Published online May 7, 2013. doi: 10.3748/wjg.v19.i17.2723
Revised: March 8, 2013
Accepted: March 21, 2013
Published online: May 7, 2013
Processing time: 79 Days and 14.3 Hours
Endoscopic hemostasis performed in the emergency room is difficult due to the presence of blood clots and food residue that makes obtaining a clear view of the bleeding vessel difficult. We experienced the efficacy of a newly developed inverted overtube to shorten the hemostatic time and obtain a clear endoscopic view with upper gastrointestinal bleeding patient who were transferred by ambulance car and required emergency endoscopy. The technique improved the endoscopic views and enabled us to perform the hemostatic procedures from the conventional standing position while freely and easily changing the patient’s position. The presence of blood clots and food residue in the gastric fornix or upper gastric body makes identifying a bleeding exposed vessel impossible. This set-up significantly shortened the procedure time. The inverted overtube helped us obtain a clear view in patients who were laid in the right lateral position. Rapid identification of exposed vessels resulted in success of hemostasis.
Core tip: The inverted overtube helped us obtain a clear view in patients who were laid in the right lateral position. Rapid identification of exposed vessels resulted in success of hemostasis.
- Citation: Mori H, Kobara H, Fujihara S, Nishiyama N, Oryu M, Rafiq K, Masaki T. Accurate hemostasis with a new endoscopic overtube for emergency endoscopy. World J Gastroenterol 2013; 19(17): 2723-2726
- URL: https://www.wjgnet.com/1007-9327/full/v19/i17/2723.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i17.2723
Patients with upper gastrointestinal bleeding who are transferred by an ambulance commonly present in emergency rooms and require an emergency endoscopy to achieve hemostasis. Although the significance, indication and timing of emergency endoscopies are controversial[1,2], in the case of esophageal or gastric varix or Dieulafoy’s ulcer, exposed vessels with spurting bleeding require prompt hemostasis, and failure to achieve hemostasis may lead to a serious condition. Endoscopists are under pressure to perform these emergency endoscopic treatments, especially in patients with cardiovascular or cerebrovascular diseases who are being treated with antiplatelet and anticoagulant agents[3] or in seriously ill patients who require rapid and reliable hemostasis[4]. In almost all cases, once the bleeding site is visually identified by endoscopy, hemostasis can be achieved using current endoscopic techniques and hemostatic forceps[5]; however, if it cannot be visually identified, a surgical procedure is required[6-8]. The presence of blood clots and food residue in the gastric fornix or upper gastric body makes identifying a bleeding exposed vessel impossible. In the case of gastric variceal bleeding, erythromycin or somatostatin has a beneficial effect on upper gastrointestinal bleeding by inducing rapid gastric emptying[9,10]. However, even with such drugs, obtaining a clear endoscopic view to rapidly identify the bleeding exposed vessels in an emergency situation is still difficult. This case series demonstrates a method for shortening the hemostasis time and reducing stress for both patients and endoscopists.
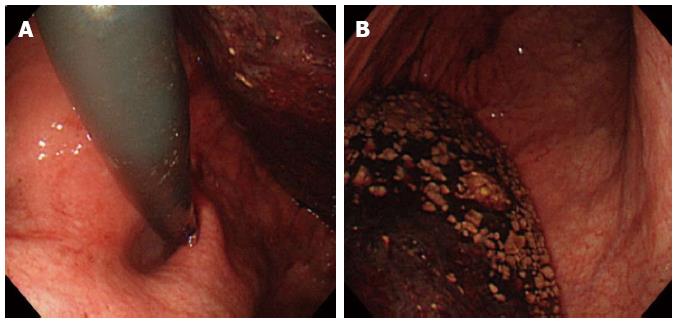
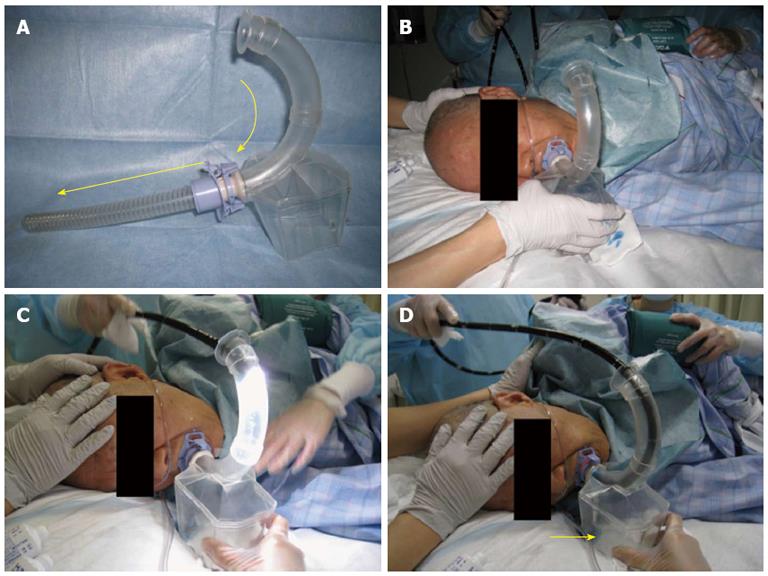
A 55-year-old woman who was transported to our emergency room in shock after feeling nauseous and experiencing sudden massive hematemesis in June 2012. Although her family informed us that a blood test 6 mo prior had shown no signs of anemia, a blood examination revealed severe anemia (hemoglobin, 5.5 g/dL). Emergency endoscopic hemostasis and a blood transfusion were performed. Large amounts of blood and food residue were observed in the stomach. Because the patient appeared drowsy, an emergency endoscopy to detect the bleeding vessel was immediately performed in the areas that could be observed in the left lateral decubitus position. The bleeding vessel could not be identified in the duodenum or gastric antrum. As the amount of fresh blood increased, obtaining a clear endoscopic view to identify the bleeding vessel gradually increased in difficulty (Figure 1). Assuming that the bleeding vessel was located in either the upper gastric body or gastric fornix, which was not visible due to the blood clot, we immediately switched from the conventional observation position to the right lateral decubitus position using newly developed inverted overtube (Figure 2). The inverted overtube was approved by the Institutional Ethics Committee of Kagawa University Hospital, Kagawa, Japan. Additionally, the inverted overtube was approved by the Japanese Pharmaceutical Law.
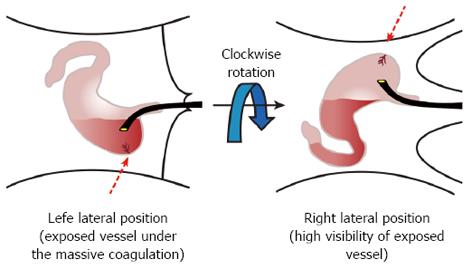
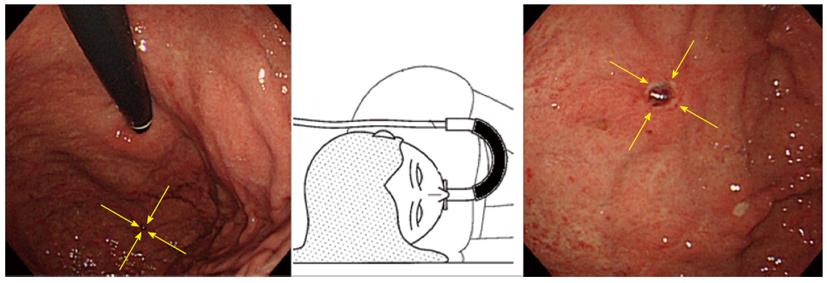
The blood clot and food residue in the gastric corpus and fornix were immediately dislodged to the right into the duodenum by gravity (Figure 3), allowing for the visual identification of an exposed blood vessel in the fornix (Figure 4). Up to this point, no spurting bleeding had been observed due to the decreased blood pressure. However, massive spurting bleeding occurred immediately after the exposed blood vessel was pinched with hemostatic forceps. The pinched vessel was then completely cauterized by coagulation mode to achieve hemostasis. No bleeding was observed thereafter.
Despite the dramatic progress made in endoscopic hemostatic techniques[1,4], hematemesis from an esophageal or gastric varix or Dieulafoy’s ulcer can lead to serious consequences if hemostasis is not achieved[8]. Achieving accurate and reliable hemostasis is difficult without a clear view of the bleeding vessel. Although hemostasis via a laparotomy can be performed as a last resort, surgery in a patient with a poor systemic condition carries a high risk. Thus, emergency endoscopic hemostasis remains the first-line treatment of choice[2,6].
During endoscopic hemostatic procedures performed in the emergency room, where pretreatment is not performed, the presence of blood clots and food residue makes obtaining a clear view of the bleeding vessel difficult[5]. The removal of blood clots from the stomach has conventionally been achieved by gastric suction with a gastric tube and/or by manual removal of the clot with grasping forceps. However, the use of gastric suction and/or grasping forceps currently requires a great deal of time. Thus, endoscopists have adopted a procedure in which the patient’s posture is rotated to the right lateral decubitus position to dislodge the blood clots and enable the identification of the bleeding vessel. Because most endoscopists perform conventional endoscopic examinations and treatment procedures with the patient lying in the left lateral decubitus position, they find that performing accurate hemostatic procedures from the opposite side, with the patient lying in the right lateral decubitus position, to be difficult. Thus, the use of the inverted overtube is the best method to help endoscopists perform an emergency endoscopy with less stress because they are in their conventional standing position relative to patients who are rotated to the right lateral decubitus position, without changing the positions of the endoscopy unit and light source. This technique is the most effective way to dislodge blood clots and food residue by gravity in these patients. The present technique dramatically improved the clarity of the endoscopic views and enabled the endoscopist to perform the hemostatic procedures from the conventional standing position while freely and easily changing the patient’s position. This set-up significantly shortened the procedure time. The inverted overtube, with its very simple structure, helped the endoscopist acquire a clear view in patients who were laid in the right lateral position. This clear view contributed to the rapid identification of the bleeding vessels and the subsequent rapid achievement of hemostasis.
We thank Professor Yasuyuki Suzuki for technical and editorial assistance.
P- Reviewers Lin CH, Kikuyama M S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Apel D, Riemann JF. Emergency endoscopy. Can J Gastroenterol. 2000;14:199-203. [PubMed] |
| 2. | Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Use of endoscopy for management of acute upper gastrointestinal bleeding in the UK: results of a nationwide audit. Gut. 2010;59:1022-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 138] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Tseng PH, Liou JM, Lee YC, Lin LY, Yan-Zhen Liu A, Chang DC, Chiu HM, Wu MS, Lin JT, Wang HP. Emergency endoscopy for upper gastrointestinal bleeding in patients with coronary artery disease. Am J Emerg Med. 2009;27:802-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Cappell MS. Therapeutic endoscopy for acute upper gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2010;7:214-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Cooper GS, Kou TD, Wong RC. Use and impact of early endoscopy in elderly patients with peptic ulcer hemorrhage: a population-based analysis. Gastrointest Endosc. 2009;70:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Koenig AM, Gawad K, Yekebas E, Seewald S, Izbicki J. [Timing and concepts of surgical treatment of upper gastrointestinal haemorrhage]. Zentralbl Chir. 2010;135:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Cheng CL, Lee CS, Liu NJ, Chen PC, Chiu CT, Wu CS. Overlooked lesions at emergency endoscopy for acute nonvariceal upper gastrointestinal bleeding. Endoscopy. 2002;34:527-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Ding YJ, Zhao L, Liu J, Luo HS. Clinical and endoscopic analysis of gastric Dieulafoy’s lesion. World J Gastroenterol. 2010;16:631-635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Avgerinos A, Vlachogiannakos J, Viazis N, Raptis SA. Clearing the stomach before emergency endoscopy in cirrhotics with acute upper gastrointestinal bleeding. A gastrokinetic or a vasoactive drug? J Hepatol. 2003;39:130-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Coffin B, Pocard M, Panis Y, Riche F, Lainé MJ, Bitoun A, Lémann M, Bouhnik Y, Valleur P. Erythromycin improves the quality of EGD in patients with acute upper GI bleeding: a randomized controlled study. Gastrointest Endosc. 2002;56:174-179. [PubMed] |