indigestion syndrome | -2 | 2.40 ± 1.04 | 0.615 | 2.54 ± 1.29 | 0.551 | 0.844 |
| 0 | 2.30 ± 1.03 | - | 2.20 ± 0.86 | - | 1.000 | |
| 4 | 2.17 ± 1.22 | 0.201 | 1.94 ± 0.75 | 0.139 | 0.961 | |
| Diarrhea syndrome | -2 | 1.77 ± 1.05 | 0.750 | 1.71 ± 0.71 | 1.000 | 0.878 |
| 0 | 1.61 ± 0.68 | - | 1.77 ± 0.75 | - | 0.661 | |
| 4 | 1.41 ± 0.49 | 0.098 | 1.71 ± 0.68 | 0.866 | 0.345 | |
| Constipation syndrome | -2 | 1.77 ± 1.05 | 0.341 | 1.71 ± 0.71 | 0.784 | 0.138 |
| 0 | 1.61 ± 0.68 | - | 1.77 ± 0.75 | - | 0.254 | |
| 4 | 1.41 ± 0.49 | 0.134 | 1.71 ± 0.68 | 1.000 | 0.883 |
Changes in gastric emptying following rikkunshito or rikkunshito plus PPI treatment are shown in Figure 2. The number of markers in the stomach tended to decrease after treatment with rikkunshito alone, but the difference was not statistically significant. However, the number of markers in the stomach was significantly decreased following treatment with rikkunshito plus PPI. We found no between-group difference in the number of markers in the stomach following the 4-wk treatment period.
The correlation between improvement in globus sensation and improvement in gastric emptying is shown in Figure 3. A marked improvement in globus sensation was observed in patients with PPI-refractory LPR as gastric emptying improved. The correlation analysis revealed a significant positive correlation between the improvement in globus sensation and the improvement in gastric emptying (r2 = 0.4582, P < 0.05).
No adverse event/reaction requiring treatment occurred in any patient during the study period.
As no diagnostic gold standard is available for LPR, few studies have investigated this condition. However, previous reports indicate that 74.4% of GERD patients experience extraesophageal or atypical manifestations with prevalences of globus sensation and laryngitis/pharyngitis in GERD patients of 38.7% and 19.9%, respectively[8]. LPR requires more aggressive and prolonged therapy than GERD, and several cases in which PPIs did not improve extraesophageal symptoms in the laryngopharynx have been reported[7,8]. We examined PPI-refractory patients whose LPR symptoms of globus sensation, sore throat, or excessive throat clearing did not improve after at least 2 wk of PPI treatment. Rikkunshito has been shown to improve upper gastrointestinal symptoms in PPI-refractory GERD patients[12]; thus, we investigated the efficacy of rikkunshito in improving extraesophageal symptoms in patients with PPI-refractory LPR. Our findings indicate that a 4-wk treatment regimen of rikkunshito alone or rikkunshito plus PPI improved globus sensation in patients with PPI-refractory LPR. Two theories of LPR pathogenesis have been proposed. According to the direct impairment theory, LPR occurs when stomach acid acts directly on the hypopharynx, whereas the reflex theory holds that acid reflux in the lower esophagus causes coughing or other symptoms through a vagal reflex[1-3]. Moreover, we demonstrated previously that globus sensation can be caused by elevated upper esophageal sphincter pressure resulting from gastroesophageal reflux without direct exposure of the hypopharynx to acid[6]. Thus, acid secretion control alone is not sufficient for the treatment of LPR, which is caused by several factors. Unlike the PPIs, rikkunshito does not have an anti-secretory effect[18], and, thus, may improve the globus sensation via a different mechanism. Kawahara et al[11] reported that rikkunshito reduced esophageal acid exposure through improved esophageal acid clearance in GERD patients. The hesperidine and atractylodin, components of rikkunshito, have been shown to improve delayed gastric emptying in L-NNA-administered rats[15,19], and rikkunshito improved upper GI symptoms via stimulation of gastric emptying in functional dyspeptic patients[13,14] and in patients who had undergone pylorus-preserving gastrectomy[20]. A recent study showed that rikkunshito stimulated secretion of a ghrelin, which has stimulatory effects on appetite and gastrointestinal motor activity[21,22]. Furthermore, rikkunshito and atractylodin enhance reactivity of its receptor[23]. Nahata et al[24] found an association between impaired ghrelin signaling and gastrointestinal motility dysfunction and demonstrated that rikkunshito restored gastrointestinal motility by improving the ghrelin response in rat GERD models. If rikkunshito reduces gastric contents, it seems reasonable that a subsequent reduction in the reflux volume may reduce acid exposure in the esophagus, pharynx, and larynx. We calculated the correlation between improved globus sensation and improved gastric emptying to investigate the association between rikkunshito-induced stimulation of gastric emptying improved globus sensation. We found a significant positive correlation between improved globus sensation and improved gastric emptying. Thus, the improvement in globus sensation following treatment with rikkunshito may be the result, at least in part, of improved gastric emptying. In addition to the globus sensation, patients with LPR typically experience sore throat or excessive throat clearing. Treatment with rikkunshito plus PPI, but not with rikkunshito alone, improved the tingling sensation in patients with PPI-refractory LPR in the present study, suggesting that acid may play a greater role in causing a sore throat than in globus sensation. Moreover, the LPR symptoms of globus sensation, sore throat, and excessive throat clearing may be induced by different mechanism. Johnston et al[25] reported absence or decreased expression of mucosal-protective proteins in laryngeal epithelial cells in 64% of patients with LPR. Thus, reducing the gastric content that passes into the laryngopharyngeal tissue via mucosal defenses may be an effective treatment for LPR. Rikkunshito has an effect on mucosal defenses in the gastroesophageal region, although the effect in the laryngopharynx is unclear[26,27]. In addition to the inhibitory effects of PPIs on acid, rikkunshito-induced stimulation of gastric emptying and effects on mucosal defense may contribute to the improvement in sore throat in the laryngopharynx.
The present study demonstrated that rikkunshito did not improve gastrointestinal symptoms in patients with PPI-refractory LPR assessed using the GSRS. In contrast, rikkunshito has been shown to improve upper gastrointestinal symptoms in PPI-refractory GERD patients assessed using the frequency scale for the symptoms of GERD score[12]. This discrepancy may be related to differences in the pathology and/or assessment tools used in the two studies.
In conclusion, rikkunshito treatment improved the globus sensation in patients with PPI-refractory LPR. The effect may be the result, at least in part, of the stimulation of gastric emptying. Rikkunshito plus PPI therapy may be an effective novel therapeutic strategy for PPI-refractory LPR symptoms, including globus sensation and sore throat.
Regarding the treatment of laryngopharyngeal reflux (LPR) symptoms such as globus sensation and a scratchy feeling, proton pump inhibitors (PPIs) are considered the mainstay. However, cases exist in which extraesophageal symptoms in the laryngopharynx are not improved by PPI.
Recently, gastroesophageal reflux disease (GERD) has been considered a major cause of globus. However, the etiology of globus remains unclear. The authors have demonstrated that the cause of the globus sensation is elevated upper esophageal sphincter pressure, resulting from gastroesophageal reflux without direct exposure of the hypopharynx to acid.
Stimulation of gastric emptying or esophageal clearance in addition to inhibition of gastric acid secretion may also be efficacious in the treatment of LPR. It has been reported that addition of prokinetics, such as cisapride and itopride, to PPIs in the treatment of LPR reduced the recurrence of symptoms. However, there are few reports of the efficacy of prokinetics in the treatment of LPR.
Rikkunshito, a traditional Japanese medicine, has a dual action on the stomach: relaxation of the proximal stomach and contraction of the distal stomach. Recently, it was reported that rikkunshito improved upper gastrointestinal symptoms in PPI-refractory GERD patients. This was a prospective, randomized, parallel comparative study performed to examine the efficacy and safety of a therapeutic strategy using rikkunshito in patients with PPI-refractory LPR.
The authors examined the effect of an herbal medicine “rikkunshito” on symptoms and gastric emptying in patients with LPR. The outcome of the study is interesting and important for the care of patients with PPI-refractory LPR.
P- Reviewers Huerta-Franco MR, Tosetti C S- Editor Wen LL L- Editor A E- Editor Li JY
| 1. | Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101:1-78. [PubMed] |
| 2. | Koufman J, Sataloff RT, Toohill R. Laryngopharyngeal reflux: consensus conference report. J Voice. 1996;10:215-216. [PubMed] |
| 3. | Sataloff RT, Castell DO, Katz PO, Sataloff DM. Reflux Laryngitis and Related Disorders. 2nd ed. Albany, New York: Delmar Thomson Learning 2003; . |
| 4. | Halum SL, Butler SG, Koufman JA, Postma GN. Treatment of globus by upper esophageal sphincter injection with botulinum A toxin. Ear Nose Throat J. 2005;84:74. [PubMed] |
| 5. | Corso MJ, Pursnani KG, Mohiuddin MA, Gideon RM, Castell JA, Katzka DA, Katz PO, Castell DO. Globus sensation is associated with hypertensive upper esophageal sphincter but not with gastroesophageal reflux. Dig Dis Sci. 1998;43:1513-1517. [PubMed] |
| 6. | Tokashiki R, Funato N, Suzuki M. Globus sensation and increased upper esophageal sphincter pressure with distal esophageal acid perfusion. Eur Arch Otorhinolaryngol. 2010;267:737-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Ford CN. Evaluation and management of laryngopharyngeal reflux. JAMA. 2005;294:1534-1540. [PubMed] |
| 8. | Dore MP, Pedroni A, Pes GM, Maragkoudakis E, Tadeu V, Pirina P, Realdi G, Delitala G, Malaty HM. Effect of antisecretory therapy on atypical symptoms in gastroesophageal reflux disease. Dig Dis Sci. 2007;52:463-468. [PubMed] |
| 9. | Galli J, Cammarota G, De Corso E, Agostino S, Cianci R, Almadori G, Paludetti G. Biliary laryngopharyngeal reflux: a new pathological entity. Curr Opin Otolaryngol Head Neck Surg. 2006;14:128-132. [PubMed] |
| 10. | Ezzat WF, Fawaz SA, Fathey H, El Demerdash A. Virtue of adding prokinetics to proton pump inhibitors in the treatment of laryngopharyngeal reflux disease: prospective study. J Otolaryngol Head Neck Surg. 2011;40:350-356. [PubMed] |
| 11. | Kawahara H, Kubota A, Hasegawa T, Okuyama H, Ueno T, Ida S, Fukuzawa M. Effects of rikkunshito on the clinical symptoms and esophageal acid exposure in children with symptomatic gastroesophageal reflux. Pediatr Surg Int. 2007;23:1001-1005. [PubMed] |
| 12. | Tominaga K, Iwakiri R, Fujimoto K, Fujiwara Y, Tanaka M, Shimoyama Y, Umegaki E, Higuchi K, Kusano M, Arakawa T. Rikkunshito improves symptoms in PPI-refractory GERD patients: a prospective, randomized, multicenter trial in Japan. J Gastroenterol. 2012;47:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Tatsuta M, Iishi H. Effect of treatment with liu-jun-zi-tang (TJ-43) on gastric emptying and gastrointestinal symptoms in dyspeptic patients. Aliment Pharmacol Ther. 1993;7:459-462. [PubMed] |
| 14. | Kusunoki H, Haruma K, Hata J, Ishii M, Kamada T, Yamashita N, Honda K, Inoue K, Imamura H, Manabe N. Efficacy of Rikkunshito, a traditional Japanese medicine (Kampo), in treating functional dyspepsia. Intern Med. 2010;49:2195-2202. [PubMed] |
| 15. | Kido T, Nakai Y, Kase Y, Sakakibara I, Nomura M, Takeda S, Aburada M. Effects of rikkunshi-to, a traditional Japanese medicine, on the delay of gastric emptying induced by N(G)-nitro-L-arginine. J Pharmacol Sci. 2005;98:161-167. [PubMed] |
| 16. | Revicki DA, Wood M, Wiklund I, Crawley J. Reliability and validity of the Gastrointestinal Symptom Rating Scale in patients with gastroesophageal reflux disease. Qual Life Res. 1998;7:75-83. [PubMed] |
| 17. | Cremonini F, Mullan BP, Camilleri M, Burton DD, Rank MR. Performance characteristics of scintigraphic transit measurements for studies of experimental therapies. Aliment Pharmacol Ther. 2002;16:1781-1790. [PubMed] |
| 18. | Hattori T. Rikkunshito and ghrelin. Int J Pept. 2010;2010. [PubMed] |
| 19. | Nakai Y, Kido T, Hashimoto K, Kase Y, Sakakibara I, Higuchi M, Sasaki H. Effect of the rhizomes of Atractylodes lancea and its constituents on the delay of gastric emptying. J Ethnopharmacol. 2003;84:51-55. [PubMed] |
| 20. | Takahashi T, Endo S, Nakajima K, Souma Y, Nishida T. Effect of rikkunshito, a chinese herbal medicine, on stasis in patients after pylorus-preserving gastrectomy. World J Surg. 2009;33:296-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Takeda H, Sadakane C, Hattori T, Katsurada T, Ohkawara T, Nagai K, Asaka M. Rikkunshito, an herbal medicine, suppresses cisplatin-induced anorexia in rats via 5-HT2 receptor antagonism. Gastroenterology. 2008;134:2004-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 231] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 22. | Matsumura T, Arai M, Yonemitsu Y, Maruoka D, Tanaka T, Suzuki T, Yoshikawa M, Imazeki F, Yokosuka O. The traditional Japanese medicine Rikkunshito increases the plasma level of ghrelin in humans and mice. J Gastroenterol. 2010;45:300-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 23. | Fujitsuka N, Asakawa A, Uezono Y, Minami K, Yamaguchi T, Niijima A, Yada T, Maejima Y, Sedbazar U, Sakai T. Potentiation of ghrelin signaling attenuates cancer anorexia-cachexia and prolongs survival. Transl Psychiatry. 2011;1:e23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 24. | Nahata M, Muto S, Oridate N, Ohnishi S, Nakagawa K, Sadakane C, Saegusa Y, Hattori T, Asaka M, Takeda H. Impaired ghrelin signaling is associated with gastrointestinal dysmotility in rats with gastroesophageal reflux disease. Am J Physiol Gastrointest Liver Physiol. 2012;303:G42-G53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Johnston N, Bulmer D, Gill GA, Panetti M, Ross PE, Pearson JP, Pignatelli M, Axford SE, Dettmar PW, Koufman JA. Cell biology of laryngeal epithelial defenses in health and disease: further studies. Ann Otol Rhinol Laryngol. 2003;112:481-491. [PubMed] |
| 26. | Arakawa T, Higuchi K, Fujiwara Y, Watanabe T, Tominaga K, Hayakawa T, Kuroki T. Gastroprotection by Liu-Jun-Zi-Tang (TJ-43): possible mediation of nitric oxide but not prostaglandins or sulfhydryls. Drugs Exp Clin Res. 1999;25:207-210. [PubMed] |
| 27. | Miwa H, Koseki J, Oshima T, Kondo T, Tomita T, Watari J, Matsumoto T, Hattori T, Kubota K, Iizuka S. Rikkunshito, a traditional Japanese medicine, may relieve abdominal symptoms in rats with experimental esophagitis by improving the barrier function of epithelial cells in esophageal mucosa. J Gastroenterol. 2010;45:478-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |