Published online Sep 21, 2012. doi: 10.3748/wjg.v18.i35.4905
Revised: April 24, 2012
Accepted: April 27, 2012
Published online: September 21, 2012
AIM: To assess the diagnostic performance of follow-up liver computed tomography (CT) for the detection of high-risk esophageal varices in patients treated with locoregional therapy for hepatocellular carcinoma (HCC).
METHODS: We prospectively enrolled 100 patients with cirrhosis who underwent transcatheter arterial chemoembolization, radiofrequency ablation or both procedures for HCCs. All patients underwent upper endoscopy and subsequently liver CT. Three radiologists independently evaluated the presence of high-risk esophageal varices with transverse images alone and with three orthogonal multiplanar reformation (MPR) images, respectively. With endoscopic grading as the reference standard, diagnostic performance was assessed by using receiver operating characteristic (ROC) curve analysis.
RESULTS: The diagnostic performances (areas under the ROC curve) of three observers with transverse images alone were 0.947 ± 0.031, 0.969 ± 0.024, and 0.916 ± 0.038, respectively. The mean sensitivity, specificity, positive predicative value (PPV), and negative predicative value (NPV) with transverse images alone were 90.1%, 86.39%, 70.9%, and 95.9%, respectively. The diagnostic performances, mean sensitivity, specificity, PPV, and NPV with three orthogonal MPR images (0.965 ± 0.025, 0.959 ± 0.027, 0.938 ± 0.033, 91.4%, 89.5%, 76.3%, and 96.6%, respectively) were not superior to corresponding values with transverse images alone (P > 0.05), except for the mean specificity (P = 0.039).
CONCLUSION: Our results showed excellent diagnostic performance, sensitivity and NPV to detect high-risk esophageal varices on follow-up liver CT after locoregional therapy for HCC.
- Citation: Kim H, Choi D, Lee JH, Lee SJ, Jo H, Gwak GY, Koh KC, Choi MS, Kim S. High-risk esophageal varices in patients treated with locoregional therapy for hepatocellular carcinoma: Assessment with liver computed tomography. World J Gastroenterol 2012; 18(35): 4905-4911
- URL: https://www.wjgnet.com/1007-9327/full/v18/i35/4905.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i35.4905
More than one-half of patients with cirrhosis eventually develop esophageal varices[1]. Screening upper endoscopy is repeated in 1-3 years in order to evaluate esophageal varices in cirrhotic patients owing to the substantial morbidity and mortality related with variceal bleeding[2]. The presence of high-risk varices seen in up to 30% of patients with esophageal varices on endoscopy is considered as an indication for prophylaxis against variceal bleeding with either endoscopic variceal ligation (EVL) or the administration of β-blockers[1,3].
Of several recent studies that have suggested the usefulness of computed tomography (CT) scans to evaluate esophageal varices[4-8], one study[7] asserted that CT was a better initial screening modality when compared to endoscopy in terms of cost-effectiveness and patient preference. However, for only these reasons, the adoption of CT to replace ultrasound as the surveillance imaging technique in all cirrhotic patients is still subject to debate with the consideration of radiation hazards[9]. As CT is commonly used as a follow-up imaging modality in patients treated with locoregional therapy for hepatocellular carcinoma (HCC)[10], we supposed that replacement of CT for evaluating varices was more persuasive in such patients. The purpose of this study was to evaluate prospectively the diagnostic performance of radiologists for the detection of high-risk esophageal varices on regular follow-up liver multi-detector row computed tomography (MDCT) examinations in patients treated with locoregional therapy for HCC. We also assessed the usefulness of the addition of coronal and sagittal multiplanar reformation (MPR) images.
The Institutional Review Board approved the current study and all subjects provided informed consent. In this prospective study, the sample size was determined for overall diagnostic performance based on the area (Az) under the composite receiver operating characteristic (ROC) curve using pooled data of all observers. We expected that the pooled Az for the diagnosis of high-risk varices on CT is 0.95, with a width of the 95% confidence interval (CI) of 0.05. When the ratio of the number of patients with high-risk varices ranges from 1:1 to 1:6 and the ratio of standard deviation of pooled Az with high-risk varices ranges from 1:1 to 3:1, the standard error of estimates of Az in 100 subjects is ≤ 0.025. Thus, the 95%CI of Az is ≤ 0.05[11].
From June 2009 to December 2010, we enrolled patients with cirrhosis as well as HCCs treated with transcatheter arterial chemoembolization (TACE), radiofrequency (RF) ablation or both procedures who were scheduled to undergo both a regular follow-up liver CT examination and a screening upper endoscopy. We excluded patients who had a history of undergoing EVL for esophageal varices[5]. One-hundred patients who agreed to participate in our prospective study underwent an endoscopy and a subsequent liver MDCT examination within four hours after endoscopy. All patients had undergone one or more regular (all within a 6-mo interval) follow-up liver MDCT examinations following TACE (n = 43), RF ablation (n = 35) or both procedures (n = 22) for HCCs. The patient population consisted of 79 men and 21 women (age range, 35-82 years; median age, 59 years, mean age, 58.4 years). Patients were diagnosed with cirrhosis based on liver histopathology (n = 28), or characteristic clinical features (symptoms and stigmata of cirrhosis and its complications), laboratory results (levels of viral markers, hyperbilirubinemia, hypoalbuminemia and coagulopathy), or imaging findings (liver configuration, splenomegaly, ascites and collateral vessels) (n = 72). Eighteen patients received β-blocker medication. All patients had liver cirrhosis due to hepatitis B infection (n = 76), hepatitis C infection (n = 14), alcohol use (n = 5) or an unknown etiology (n = 5). There were 89 patients with Child-Pugh class A, ten patients with Child-Pugh class B, and one patient with Child-Pugh class C disease.
Patients underwent standard upper endoscopy performed by experienced gastroenterologists (with experience of performing more than 500 endoscopy examinations) in our endoscopy unit. Seven gastroenterologists performed endoscopy of the 100 patients in our study. All endoscopic studies were captured as digital imaging files. On endoscopy, esophageal varices were graded according to criteria proposed by the Japanese Research Society for Portal Hypertension[12]. Grade 2 (varices showing a beaded appearance) or grade 3 (varices running in an oblique course and showing tortuosity with a tumorfactive appearance) was chosen as a cutoff point to define high-risk varices, based on the possibility to develop esophageal bleeding[12]. Two specialized endoscopists (Joon Hyeok Lee and Moon Seok Choi) reviewed all of the stored endoscopic images and the procedure reports for all patients. The endoscopists determined the final grades of the esophageal varices of the study population based on consensus. Disagreement between the two endoscopists was resolved in conference along with a third endoscopist (Geum-Youn Gwak).
Liver CT examinations for follow-up were performed with a 64-slice MDCT scanner (Lightspeed VCT; GE Healthcare, Milwaukee, WI, United States). A total of 120 mL of nonionic contrast material (Ultravist 300, 300 mg/mL iopromide, Schering, Berlin, Germany) was administered intravenously with an automatic injector at a rate of 3-4 mL/s. Images were obtained at 30-40 s, 70 s and 180 s after the initiation of contrast material injection, representing the hepatic arterial, portal venous and equilibrium phases, respectively. In order to determine the appropriate scanning time for hepatic arterial phase imaging, we used an automatic bolus-tracking technique with automated scan-triggering software (SmartPrep; GE Healthcare). Hepatic arterial phase scanning was started automatically 12 s after the trigger threshold (100 HU) was reached at the level of the supraceliac abdominal aorta. Images were obtained from the dome of the diaphragm to the bottom of the liver during a single breath-hold. CT scanning parameters were as follows: 64 detector rows; beam collimation, 0.625 mm × 64 mm; pitch, 0.984; kVp/mA, 120/100-300; gantry rotation time, 0.6 s. Isotropic raw data were acquired with a slice thickness of 1.25 mm and an interval of 1.25 mm with the use of MDCT. Using the raw data, a transverse image was obtained with a slice thickness of 5 mm and an interval of 2.5 mm. During the portal venous phase, coronal and sagittal MPR images were obtained with a 3 mm interval and a slice thickness of 3 mm. No patients received oral contrast material.
Three abdominal radiologists (Soon Jin Lee, Dongil Choi and Hangi Jo) independently interpreted the liver CT images in order to detect the presence of high-risk (grade 2 or 3) esophageal varices. The radiologists had 13, nine and five years experience, respectively, in the interpretation of abdominal CT images. The radiologists initially evaluated transverse images alone in a random order on a picture archiving and communication system (PACS) monitor. After three weeks, three orthogonal MPR images were assessed in another random order. The radiologists were blinded to the patient physical findings, laboratory values, previous imaging results and endoscopy results.
The CT images were reviewed to detect the presence of high-risk esophageal varices with a 4-point confidence scale for the development of variceal bleeding based on the endoscopic findings that were correlated with variceal bleeding: (1) definitely low-risk or no varices; (2) probably low-risk; (3) probably high-risk; and (4) definitely high-risk. The observers investigated beaded and tortuous varices (distinct enhancing nodular or linear lesions that abutted the surface of the esophageal lumen or protruded into the luminal space) on stack PACS images of CT scans. In addition, the observers measured the shortest diameter of the largest enhancing lesion (varix) during the portal venous phase by the use of an electronic caliper on one-format PACS images. A confidence score of 4 could be assigned if the diameter was definitely greater than 3 mm. A score of 3 was assigned if the diameter was between 2 mm to 3 mm. A score of 2 was assigned if the diameter was between 1 mm to 2 mm. A score of 1 was assigned if the diameter was less than 1 mm[4].
The results of liver CT imaging analyzed by three observers were correlated with the endoscopic grading of esophageal varices by the study coordinator (Hyojin Kim). Observer performance for the detection of high-risk esophageal varices was assessed by the use of ROC curve analysis with transverse images alone and with three orthogonal MPR images. Az under each ROC curve by application of the maximum-likelihood curve-fitting algorithm was used to indicate the diagnostic performance for the detection of high-risk esophageal varices on liver CT images. Az values were compared by using pseudovalues with the jackknife method developed by Dorfman et al[13]. Composite ROC curves for the performance of all observers were obtained by using the pooled data of the three observers.
The sensitivity and specificity for the CT diagnosis of high-risk esophageal varices were calculated. The sensitivity for the detection of varices was determined by use of the number of patients with varices assigned a score of 3 or 4. Sensitivities and specificities for transverse images alone and three orthogonal MPR images were compared with use of the McNemar test. The positive predicative value (PPV) and negative predicative value (NPV) were also calculated and compared with use of the χ2 test and Fisher’s exact test, respectively. A P value of less than 0.05 was considered as significant.
Interobserver agreements for the detection of esophageal varices and high-risk varices were evaluated using κ statistics. The degree of agreement was categorized as follows: κ values of 0.00-0.20 were considered to indicate poor agreement; κ values of 0.21-0.40, fair agreement; κ values of 0.41-0.60, moderate agreement; κ values of 0.61-0.80, good agreement; κ values of 0.81-1.00, excellent agreement[14]. Statistical analyses were performed using commercially available software packages (PASW Statistics, release 17.0.2; SPSS, Chicago, IL, United States; MedCalc, version 7.1; MedCalc Software, Mariakerke, Belgium).
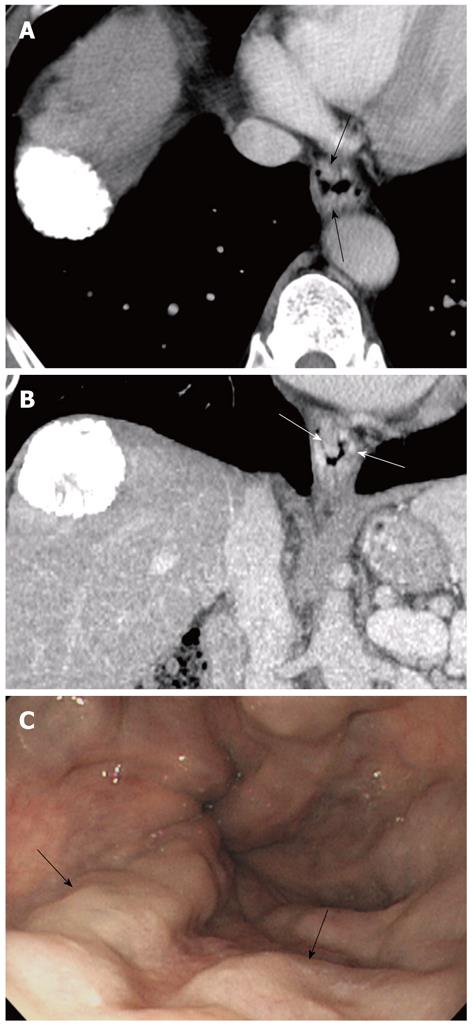
In 50 patients, there were no esophageal varices (grade 0) as determined by endoscopy. Twenty-three patients were classified with grade 1 esophageal varices, 24 patients were classified with grade 2 esophageal varices (Figure 1), and three patients were classified with grade 3 esophageal varices. No patients had a significant endoscopic abnormality other than esophageal varices, such as an ulcer, inflammation or mass. The red sign was observed in one (4.3%) of 23 patients with a grade 1 varix, 15 (62.5%) of 24 patients with a grade 2 varix and two (66.7%) of three patients with a grade 3 varix.
The Az values of the ROC assessment of the three observers for the detection of high-risk esophageal varices with transverse images alone were 0.947 ± 0.031 (95%CI, 0.883-0.982), 0.969 ± 0.024 (95%CI, 0.913-0.993) and 0.916 ± 0.038 (95%CI, 0.843-0.962), respectively. The Az values of the ROC assessment of the three observers with the three orthogonal MPR images were 0.965 ± 0.025 (95%CI, 0.908-0.991), 0.959 ± 0.027 (95%CI, 0.899-0.988) and 0.938 ± 0.033 (95%CI, 0.871-0.976), respectively. The Az values of each observer were similar for transverse images alone and for the three orthogonal MPR images (each P > 0.05) (Table 1). In addition, there was no significant difference of mean Az values of pooled data by the three observer for transverse images alone (0.946 ± 0.018; 95%CI, 0.914-0.968) and for the three orthogonal MPR images (0.954 ± 0.017; 95%CI, 0.924-0.975, P > 0.05). The Az values were also similar among the three observers both for transverse images alone and for the three orthogonal MPR images, respectively (each P > 0.05) (Table 1).
| Observer 1 | Observer 1 | Observer 2 | Observer 2 | Observer 3 | Observer 3 | Mean | Mean | |
| Transverse | 3 MPR | Transverse | 3 MPR | Transverse | 3 MPR | Transverse | 3 MPR | |
| ROC Az | 0.947 ± 0.031 | 0.965 ± 0.025 | 0.969 ± 0.024 | 0.959 ± 0.027 | 0.916 ± 0.038 | 0.938 ± 0.033 | 0.946 ± 0.018 | 0.954 ± 0.017 |
| 95%CI | 0.883-0.982 | 0.908-0.991 | 0.913-0.993 | 0.899-0.988 | 0.843-0.962 | 0.871-0.976 | 0.914-0.968 | 0.924-0.975 |
| P value1 | 0.318 | 0.328 | 0.271 | 0.367 | ||||
| P value2 | Observer 1-2 | Observer 1-2 | Observer 2-3 | Observer 2-3 | Observer 3-1 | Observer 3-1 | ||
| 0.368 | 0.782 | 0.099 | 0.461 | 0.35 | 0.334 |
The mean sensitivity for the detection of high-risk esophageal varices of the three observers with transverse images alone and with the three orthogonal MPR images were 90.1% and 91.4%, respectively (P > 0.05). For each observer, the sensitivities of detecting high-risk esophageal varices were also similar for transverse images alone and for the three orthogonal MPR images (each P > 0.05) (Table 2). While the specificities of each observer were similar for transverse images alone and for the three orthogonal MPR images (each P > 0.05), the mean specificity with the three orthogonal MPR images (89.5%) was better than that with transverse images alone (86.3%) (P = 0.039) (Table 2).
| Observer 1 | Observer 1 | Observer 2 | Observer 2 | Observer 3 | Observer 3 | Mean | Mean | |
| Transverse | 3 MPR | Transverse | 3 MPR | Transverse | 3 MPR | Transverse | 3 MPR | |
| Sensitivity% | 92.6 (25/27) | 92.6 (25/27) | 92.6 (25/27) | 92.6 (25/27) | 85.2 (23/27) | 88.9 (24/27) | 90.1 (73/81) | 91.4 (74/81) |
| P value | 1.000 | 1.000 | 1.000 | 1.000 | ||||
| Specificity% | 89.0 (65/73) | 90.4 (66/73) | 87.7 (64/73) | 87.7 (64/73) | 82.2 (60/73) | 90.4 (66/73) | 86.3 (189/219) | 89.5 (196/219) |
| P value | 1.000 | 1.000 | 0.070 | 0.039 |
There was no significant difference for the mean PPV of three observers for transverse images alone (70.9%) and for the three orthogonal MPR images (76.3%, P > 0.05). For each observer, the PPVs were also similar for transverse images alone and for the three orthogonal MPR images (each P > 0.05) (Table 3). There was no significant difference of the mean NPV for transverse images alone (95.9%) and for the three orthogonal MPR images (96.6%, P > 0.05). For each observer, the NPVs were also similar for transverse images alone and for the three orthogonal MPR images (each P > 0.05) (Table 3).
| Observer 1 | Observer 1 | Observer 2 | Observer 2 | Observer 3 | Observer 3 | All | All | |
| Transverse | 3 MPR | Transverse | 3 MPR | Transverse | 3 MPR | Transverse | 3 MPR | |
| PPV % | 75.8 (25/33) | 78.1 (25/32) | 73.5 (25/34) | 73.5 (25/34) | 63.9 (23/36) | 77.4 (24/31) | 70.9 (73/103) | 76.3 (74/97) |
| P value | 0.947 | 1.000 | 0.352 | 0.482 | ||||
| NPV% | 97.0 (65/67) | 97.1 (66/68) | 97.0 (64/66) | 97.0 (64/66) | 93.8 (60/64) | 95.7 (66/69) | 95.9 (189/197) | 96.6 (196/203) |
| P value | 1.000 | 1.000 | 0.710 | 0.797 |
All κ values for agreements among the three observers with transverse images alone showed excellent agreements (range: 0.845-0.933), and κ values for agreements among three observers with three orthogonal MPR images demonstrated good and excellent agreements (range: 0.791-0.910).
Although liver CT images always cover the distal esophagus where all varices occur, some radiologists do not comment on either the presence or the degree of esophageal varices in radiological reports. Some endoscopists are unaware that liver CT scans provide excellent images of esophageal varices. Regular follow-up CT examinations are essential to evaluate recurrence and therapeutic effectiveness in patients treated with TACE or ablation therapy for HCC[10,15]. In such patients, we can make an objective decision about the risk of variceal bleeding with the use of regular follow-up CT imaging without the use of an invasive endoscopic evaluation. The presence of periesophageal varices has been correlated with recurrence of luminal esophageal varices after treatment[16].
As with the results of previous reports[4-8], the sensitivities for the detection of high-risk esophageal varices for each observer were also high (approximately 90%) in our study (Table 2). Excellent NPVs as well as high sensitivities for the detection of high-risk varices are clinically important, as the goal of endoscopic screening for esophageal varices is to decrease morbidity and mortality resulting from variceal bleeding. As good screening tests should show a low frequency of false negative results, sensitivity and NPV are more important as compared to specificity and PPV in a screening test[17]. Even though both PPV and NPV are influenced by disease prevalence, the prevalence of high-risk esophageal varices in our study was similar to prior studies[4-8].
A recent study[7] mentioned the possibility that sagittal and coronal images with isotropic spacial resolution potentially decrease measurement variability as vessels are displayed within the imaging plane. However, based on the results of our study, additional coronal and sagittal images showed little practical help to evaluate high-risk esophageal varices when compared to assessment of transverse images alone. Moreover, the use of virtual esophagography proposed in another recent study[5] might be impractical because of time-consuming and invasive insertion of the esophagus with a catheter for air insufflation. Insufflation alters both the luminal pressure and the hemodynamics of the varices. Perri et al[7] pointed out that the measurement of varices in a non-distended state might provide a more proper assessment for bleeding risk as variceal bleeding occurs while the esophagus is in its normal non-distended state.
Our study has some limitations. The most important limitation is the use of endoscopy as the reference standard. Prior studies[18,19] have demonstrated a lack of good correlation between endoscopists to evaluate the grades of esophageal varices. In our study, given the semi-open access system of the endoscopy unit, many different endoscopists perform endoscopy procedures. Hence, specialized endoscopists re-evaluated the grades of esophageal varices with review of the stored endoscopic images. Second, we could not evaluate qualitative endoscopic appearances including the presence of red signs such as cherry-red spots and diffuse redness, which is one of the predictors of variceal bleeding. These red signs cannot be depicted on CT images. In a recent report[20], cases with the shortest diameter of the largest varix of more than 4 mm showed positive red signs. In our study, the endoscopic red sign was observed in only one patient with low-risk (grade 1) esophageal varices (4.3%, 1 of 23 cases)[4].
In conclusion, our results have demonstrated excellent diagnostic performance, sensitivity and NPV with low interobserver variability to detect high-risk esophageal varices on regular follow-up liver MDCT examinations in patients treated with locoregional therapy for HCCs. Careful evaluation of high-risk esophageal varices on a liver MDCT examination may be useful to avoid performing low-yield endoscopy in such patients. When compared to the assessment of transverse images alone, additional coronal and sagittal images were of little help to evaluate high-risk esophageal varices. Our results suggest that liver CT can be used as a single noninvasive surveillance tool for both esophageal varices and recurrent HCC after locoregional therapy. However, a definite change of clinical pathways may be needed in a randomized controlled study on the comparison of bleeding frequency and survival in patients treated with locoregional therapy between the use of a regular follow-up liver MDCT examination alone and with the combination of screening endoscopy.
The presence of high-risk varices seen in up to 30% of patients with esophageal varices on endoscopy is considered as an indication for prophylaxis against variceal bleeding with either endoscopic variceal ligation or the administration of β-blockers. Several recent studies have suggested the usefulness of computed tomography (CT) scans to evaluate esophageal varices, and one study asserted that CT was a better initial screening modality when compared to endoscopy in terms of cost-effectiveness and patient preference.
As CT is commonly used as a follow-up imaging modality in patients treated with locoregional therapy for hepatocellular carcinoma (HCC), the authors suggested that replacement of CT for evaluating varices was more persuasive in such patients. Careful evaluation of high-risk esophageal varices on a liver multi-detector row computed tomography (MDCT) examination may be useful to avoid performing low-yield endoscopy in such patients.
The results of this study have demonstrated excellent diagnostic performance, sensitivity and negative predicative value with low interobserver variability to detect high-risk esophageal varices on regular follow-up liver MDCT examinations in patients treated with locoregional therapy for HCCs. When compared to the assessment of transverse images alone, additional coronal and sagittal images were of little help to evaluate high-risk esophageal varices.
The study results suggest that that liver CT can be used as a single noninvasive surveillance tool for both esophageal varices and recurrent HCC after locoregional therapy.
This is a good prospective study in which authors evaluate the diagnostic performance of radiologists for the detection of high-risk esophageal varices on regular follow-up liver multi-detector row CT examinations in patients treated with locoregional therapy for HCC.
Peer reviewers: Eric R Kallwitz, Assistant Professor, University of Illinois, 840 S Wood Street, Chicago, IL 60612, United States; Hyo-Cheol Kim, Professor, Seoul National University Hospital, 28 Yongon-dong, Chongno-gu, Seoul 110-744, South Korea
S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | D'Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19:475-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 600] [Cited by in RCA: 484] [Article Influence: 18.6] [Reference Citation Analysis (1)] |
| 2. | Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001;120:726-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 284] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 3. | De BK, Ghoshal UC, Das T, Santra A, Biswas PK. Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleed: preliminary report of a randomized controlled trial. J Gastroenterol Hepatol. 1999;14:220-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Kim H, Choi D, Gwak GY, Lee JH, Park MK, Lee HIe, Kim SH, Nam S, Yoo EY, Do YS. Evaluation of esophageal varices on liver computed tomography: receiver operating characteristic analyses of the performance of radiologists and endoscopists. J Gastroenterol Hepatol. 2009;24:1534-1540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Kim SH, Kim YJ, Lee JM, Choi KD, Chung YJ, Han JK, Lee JY, Lee MW, Han CJ, Choi JI. Esophageal varices in patients with cirrhosis: multidetector CT esophagography--comparison with endoscopy. Radiology. 2007;242:759-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Kim YJ, Raman SS, Yu NC, To'o KJ, Jutabha R, Lu DS. Esophageal varices in cirrhotic patients: evaluation with liver CT. AJR Am J Roentgenol. 2007;188:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Perri RE, Chiorean MV, Fidler JL, Fletcher JG, Talwalkar JA, Stadheim L, Shah ND, Kamath PS. A prospective evaluation of computerized tomographic (CT) scanning as a screening modality for esophageal varices. Hepatology. 2008;47:1587-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Kim H, Choi D, Gwak GY, Lee JH, Lee SJ, Kim SH, Lee JY, Park Y, Chang I, Lim HK. High-risk esophageal varices in patients treated with locoregional therapies for hepatocellular carcinoma: evaluation with regular follow-up liver CT. Dig Dis Sci. 2009;54:2247-2252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4333] [Cited by in RCA: 4507] [Article Influence: 225.4] [Reference Citation Analysis (0)] |
| 10. | Lim HK, Choi D, Lee WJ, Kim SH, Lee SJ, Jang HJ, Lee JH, Lim JH, Choo IW. Hepatocellular carcinoma treated with percutaneous radio-frequency ablation: evaluation with follow-up multiphase helical CT. Radiology. 2001;221:447-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 173] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 11. | Obuchowski NA. Computing sample size for receiver operating characteristic studies. Invest Radiol. 1994;29:238-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Idezuki Y. General rules for recording endoscopic findings of esophagogastric varices (1991). Japanese Society for Portal Hypertension. World J Surg. 1995;19:420-422; discussion 423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 141] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Dorfman DD, Berbaum KS, Metz CE. Receiver operating characteristic rating analysis. Generalization to the population of readers and patients with the jackknife method. Invest Radiol. 1992;27:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 614] [Cited by in RCA: 573] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 14. | Fleiss JL. The measurment of interrater agreement. Statistical methods for rates and proportions. New York: John Wiley and Sons 1981; 212-236. |
| 15. | Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD, Dupuy DE, Gervais D, Gillams AR, Kane RA, Lee FT. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005;235:728-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 522] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 16. | Irisawa A, Saito A, Obara K, Shibukawa G, Takagi T, Shishido H, Sakamoto H, Sato Y, Kasukawa R. Endoscopic recurrence of esophageal varices is associated with the specific EUS abnormalities: severe periesophageal collateral veins and large perforating veins. Gastrointest Endosc. 2001;53:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Dawson-Saunders B, Trapp RG. Evaluating diagnostic procedures. Basic and clinical biostatistics. 2nd ed. Tokyo: Prentice-Hall International Inc 1994; 232-249. |
| 18. | Calès P, Oberti F, Bernard-Chabert B, Payen JL. Evaluation of Baveno recommendations for grading esophageal varices. J Hepatol. 2003;39:657-659. [PubMed] |
| 19. | Bendtsen F, Skovgaard LT, Sørensen TI, Matzen P. Agreement among multiple observers on endoscopic diagnosis of esophageal varices before bleeding. Hepatology. 1990;11:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Mifune H, Akaki S, Ida K, Sei T, Kanazawa S, Okada H. Evaluation of esophageal varices by multidetector-row CT: correlation with endoscopic 'red color sign'. Acta Med Okayama. 2007;61:247-254. [PubMed] |