Published online Dec 14, 2012. doi: 10.3748/wjg.v18.i46.6850
Revised: September 23, 2012
Accepted: October 16, 2012
Published online: December 14, 2012
AIM: To evaluate the safety and effectiveness of laparoscopy compared with laparotomy for diagnosing and treating small bowel injuries (SBIs) in a porcine model.
METHODS: Twenty-eight female pigs were anesthetized and laid in the left recumbent position. The SBI model was established by shooting at the right lower quadrant of the abdomen. The pigs were then randomized into either the laparotomy group or the laparoscopy group. All pigs underwent routine exploratory laparotomy or laparoscopy to evaluate the abdominal injuries, particularly the types, sites, and numbers of SBIs. Traditional open surgery or therapeutic laparoscopy was then performed. All pigs were kept alive within the observational period (postoperative 72 h). The postoperative recovery of each pig was carefully observed.
RESULTS: The vital signs of all pigs were stable within 1-2 h after shooting and none of the pigs died from gunshot wounds or SBIs immediately. The SBI model was successfully established in all pigs and definitively diagnosed with single or multiple SBIs either by exploratory laparotomy or laparoscopy. Compared with exploratory laparotomy, laparoscopy took a significantly longer time for diagnosis (41.27 ± 12.04 min vs 27.64 ± 13.32 min, P = 0.02), but the time for therapeutic laparoscopy was similar to that of open surgery. The length of incision was significantly reduced in the laparoscopy group compared with the laparotomy group (5.27 ± 1.86 cm vs 15.73 ± 1.06 cm, P < 0.01). In the final post-mortem examination 72 h after surgery, both laparotomy and laparoscopy offered a definitive diagnosis with no missed injuries. Postoperative complications occurred in four cases (three following laparotomy and one following laparoscopy, P = 0.326). The average recovery period for bowel function, vital appearance, and food re-intake after laparoscopy was 10.36 ± 4.72 h, 14.91 ± 3.14 h, and 15.00 ± 7.11 h, respectively. All of these were significantly shorter than after laparotomy (21.27 ± 10.17 h, P = 0.004; 27.82 ± 9.61 h, P < 0.001; and 24.55 ± 9.72 h, respectively, P = 0.016).
CONCLUSION: Compared with laparotomy, laparoscopy offers equivalent efficacy for diagnosing and treating SBIs, and reduces postoperative complications as well as recovery period.
- Citation: Shan CX, Ni C, Qiu M, Jiang DZ. Is laparoscopy equal to laparotomy in detecting and treating small bowel injuries in a porcine model? World J Gastroenterol 2012; 18(46): 6850-6855
- URL: https://www.wjgnet.com/1007-9327/full/v18/i46/6850.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i46.6850
The vast anatomic space occupied by the gastrointestinal tract prediposes it to penetrating injuries. In penetrating trauma, the small bowel is most frequently injured, followed by the large intestine and stomach[1]. Small bowel injury (SBI) is seldom diagnosed preoperatively especially when there are no frank signs of hemoperitoneum or peritonitis[2,3].
Laparotomy is considered the gold standard for evaluation of intra-abdominal injuries sustained from trauma[4]. However, complications following negative or nontherapeutic laparotomy can be as high as 20%-40%[5-7]. Therefore, it is advantageous to avoid a negative laparotomy while providing a reliable and accurate alternative diagnostic procedure[8]. While laparoscopy has become a standard component of diagnosis and therapy for many conditions in general surgery, its role in trauma remains controversial. Many concerns about the safety, sensitivity, and specificity of laparoscopy have limited its application in abdominal trauma[9-12], particularly in detecting SBIs[13-15]. It was reported that laparoscopy in trauma initially resulted in a high rate of missed injuries (41%-77%) and considerable criticism of laparoscopy as a diagnostic tool[9,10]. Studies in 1993 and 2006 showed little statistical change in its reliability; only 20% of SBIs were correctly identified by laparoscopy, and sensitivity was 25% for diagnosis of hollow viscus and retroperitoneal injuries[16,17]. The high proportion of missed occult SBIs with laparoscopy in trauma (LIT) is a major reason why some surgeons still preclude LIT use today[18]. These considerations conflict with the considerable advances that have been made in LIT.
In this present study we mimicked injuries to the small intestines by firing bullets into the abdomen of anesthetized pigs. We tried to provide a reproducible and hemodynamically stable porcine model with multiple SBIs. We also aimed to evaluate the safety and effectiveness of diagnostic and therapeutic laparoscopy compared with the laparotomy for SBI in the porcine model.
The study protocol was approved by the Institutional Review Board of the Research Institute of Surgery (RIS), which was affiliated to the Third Military Medical University in Chong Qing (People’s Republic of China). Animal welfare and experimental procedures were carried out strictly in accordance with the guide for the Animal Care and Use Committee of RIS.
A prospective, randomized, comparative study was conducted between February and July 2010. Enrolled in this research were 28 consecutive healthy pigs native to Chong Qing (all females). The pigs were provided and fed by staff from the Medical Animal Research Center of Da Ping Hospital (Affiliated to the Third Military Medical University).
After mastering the skilled techniques gained from previous experience in modeling and treating SBIs, we carried out this study to ascertain if laparoscopy alone could replace laparotomy in diagnosing and treating SBIs in this porcine model.
All 28 pigs had free access to food and tap water without oral intake of antibiotics. After premedication with intramuscular administration of azaperone 4 mg/kg, ketamine 10 mg/kg, and atropine 0.02 mg/kg, general anesthesia was induced by 3% pentobarbital (1 mL/kg) via the left ear vein; an additional 3-5 mL of 3% pentobarbital was given if the pigs became restless. A 6.5-F endotracheal tube was applied, and pigs allowed to breathe spontaneously. They were ventilated with room air using a standard ventilator if necessary. Most of the animals were in the anesthetic plane between medium and deep anesthesia [muscles relaxed; most reflexes (palpebral, corneal) absent; pupillary light reflex slow or absent].
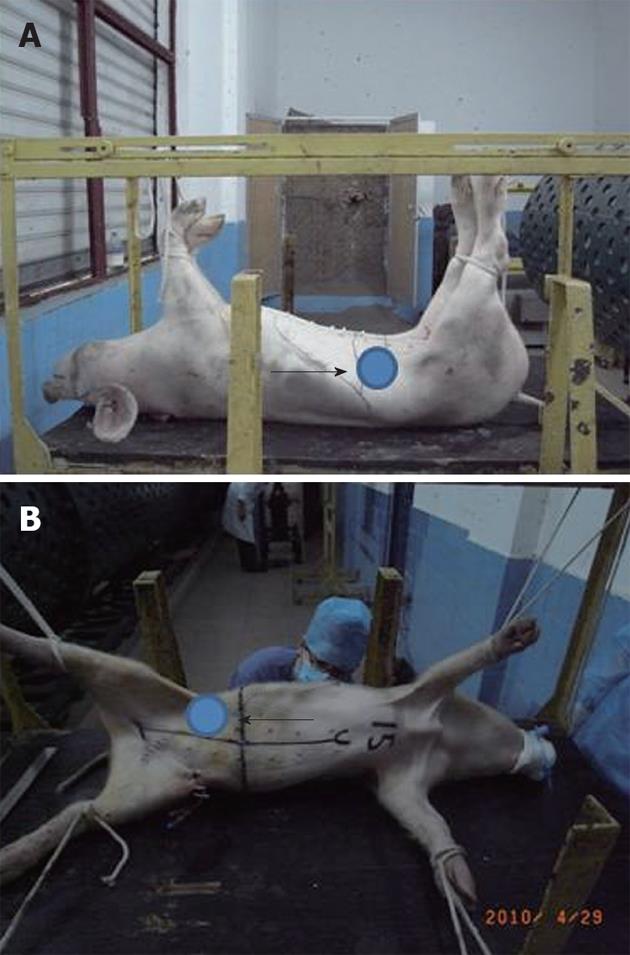
SBI modeling procedures: After anesthesia, the pigs were transferred to the shooting cabin to establish the model. Pigs were laid in the left lateral recumbent position; the right forelimb and hindlimb were abducted and suspended on the shooting shelf whereas the left forelimb and hindlimb were fixed horizontally. The entry point was 2 cm medial and 3 cm cephalad from the point of the right hip (this position was determined according to our previously experience). Once the entry point was defined, the location of the predicted exit point was obtained by ensuring that both points were in the right quadrant of the abdomen and the line between the two points was horizontal. The predicted exit point was equivalent to the entry point moving medially, and was 4 cm lateral to the abdominal midline (Figure 1).
The injury was inflicted by a 56-type military firearm. It fired 7.62-mm steel-core bullets weighing 7.9 g at a shooting distance of 5 meters. The military firearm was used after fine adjustment of the ballistic trajectory according to the position of animal. All devices and the professional marksman were provided by the RIS.
Surgical procedures: After shooting at the abdomen, pigs were rapidly transferred to the operating room. Immediately before surgery, all pigs were randomized to one of the two surgical approaches (laparotomy or laparoscopy). The interval between shooting and surgery was similar in each pig: approximately 70-80 min.
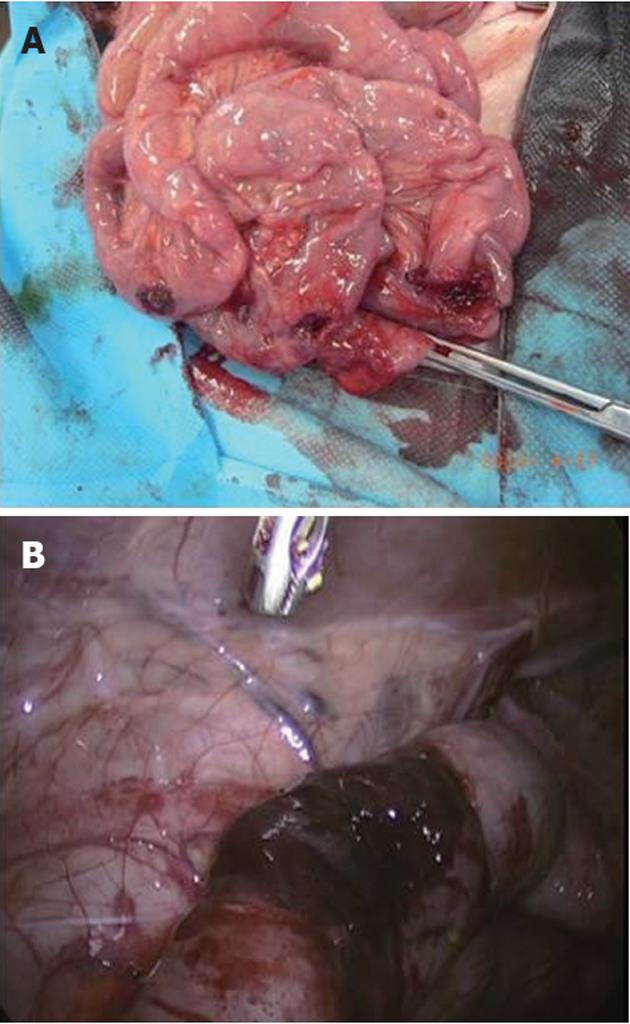
Laparotomy group: Pigs were placed in the supine position. Access to the abdominal cavity was gained through a midline incision ranging from approximately 7 cm above the umbilicus to approximately 9 cm below the umbilicus. The abdominal wall was drawn back with a metal retractor. Viscera (particularly the intestinal tract) were exposed manually. The sequence of exploration was from the major vessels, liver, spleen, the gyri centripetales and gyri centrifugales of the colon to the left kidney and left segment of the pancreas; this was continued from the sigmoid colon, rectum, bladder, and cecum to the ileum and jejunum; then continued from the stomach, duodenum, and the pancreatic head to the right segment of the pancreas and right kidney. After exploration, surgical treatment was performed for intra-abdominal injuries. Intestinal resection and anastomoses were undertaken if the diameter of the intestinal rupture was longer than 50% of the intestine circumference, otherwise simple repair with edge trimming was applied; end-to-end single-layer anastomoses were conducted with running number 0 silk sutures;
Laparoscopy group: A pneumoperitoneum of 13 mmHg with CO2 insufflation was established after insertion of a Veress needle. A 10-mm camera access port was introduced 1 cm above the umbilicus. A 30° laparoscope connected to a camera allowed endoscopic visualization. Two additional 5-mm or 10-mm ports were inserted in the left lower quadrant of the abdomen in right-angled triangular fashion under laparoscopic guidance. Pigs were positioned in a Trendelenburg angle or a reverse angle to facilitate free access to the intestinal tract and other viscera. The sequence of exploration and some of the specific rules of treatment during surgery were the same as those mentioned in the laparotomy. The small bowel was examined for traumatic injuries by two 5-mm atraumatic bowel graspers from the ileocecal valve to the ligament of Treitz (running the bowel). Once exploration was accomplished, effective therapeutic laparoscopic procedures were undertaken to treat the injuries. Larger bleedings were controlled through application of a laparoscopic clip or with bipolar forceps. If the intestinal injuries were not severe (injury scale lower than Grade II[19]) with the exception of ruptures of the colon or rectum, single repair with single-layer interrupted sutures was undertaken entirely under the laparoscopic view (total laparoscopy). Otherwise, intestinal resection and anastomoses were performed through an extended 5-cm incision of the exit wound (video-assisted laparoscopy).
After anastomoses and debridement, the abdominal cavity was irrigated with approximately 2000 mL normal (0.9%) saline, and a drainage tube placed in the pelvic cavity. The exit wound was managed with sharp debridement and two layers of interrupted sutures for the deep fascia and skin and the surgical incision. Administration of anesthetics was stopped. Both laparoscopy and laparotomy were performed by the same surgeons in our study, all of whom trained at RIS and used similar techniques.
Postoperatively, a clean dry dressing was sutured with the abdominal skin to prevent contamination of the incision. Each pig was transferred to the feeding room, kept in a single cage, and injected with 25 mg pethidine 3 h after surgery. All pigs received 500 mL 5% glucose solution containing 1 g cefradine and 0.5 g metronidazole per day through a peripheral vein. The eating habits and physical activities of the pigs were closely monitored three times daily to detect signs of peritonitis and generalized sepsis. The recovery of bowel function was recorded as the time of return of bowel sounds. At 72 h after surgery, all animals were sacrificed for a thorough exploration of the abdomen to check for missed injuries.
Statistical analysis were carried out with SPSS software (SPSS/PC + 16.0; SPSS, Chicago, IL, United States). Values are presented as mean ± standard deviation; P < 0.05 was considered significant. Statistical comparisons of data were carried out by the Student t-test, the Chi-square test or repeated measures as appropriate. In addition, Fisher’s exact test was applied if the sample was < 5.
The point of the entry wound was 2.1-2.9 cm medial (mean, 2.60 ± 0.19 cm) and 1.2-1.7 cm cephalad (mean, 1.5 ± 0.12 cm) from the point of the right hip. The exit wounds were located in the right lower quadrant of the abdomen, and 3.2-5.8 cm (mean, 4.53 ± 0.51 cm) lateral to the midline.
The vital signs of all pigs were stable within 1-2 h after shooting. None of the pigs died from gunshot wounds (GSW) to the abdomen. All 28 pigs underwent routine exploration of the abdominal cavity. All had single or multiple injuries to the small bowel, one (3.57%) with sigmoid ruptures (Figure 2), and one (3.57%) with cecum ruptures. Injuries to the liver, spleen, the gyri centripetales and gyri centrifugales of the colon, crucial vessels and retroperitoneal organs were not observed. The details of the SBIs are listed in Table 1; the organ injury scale was based on that of Moore et al[19]. In addition, the severity of SBIs in the two groups was also compared. We considered injury numbers of Grade II SBIs < 3 as minor injuries, and injury numbers of Grade III or more SBIs ≥ 1 as severe injuries. In the laparoscopy group, 5 cases were found with minor injuries and 9 cases with severe injuries, while in the laparotomy group, 4 cases were diagnosed with minor injuries and 10 cases with severe injuries. There was no significant difference between the groups concerning the severity of SBIs.
| Case | Injury scale1 of SB | Treatment | ||||||
| IH | IL | II | III | IV | V | Sum | ||
| 1 | 1 | 2 | 1 | 4 | Laparotomy | |||
| 2 | 1 | 1 | Laparoscopy (total) | |||||
| 3 | 2 | 1 | 2 | 5 | Laparoscopy (total) | |||
| 4 | 3 | 1 | 4 | 2 | 1 | 11 | Laparoscopy (video-assisted) | |
| 5 | 3 | 3 | Laparotomy | |||||
| 6 | 2 | 2 | 6 | 10 | Laparoscopy (video-assisted) | |||
| 7 | 3 | 4 | 7 | Laparotomy | ||||
| 8 | 1 | 2 | 3 | Laparotomy | ||||
| 9 | 1 | 1 | 1 | 3 | Laparoscopy (video-assisted) | |||
| 10 | 4 | 2 | 1 | 1 | 8 | Laparoscopy (video-assisted) | ||
| 11 | 1 | 2 | 3 | Laparotomy | ||||
| 12 | 1 | 1 | 3 | 2 | 1 | 8 | Laparotomy | |
| 13 | 1 | 2 | 1 | 1 | 5 | Laparotomy | ||
| 14 | 1 | 1 | 2 | Laparoscopy (total) | ||||
| 15 | 1 | 3 | 4 | 8 | Laparoscopy (video-assisted) | |||
| 16 | 1 | 2 | 1 | 1 | 5 | Laparotomy | ||
| 17 | 1 | 1 | 2 | 4 | Laparotomy | |||
| 18 | 2 | 1 | 1 | 4 | Laparotomy | |||
| 19 | 1 | 1 | 2 | Laparoscopy (total) | ||||
| 20 | 2 | 1 | 3 | Laparotomy | ||||
| 21 | 1 | 2 | 1 | 1 | 5 | Laparoscopy (video-assisted) | ||
| 22 | 1 | 1 | 2 | Laparotomy | ||||
| 23 | 2 | 3 | 1 | 6 | Laparoscopy (video-assisted) | |||
| 24 | 1 | 2 | 1 | 1 | 5 | Laparotomy | ||
| 25 | 1 | 1 | 1 | 3 | Laparoscopy (video-assisted) | |||
| 26 | 2 | 4 | 1 | 7 | Laparotomy | |||
| 27 | 1 | 1 | 2 | 4 | Laparoscopy (total) | |||
| 28 | 1 | 2 | 1 | 4 | Laparoscopy (video-assisted) | |||
All 28 pigs were randomized into either the laparotomy group or the laparoscopy group (14 in each group). According to the operative findings, both laparotomy and laparoscopy offered a definitive diagnosis with no missed injuries (all confirmed by the final post-mortem examination). Compared with laparotomy, laparoscopy took a significantly longer time for diagnosis (41.27 ± 12.04 min vs 27.64 ± 13.32 min, P = 0.02), but the time of therapeutic laparoscopy was similar to that of open surgery (83.27 ± 23.43 min vs 79.00 ± 19.17 min, P > 0.05). Furthermore, according to our analysis, the overall operative (diagnostic plus therapeutic) time was slightly longer in the laparoscopy group, but the difference did not reach statistical significance (P = 0.12). In addition, the length of the incision was significantly reduced in the laparoscopy group compared with the laparotomy group (5.27 ± 1.86 cm vs 15.73 ± 1.06 cm, P < 0.01).
Although all 28 pigs survived during the 72 h of follow-up, the recovery was not uneventful. Three cases (3/14, 21.5%) in the laparotomy group developed postoperative complications (one small bowel volvulus, one gastric retention, and one abdominal cavity infection and abscess) while only one case (1/14, 7.14%) had a complication of incisional infection in the laparoscopy group. No complications related to the technique (e.g., leakage, obstruction due to tight anastomosis, bleeding) were found. Although the incidence of complications was slightly higher following laparotomy, the difference between groups was not significant (P = 0.326). The average recovery period for bowel function, vital appearance, and food re-intake after laparoscopy was 10.36 ± 4.72 h, 14.91 ± 3.14 h, and 15.00 ± 7.11 h, respectively, following laparoscopy. All of these were significantly shorter than after laparotomy (21.27 ± 10.17 h, P = 0.004; 27.82 ± 9.61 h, P < 0.001; and 24.55 ± 9.72 h, respectively, P = 0.016).
Few studies have been carried out focusing on the methodology of SBI in pigs arising from GSW[20,21]. According to our experience, the entry and exit points were extremely critical in establishing a purely SBI model. Through our work on intra-abdominal anatomy, we found that the distribution pattern was considerably regular in pigs. The small bowel had a centralized distribution in the right abdomen, and the gyri centripetales and gyri centrifugales of the colon were located in the left upper quadrant in a circular fashion. The cecum was approximately 20 cm in length with no obvious mesentery; it was mainly located in the left lower quadrant with its end pointing towards the pelvic cavity. Therefore, we assumed that if both the entry and exit wounds were located on the right lower quadrant of the abdomen, avoiding bony structures such as right ribs, right hip and pubis, there would be injuries only to the small intestine. As predicted, in the present study, all 28 pigs were diagnosed with SBIs.
One of the greatest concerns about LIT has been its unreliability in detecting SBIs[13,14], a major reason why some surgeons still preclude LIT today. However, according to the results of the final post-mortem abdominal examination, the present study demonstrated that laparoscopy could also offer equivalent efficacy for diagnosing SBIs compared with laparotomy, with no missed injuries. According to our experience, the systematic approach for diagnostic laparoscopy exploration of the gastrointestinal tract was very important for avoiding missed SBIs[15], and mainly consisted of all the principles of open exploratory laparotomy for trauma and the technique of running the small bowel. During the exploration, we initially lifted an 8-10-cm segment of the small bowel with two 5-mm atraumatic bowel graspers at the ileocecal valve, and one side of the bowel and mesentery was observed. The graspers were then turned 180 degrees, and the other side of the bowel was visualized. This sequence was repeated until the ligament of Treitz was reached. Therefore, after using this systematic approach, we could correctly identify SBIs, minimizing the potential of a missed injury. Although diagnostic laparoscopy was time-consuming, and took approximately 45 min to diagnose intestinal injuries in each case, which was significantly longer than the laparotomy exploration, the safety and sensitivity of diagnostic laparoscopy for SBIs was good according to our research.
While surgeons disputed the disadvantages of laparoscopy for SBIs, the benefits of laparoscopy were evident[22]. First, by directly visualizing the abdominal cavity, laparoscopy allowed the surgeon to exclude the presence of other associated intra-abdominal injuries, and was also able to eliminate the blind zone of visual fields when using a 30° laparoscope. Secondly, following the laparoscopic guidance, the SBIs could be treated directly using a laparoscopic technique, or using a notably shorter incision, which was near the injuries. In the current study, five pigs in the laparosopy group were diagnosed with simple SBIs, and received total laparoscopy for treatment. In addition, video-assisted therapeutic laparoscopy, which utilized a 6-7 cm incision, was successfully carried out in nine pigs with relatively severe SBIs. Therefore, laparoscopy would also be a reliable and accurate alternative therapeutic procedure for severe SBIs[23]. Thirdly, compared with the laparotomy group, the length of incision was significantly shortened in the laparoscopy group. The length of incision is an important factor affecting surgical stress[24]. Thus, given the minimally invasive nature of laparoscopy, there is good reason to assume that laparoscopy is advantageous over conventional laparotomy in reducing surgical trauma. Another benefit of laparoscopy was the significantly reduced recovery period after surgery. The almost 50% reduction in recovery periods of bowel function, vital appearance, and food re-intake in the present research was not surprising considering the less invasive nature of the procedure. Therefore, laparoscopy could be a promising minimally invasive approach for treating SBIs[25,26].
One overwhelming limitation of this study was that a major proportion of patients with GSW to the abdomen would have significant injuries involving not only the small intestines, but also many other kinds of abdominal organs, which would make the conditions of the patients very complicated. Thus, therapeutic laparoscopy might not be the first choice for patients with GSW. However, we believe that, in the hemodynamically stable patient with abdominal penetrating injury and without extensive intra-abdominal adhesions, a thorough laparoscopic examination is possible and feasible. The results of diagnostic laparoscopy would be a useful guidance, and directly influence the modality of further treatment. Moreover, we aimed to evaluate the feasibility and validity of diagnostic and therapeutic laparoscopy for SBI, which was the chief objective of our study, and we did obtain convincing evidence supporting the use of laparoscopy for SBIs.
In conclusion, our research indicates that laparoscopy could be a minimally invasive approach for diagnosing and treating SBIs. Compared with laparotomy, laparoscopy could offer equivalent efficacy for SBIs, and reduces postoperative complications as well as recovery period.
Jian-Min Wang, Xiao-Xia Li, Liang-Chao Zhang, and Jian-Yi Kang are thanked for the skilled technical assistance when establishing the animal model (RIS, Third Military Medical University, Chongqing, China).
While laparoscopy has become a standard component of diagnosis and therapy for many conditions in general surgery, its role in abdominal trauma remains controversial. Many concerns about the safety, sensitivity, and specificity of the laparoscopy have limited its application in abdominal trauma, particularly in detecting small bowel injuries (SBIs).
One of the greatest concerns about laparoscopy in trauma (LIT) has been its unreliability in detecting SBIs, a major reason why some surgeons still preclude LIT today. This study aimed to evaluate the safety and effectiveness of diagnostic and therapeutic laparoscopy compared with laparotomy for SBIs in a porcine model.
Few studies have been carried out focusing on the value of laparoscopy for SBIs due to gunshot wounds in pigs. To the best of the authors’ knowledge, the present study was the most detailed and systematic study establishing a purely SBI porcine model. Furthermore, the study also provided a comprehensive picture of the safety and effectiveness of laparoscopy and laparotomy in trauma.
In the hemodynamically stable patient with abdominal penetrating injury, a thorough diagnostic and therapeutic laparoscopy was possible and feasible. Compared with laparotomy, laparoscopy offers equivalent efficacy for diagnosing and treating SBIs, and reduces postoperative complications as well as recovery period.
The author compared the safety and efficacy of laparoscopy for diagnosing and treating small bowel injuries in a trauma model using pigs. The study is well designed, and the article is also important and interesting.
Peer reviewers: Lygia Stewart, MD, Professor of Clinical Surgery, University of California San Francisco, 4150 Clement Street, San Francisco, CA 94121, United States; Keiji Hirata, MD, Surgery 1, University of Occupational and Environmental Health, 1-1 Iseigaoka, Yahatanishi-ku, Kitakyushu 807-8555, Japan; Dr. Olivier Detry, Department of Abdominal Surgery and Transplantation, University of Liège, CHU Sart Tilman B35, B-4000 Liège, Belgium
S- Editor Gou SX L- Editor Cant MR E- Editor Xiong L
| 1. | Nicholas JM, Rix EP, Easley KA, Feliciano DV, Cava RA, Ingram WL, Parry NG, Rozycki GS, Salomone JP, Tremblay LN. Changing patterns in the management of penetrating abdominal trauma: the more things change, the more they stay the same. J Trauma. 2003;55:1095-108; discussion 1108-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Watts DD, Fakhry SM. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. J Trauma. 2003;54:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 197] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Busić Z, Lovrić Z, Amić E, Busić D, Lovrić L. Small bowel injuries in penetrating abdominal trauma during war: ten-year follow-up findings. Mil Med. 2004;169:721-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Lee WC, Uddo JF, Nance FC. Surgical judgment in the management of abdominal stab wounds. Utilizing clinical criteria from a 10-year experience. Ann Surg. 1984;199:549-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Ertekin C, Yanar H, Taviloglu K, Güloglu R, Alimoglu O. Unnecessary laparotomy by using physical examination and different diagnostic modalities for penetrating abdominal stab wounds. Emerg Med J. 2005;22:790-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma. 1995;38:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 216] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 8. | Lin HF, Wu JM, Tu CC, Chen HA, Shih HC. Value of diagnostic and therapeutic laparoscopy for abdominal stab wounds. World J Surg. 2010;34:1653-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Leppäniemi A, Haapiainen R. Diagnostic laparoscopy in abdominal stab wounds: a prospective, randomized study. J Trauma. 2003;55:636-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 89] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Elliott DC, Rodriguez A, Moncure M, Myers RA, Shillinglaw W, Davis F, Goldberg A, Mitchell K, McRitchie D. The accuracy of diagnostic laparoscopy in trauma patients: a prospective, controlled study. Int Surg. 1998;83:294-298. [PubMed] |
| 11. | Simon RJ, Rabin J, Kuhls D. Impact of increased use of laparoscopy on negative laparotomy rates after penetrating trauma. J Trauma. 2002;53:297-302; discussion 302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Villavicencio RT, Aucar JA. Analysis of laparoscopy in trauma. J Am Coll Surg. 1999;189:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 90] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Streck CJ, Lobe TE, Pietsch JB, Lovvorn HN. Laparoscopic repair of traumatic bowel injury in children. J Pediatr Surg. 2006;41:1864-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Mathonnet M, Peyrou P, Gainant A, Bouvier S, Cubertafond P. Role of laparoscopy in blunt perforations of the small bowel. Surg Endosc. 2003;17:641-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Kawahara NT, Alster C, Fujimura I, Poggetti RS, Birolini D. Standard examination system for laparoscopy in penetrating abdominal trauma. J Trauma. 2009;67:589-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Ivatury RR, Simon RJ, Stahl WM. A critical evaluation of laparoscopy in penetrating abdominal trauma. J Trauma. 1993;34:822-87; discussion 822-87;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 186] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Becker HP, Willms A, Schwab R. [Laparoscopy for abdominal trauma]. Chirurg. 2006;77:1007-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, Ivatury RR, Scalea TM. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010;68:721-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 174] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 19. | Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, McAninch JW, Pachter HL, Shackford SR, Trafton PG. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma. 1990;30:1427-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 446] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 20. | Olofsson P, Vikström T, Nagelkerke N, Wang J, Abu-Zidan FM. Multiple small bowel ligation compared to conventional primary repair after abdominal gunshot wound with haemorrhagic shock. Scand J Surg. 2009;98:41-47. [PubMed] |
| 21. | Wang P, Wang J, Zhang W, Li Y, Li J. Effect of the combination of fibrin glue and growth hormone on intestinal anastomoses in a pig model of traumatic shock associated with peritonitis. World J Surg. 2009;33:567-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Barzana DC, Kotwall CA, Clancy TV, Hope WW. Use of laparoscopy in trauma at a level II trauma center. JSLS. 2011;15:179-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Kaban GK, Novitsky YW, Perugini RA, Haveran L, Czerniach D, Kelly JJ, Litwin DE. Use of laparoscopy in evaluation and treatment of penetrating and blunt abdominal injuries. Surg Innov. 2008;15:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Ishibashi S, Takeuchi H, Fujii K, Shiraishi N, Adachi Y, Kitano S. Length of laparotomy incision and surgical stress assessed by serum IL-6 level. Injury. 2006;37:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Addeo P, Calabrese DP. Diagnostic and therapeutic value of laparoscopy for small bowel blunt injuries: A case report. Int J Surg Case Rep. 2011;2:316-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Chol YB, Lim KS. Therapeutic laparoscopy for abdominal trauma. Surg Endosc. 2003;17:421-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 86] [Article Influence: 3.9] [Reference Citation Analysis (0)] |