Published online Jan 21, 2013. doi: 10.3748/wjg.v19.i3.362
Revised: December 11, 2012
Accepted: December 15, 2012
Published online: January 21, 2013
AIM: To compare the impact of the right recumbent position with the sitting position on gastric emptying of water.
METHODS: In eight healthy male volunteers, the 13C acetate breath test was performed twice to assess gastric emptying of 100 mL tap water. Subjects were seated in one test and lying on their right side in the other. In both positions, pulmonary 13CO2 exhalation curves were obtained by plotting breath data against time. Percent gastric retention curves were created by analyzing data using the Wagner-Nelson protocol.
RESULTS: No significant posture effect was found in pulmonary 13CO2 output curves (P = 0.2150), whereas a significant effect was seen in gastric retention curves (P = 0.0315). The percent retention values at 10 min and 15 min were significantly smaller when subjects were in the right recumbent position compared with the seated position (P < 0.05). Our results verified the accelerating effect of the right recumbent position on gastric emptying of non-nutritive solutions. Concerning clinical implications, this study suggests that placing patients with acute pain on their right side after oral administration of analgesic drugs in solution is justified as an effective practice for rapid pain relief. For patients with gastrointestinal reflux symptoms, sleeping in the right recumbent position may reduce nocturnal symptoms, as delayed gastric emptying can cause reflux symptoms.
CONCLUSION: Gastric emptying of water occurs more quickly when a subject lies on the right side compared with sitting.
- Citation: Sanaka M, Urita Y, Yamamoto T, Shirai T, Kimura S, Aoyagi H, Kuyama Y. Right recumbent position on gastric emptying of water evidenced by 13C breath testing. World J Gastroenterol 2013; 19(3): 362-365
- URL: https://www.wjgnet.com/1007-9327/full/v19/i3/362.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i3.362
Gastric emptying of orally ingested contents is a great concern to clinicians because it is associated with gastrointestinal symptoms and can affect the efficacy of medications. Little absorption takes place in the stomach, and any oral medication must therefore pass beyond the stomach before being absorbed within the small intestine. The rate of gastric emptying is determined by the balance between the propulsive force (fundic tonic pressure and antral contractions) and the outlet resistance (pyloric and duodenal contractions). For calorie-containing meals, the force-resistance balance is primarily regulated by the nutrient-evoked feedback loop that strictly controls duodenal entry of meals so as to optimize intestinal absorption of nutrients[1]. On the other hand, for non-caloric fluids (e.g., water and normal saline), the feedback system is barely activated and consequently, the stomach behaves like “a motionless bag” in which the fluids passively flow back and forth depending on gravity[2]. Considering this gravity-dependent flow, the idea has been proposed that, among the variety of body positions, the right lateral recumbent position makes emptying of non-nutritive fluids the fastest[3].
Positioning a patient has traditionally been regarded as an effective maneuver to modulate the absorption of orally administered drugs in solution. In the case of oral overdosing, for which drug absorption should be delayed, being recumbent on the left side (“pylorus up” status) is advisable.; In the case of acute pain, for which the rapid onset of analgesic effect is favored, being recumbent on the right side (“pylorus down” status) is recommended. Indeed, the delaying effect of the left recumbent position on gastric emptying of non-caloric liquids has been well documented. However, the evidence that the right recumbent position enhances liquid emptying is much less certain[4]. According to a recent review on the postural effect on gastric emptying[4], only one trial supports the enhanced emptying of non-nutritive liquids in the right recumbent position, showing that emptying is significantly faster than in the left recumbent position[2]. However, this result only suggests that emptying in the left recumbent position is slower than that in the right.
The present study was conducted to elucidate whether gastric emptying of water is faster when lying on the right side than when seated. The sitting position is regarded as “neutral” if the effect of the gravity over intragastric fluids is accounted for, and was thereby set as the reference posture. The 13C-acetate breath test with Wagner-Nelson analysis was used to measure gastric emptying accurately without any invasive procedures.
Eight healthy male volunteers (age: 19-52 years, median 38 years; weight: 48.0-80.2 kg, median 64.0 kg) participated in this study. No subject had a history of, or symptoms referable to, gastrointestinal and pulmonary disease or chronic medical problems. Additionally, no subjects were receiving medication at the time of the study. Written informed consent was obtained from each volunteer. The study protocol was approved by the Ethics Committee of Toho University.
The 13C-acetate breath test was used to assess gastric emptying [5]. The assessment was carried out on two randomized occasions, at least 3 d apart, with subjects either seated or lying on their right side. On both occasions, subjects had fasted overnight, and they drank 100 mL tap water labeled with 100 mg 13C-acetate in the sitting position. Breath samples were collected at baseline and, following ingestion of the water, at 5-min intervals for the first 20 min and at 10-min intervals thereafter up to 120 min. On one occasion, the subjects remained seated throughout the 120-min period. On the other occasion, immediately after drinking the test solution, they lay down on their right side and maintained the position until they exhaled the 15-min breath sample; thereafter they remained seated.
Breath 13CO2 isotopic enrichment was determined using non-dispersive infrared isotope spectrometry (UbiT-IR 300; Otsuka Electronics, Osaka, Japan). The pulmonary recovery of 13CO2 was expressed in %dose/h based on the body surface area and the assumed CO2 production. The %dose/h recovery values were plotted against time to create the time-breath 13CO2 excretion curve, which indirectly reflects gastric emptying. The time to the maximal recovery (Tmax), a semi-quantitative index of gastric emptying, was determined by visual inspection of the 13CO2 output curve[6]. The breath data were further analyzed using the Wagner-Nelson method, which enables creation of a percent gastric retention-time curve that is as accurate as the scintigraphic emptying curve[7]. The Wagner-Nelson procedure has been detailed elsewhere[7,8]. In short, estimated fraction of the labeled test meal that has been emptied from the stomach by time t, F(t), is obtained from the conventional equation; F(t) = area under the concentration curve (AUC)(t)/AUC(infinite), although the value can differ from those obtained using the scintigraphic method. Wagner-Nelson method allows accurate estimation of F(t) using the revised equation as follows: F(t) = [AUC(t) + C(t)/Kel]/AUC(infinite). In the equation, Kel (1/h) is the first-order rate constant for total elimination of 13CO2 from the human body, C(t) is the 13CO2 excretion rate (%dose/h), AUC(t) is the area under the C(t) curve (%dose) (= the pulmonary recovery of 13CO2), and AUC(infinite) is the cumulative amount of 13CO2 recovered in the breath at the infinite time (% dose).
The time by which half of the water has been emptied (t1/2), which is used as the standard index in gastric emptying scintigraphy, was determined by interpolation from the retention-time curve[7].
Differences in the pulmonary 13CO2 output and the percent gastric retention curves between the two postures were assessed with repeated measures of analysis of variance (ANOVA) using “posture” and “time” as factors. When the ANOVA showed a significant difference, it was followed by post hoc comparisons at each measurement time with Student’s paired t test with Bonferroni adjustment. The tmax and t1/2 values are presented as mean ± SD. Differences in tmax and t1/2 between the two body positions were also assessed with Student’s paired t test. The level of significance was set at P = 0.05 (two-sided probability).
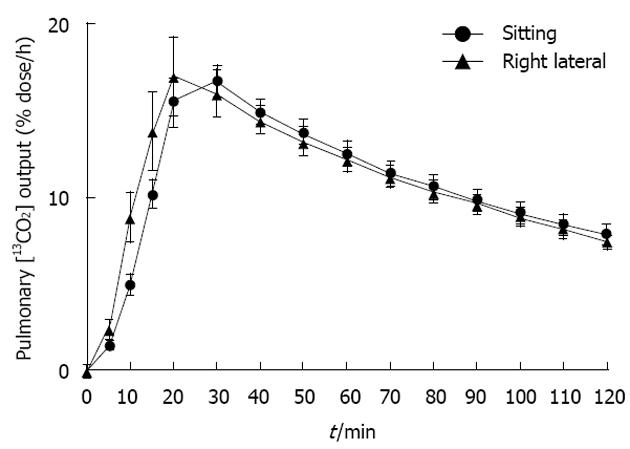
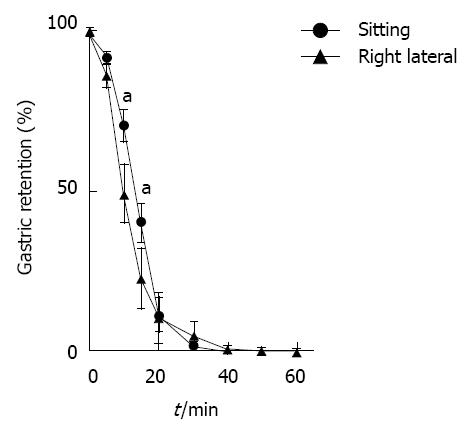
No significant posture effect was found in pulmonary 13CO2 output curves (P = 0.2150; Figure 1), whereas a significant effect was found in gastric retention curves (P = 0.0315; Figure 2). The post hoc comparisons revealed that the percent retention values were significantly smaller in the right recumbent position at 10 min (P < 0.01) and at 15 min (P < 0.05). On the other hand, neither Tmax nor t1/2 was significantly different between the two positions (Tmax: 25.0 ± 5.35 min in the sitting position and 23.1 ± 9.23 min in the right recumbent position; P = 0.644, t1/2: 13.7 ± 2.79 min in the sitting position and 11.6 ± 5.92 min in the right recumbent position; P = 0.378).
It seems natural that non-caloric fluids in the stomach should gravitate toward the duodenum in the right recumbent position. It is, therefore, reasonable to assume that the right recumbent position would hasten gastric emptying of fluids compared to a sitting position. However, this assumption has not been verified. The present results provided clear evidence that water is emptied significantly faster when a subject is in the right recumbent position than when seated.
Burn-Murdoch et al[2] showed that emptying of saline was significantly faster in the right recumbent position than in the left recumbent position whereas it was not significantly different between the right recumbent position and the seated position. We think that the lack of significant difference between the right recumbent position and the seated position in that study might be due to the suboptimal protocol used to measure gastric emptying: the emptying was quantified as the volume aspirated via a nasogastric tube at 10 min after ingestion of 750-mL saline. The aspiration technique appears unreliable to measure residual gastric volume[9].
In the present study, the gastric retention at 10 and 15 min indicated a significant positional effect (Figure 2), whereas the pulmonary 13CO2 output curve did not (Figure 1). This is possibly because the Wagner-Nelson modification improved the accuracy of breath testing. In contrast to gastric scintigraphy, which allows direct visualization of duodenal transit of gastric contents[10], the conventional 13C-acetate breath test indirectly reflects gastric emptying and thus is less sensitive[6]. The Wagner-Nelson analytical strategy has been introduced into the breath test system to overcome its indirect nature, making the 13C-breath test as accurate as the “gold standard” of scintigraphy[7]. Gastric emptying of non-nutrient fluids in the sitting position per se is so rapid that conventional breath testing would have overlooked a subtle, albeit real acceleration of emptying in the right recumbent position. This subtle difference would be detected only by the gastric retention curve created by Wagner-Nelson analysis. The t1/2 values were not significantly different between the two body positions even though values were derived from the “accurate” Wagner-Nelson analysis. This is probably because the t1/2 value itself would be a less accurate parameter than the percent gastric retention at a fixed time point, as shown in the expert recommended guidelines for scintigraphic gastric emptying studies[10].
There are some limitations to the present study. First, we used only a small sample size. Second, only a small volume of tap water was used. A larger volume may influence the results.
In conclusion, our results verified the accelerating effect of the right recumbent position on gastric emptying of non-nutritive solutions. Concerning clinical implications, this study suggests that placing patients with acute pain on their right side after oral administration of analgesic drugs in solution is justified as an effective practice for rapid pain relief. For patients with gastrointestinal reflux symptoms, sleeping in the right recumbent position may reduce nocturnal symptoms, as delayed gastric emptying can cause reflux symptoms.
Conventionally, gastric emptying of non-caloric fluids is thought to be accelerated when a person is in the right recumbent position. However, evidence supporting this hypothesis is weak. The present study compared the impact of the right recumbent position with the sitting position on gastric emptying of water.
For calorie-containing meals, the force-resistance balance is primarily regulated by the nutrient-evoked feedback loop that strictly controls duodenal entry of meals so as to optimize intestinal absorption of nutrients. On the other hand, for non-caloric fluids, the feedback system is barely activated and consequently, the stomach behaves like “a motionless bag” in which the fluids passively flow back and forth depending on gravity.
The present study was conducted to elucidate whether gastric emptying of water is faster when lying on the right side than when seated. The sitting position is regarded as “neutral” if the effect of the gravity over intragastric fluids is accounted for, and was thereby set as the reference posture. The 13C-acetate breath test with Wagner-Nelson analysis was used to measure gastric emptying accurately without any invasive procedures.
Their results verified the accelerating effect of the right recumbent position on gastric emptying of non-nutritive solutions. Concerning clinical implications, this study suggests that placing patients with acute pain on their right side after oral administration of analgesic drugs in solution is justified as an effective practice for rapid pain relief. For patients with gastrointestinal reflux symptoms, sleeping in the right recumbent position may reduce nocturnal symptoms, as delayed gastric emptying can cause reflux symptoms.
This is a prospective study to evaluate the gastric emptying of non-caloric liquids in a seated position versus right lateral recumbence. A total of 8 healthy male volunteers were given 100 mL of tap water labeled with 13C-acetate and evaluated in a seated position on one occasion and, on a separate day, evaluated in a right lateral recumbence position. Breath samples were collected at given intervals and tested for the pulmonary recovery of 13CO2. The values were plotted against time to create a time-breath 13CO2 excretion curve, which is an indirect measurement of the gastric emptying. The Wagner-Nelson procedure was then used to further analyze the data and extrapolate percent gastric retention-time curve.
P- Reviewers Koch TR, Ghoshal UC S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Schulze K. Imaging and modelling of digestion in the stomach and the duodenum. Neurogastroenterol Motil. 2006;18:172-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 172] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Burn-Murdoch R, Fisher MA, Hunt JN. Does lying on the right side increase the rate of gastric emptying? J Physiol. 1980;302:395-398. [PubMed] |
| 3. | Vance MV, Selden BS, Clark RF. Optimal patient position for transport and initial management of toxic ingestions. Ann Emerg Med. 1992;21:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Queckenberg C, Fuhr U. Influence of posture on pharmacokinetics. Eur J Clin Pharmacol. 2009;65:109-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Braden B, Adams S, Duan LP, Orth KH, Maul FD, Lembcke B, Hör G, Caspary WF. The [13C]acetate breath test accurately reflects gastric emptying of liquids in both liquid and semisolid test meals. Gastroenterology. 1995;108:1048-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 209] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Sanaka M, Nakada K. Stable isotope breath tests for assessing gastric emptying: A comprehensive review. J Smooth Muscle Res. 2010;46:267-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Sanaka M, Nakada K, Nosaka C, Kuyama Y. The Wagner-Nelson method makes the [13C]-breath test comparable to radioscintigraphy in measuring gastric emptying of a solid/liquid mixed meal in humans. Clin Exp Pharmacol Physiol. 2007;34:641-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Sanaka M, Yamamoto T, Ishii T, Kuyama Y. The Wagner-Nelson method can generate an accurate gastric emptying flow curve from CO2 data obtained by a 13C-labeled substrate breath test. Digestion. 2004;69:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Parrish CR, McClave SA. Checking gastric residual volumes-A practice in search of science? Prac Gastroenterol. 2008;32:33-47. |
| 10. | Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, McCallum RW, Nowak T, Nusynowitz ML, Parkman HP. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 458] [Cited by in RCA: 461] [Article Influence: 27.1] [Reference Citation Analysis (0)] |