Published online Sep 7, 2012. doi: 10.3748/wjg.v18.i33.4585
Revised: February 10, 2012
Accepted: March 10, 2012
Published online: September 7, 2012
AIM: To determine the value of bowel sounds analysis using an electronic stethoscope to support a clinical diagnosis of intestinal obstruction.
METHODS: Subjects were patients who presented with a diagnosis of possible intestinal obstruction based on symptoms, signs, and radiological findings. A 3M™ Littmann® Model 4100 electronic stethoscope was used in this study. With the patients lying supine, six 8-second recordings of bowel sounds were taken from each patient from the lower abdomen. The recordings were analysed for sound duration, sound-to-sound interval, dominant frequency, and peak frequency. Clinical and radiological data were reviewed and the patients were classified as having either acute, subacute, or no bowel obstruction. Comparison of bowel sound characteristics was made between these subgroups of patients. In the presence of an obstruction, the site of obstruction was identified and bowel calibre was also measured to correlate with bowel sounds.
RESULTS: A total of 71 patients were studied during the period July 2009 to January 2011. Forty patients had acute bowel obstruction (27 small bowel obstruction and 13 large bowel obstruction), 11 had subacute bowel obstruction (eight in the small bowel and three in large bowel) and 20 had no bowel obstruction (diagnoses of other conditions were made). Twenty-five patients received surgical intervention (35.2%) during the same admission for acute abdominal conditions. A total of 426 recordings were made and 420 recordings were used for analysis. There was no significant difference in sound-to-sound interval, dominant frequency, and peak frequency among patients with acute bowel obstruction, subacute bowel obstruction, and no bowel obstruction. In acute large bowel obstruction, the sound duration was significantly longer (median 0.81 s vs 0.55 s, P = 0.021) and the dominant frequency was significantly higher (median 440 Hz vs 288 Hz, P = 0.003) when compared to acute small bowel obstruction. No significant difference was seen between acute large bowel obstruction and large bowel pseudo-obstruction. For patients with small bowel obstruction, the sound-to-sound interval was significantly longer in those who subsequently underwent surgery compared with those treated non-operatively (median 1.29 s vs 0.63 s, P < 0.001). There was no correlation between bowel calibre and bowel sound characteristics in both acute small bowel obstruction and acute large bowel obstruction.
CONCLUSION: Auscultation of bowel sounds is non-specific for diagnosing bowel obstruction. Differences in sound characteristics between large bowel and small bowel obstruction may help determine the likely site of obstruction.
- Citation: Ching SS, Tan YK. Spectral analysis of bowel sounds in intestinal obstruction using an electronic stethoscope. World J Gastroenterol 2012; 18(33): 4585-4592
- URL: https://www.wjgnet.com/1007-9327/full/v18/i33/4585.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i33.4585
Auscultation of bowel sounds is a traditional technique for evaluating patients with abdominal symptoms. It is simple, but generally empirical and too subjective. Bowel sounds show wide variations from person to person and even from the same person at different times. The interpretation of a person’s bowel sounds by different clinicians may also vary[1,2]. There is a distinct lack of clinical research within the literature to support any discussion on the value of auscultation for bowel sounds[3]. Many practitioners pay little attention to this physical examination and some have even abandoned their stethoscope. The question has been raised as to whether auscultation for bowel sounds is of any clinical value.
Recently, recording of bowel sounds with objective evaluation has become possible with commercially available electronic stethoscopes; however, bowel sounds in intestinal obstruction have not been extensively studied since the introduction of these stethoscopes.
The aim of this study is to determine the value of objective assessment of bowel sounds provided by an electronic stethoscope in supporting a clinical diagnosis of intestinal obstruction. Correlation with radiological and operative findings and clinical outcome is made to identify characteristic bowel sounds that will improve the diagnostic accuracy for bowel obstruction.
The electronic stethoscope used for this study was the 3M™ Littmann® Model 4100 with Version 2.0 sound analysis software (3M Health Care, St. Paul, MN 55144, United States). Three frequency modes are available for auscultation: bell (20-200 Hz), diaphragm (100-500 Hz), and extended range (20-1000 Hz). Bowel sounds are best heard in the diaphragm mode, which selectively filters in sounds of higher frequency range, thus omitting the low frequency sounds transmitted from the heart or lungs. Other features of the electronic stethoscope include the ability to amplify sounds several times compared with a conventional stethoscope, and digital signal processing over the entire acoustic range. A maximum of six distinct tracks of up to 8 s each can be recorded and stored in the stethoscope. The recorded sound tracks are then transmitted to a computer via an infrared link.
The Local Ethics Committee approved this study. The subjects were patients admitted to our institution with a diagnosis of possible intestinal obstruction during the period July 2009 to January 2011. Clinical data were prospectively collected. The presenting complaints and findings from physical examination were reviewed following admission to the ward. Verbal consent was obtained from the patients for recording of their bowel sounds. The patients were positioned lying supine on a bed. Six 8-s recordings were taken from each patient with the stethoscope positioned on the lower abdomen (two at the right iliac fossa, two at the suprapubic region, and two at the left iliac fossa). The reason for recording sounds from the three different areas of the lower abdomen was to position the stethoscope as far away from the heart and lungs as possible to reduce the interference by sounds arising from the heart and lungs. For the purpose of this study, no attempt was made to compare the sounds at different recording sites as a previous study showed that the frequency and intensity of bowel sounds were equal throughout all four quadrants[4]. The diagnosis of each of the patients was determined by clinical follow-up, clinical evolution, and by radiological and operative findings. The recorded sound tracks were analysed by the main investigator using the supplied software. The investigators were not blinded to the results of other tests such as radiological imaging or intra-operative findings.
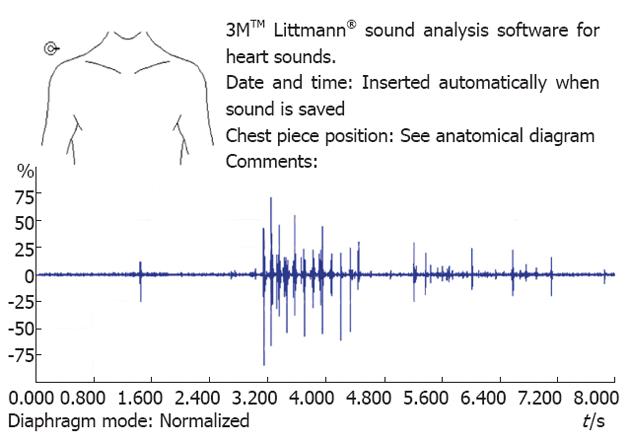
When analyzing the sound tracks, the tracks were played back in the “diaphragm” mode. The overall quality of recording was determined by the level of ambient background noise that was actually present at the time of recording, and the presence of a constant “hissing” machinery noise (not present in the environment during recording), which could sometimes occur during playback of some of the tracks. This “ghost sound” phenomenon was noticeably more common when the entire track lacked actual bowel sounds and it was thought that the recording system compensates for the lack of sound by automatic over-amplification of the baseline machine noise. The waveform view displays the raw input signal as a continuous waveform line, where each wave is a pulse of sound. The maximum arbitrary amplitude (range 0% to 100%) of the bowel sounds was identified from each track (Figure 1).
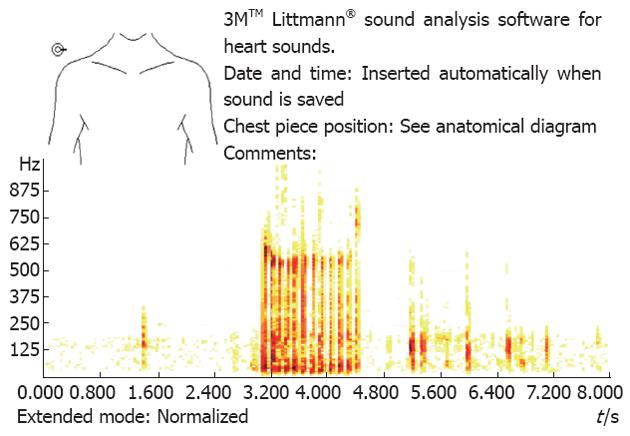
The sounds were described as “isolated” when they occurred in isolation and did not last for more than 0.5 s in duration and were more than 0.2 s apart. The spike of the isolated sound is shown as a single vertical line over a very short duration (Figure 1). The sounds were described as “clustered” when they occurred continuously for more than 0.5 s and recognised audibly as a run of individual “popping” effects (Figure 1), and “prolonged” when they occurred continuously for longer than 4 s[5]. The interval between sounds was determined by the period between the end of one sound and the start of the next sound. For the purpose of computation, when there were more than two distinct bowel sounds on a single track the shortest interval between two distinct bowel sounds was taken as the interval between sounds for that track. The spectrum view displays the frequency distribution as vertical bars, each bar represents a group of frequencies, and the more prominent frequencies have darker colour tones than the less prominent frequencies (Figure 2). The highest dominant frequency from each track was determined by first identifying the most dominant sound frequency across the spectrum at each point of time when bowel sounds were present. The highest dominant frequency over the entire duration of the track was then identified and used for analysis. The peak frequency was determined by the highest value dominant frequency among the six tracks for each individual patient.
X-rays and computed tomography (CT) imaging of the abdomen and pelvis were reviewed for evidence of intestinal distension. The calibre of the small bowel and large bowel at the widest points were determined using the measuring tool in the Amalga IMS 5.1 radiology image viewing system installed on our institution’s computers. The point of transition was identified if bowel obstruction was present on CT images. Any operative intervention performed for the patients was also documented. The cause of obstruction, as identified from radiological imaging and/or during surgery, was recorded.
The following definitions were used to compare bowel sounds between patients with acute bowel obstruction vs subacute obstruction vs no obstruction[6-8]:
Acute bowel obstruction: Dilated bowel calibre (> 3 cm for small bowel, > 6 cm for large bowel) with symptoms of vomiting (for small bowel pathology) or no flatus/bowel motion for > 24 h (for large bowel pathology) and with CT/operative evidence of complete or high grade mechanical obstruction with a discrete transition point, collapsed distal segment, and little or no colonic gas present distal to the obstruction.
Subacute obstruction: Dilated bowel calibre (> 3 cm for small, > 6 cm for large bowel), with or without symptoms as per acute obstruction, but no CT/operative evidence of complete or high-grade mechanical obstruction (a poorly defined transition zone, incomplete collapse of distal bowel segment, and moderate colonic gas distal to the obstruction).
Acute (complete) or subacute (partial) mechanical obstruction of the bowel may be caused by herniation, adhesions, volvulus, intussusception, foreign body, phytobezoar, strictures, neoplasia, or wall oedema due to inflammatory conditions. Partial obstruction allows some liquid contents and gas to pass through the point of obstruction, whereas complete obstruction impedes passage of all bowel contents.
No obstruction: No clinical/CT/operative/endoscopic evidence of mechanical obstruction and other diagnosis was observed during the clinical course of the patient. Diagnoses such as constipation colic, faecal impaction, paralytic ileus, chronic megacolon, and pseudo-obstruction will be classified under this category.
Statistical analysis was performed using SPSS Version 12.0.1 (SPSS Inc. Chicago, Illinois, United States). Continuous non-parametric data were analysed using Mann-Whitney U test. A χ2 test was used to correlate the type of bowel sounds with the presence of obstruction. Pearson correlation was used to correlate bowel calibre with sound duration, sound-to-sound interval, dominant frequency, and peak frequency. Continuous data was presented as median values with inter-quartile ranges.
Seventy-one patients were recruited and had their bowel sounds recorded during the period July 2009 to January 2011. These patients had been admitted to our institution with abdominal symptoms, physical signs, or radiological findings suggestive of possible bowel obstruction.
There were 43 male and 28 female patients with age range from 22 to 93 years (mean 68 ± 16 years). Sixty-nine percent of patients presented with abdominal pain and 70.4% had a history of vomiting. Abdominal distension was present in 90.1% of the patients and abdominal tenderness was present in 33.8%. All patients had radiological imaging of the abdomen and pelvis. Plain film radiography was performed in all patients and CT was performed in 85.9% of patients.
Acute bowel obstruction was diagnosed in 40 patients (56.3%). Of these, 27 occurred in the small bowel and 13 occurred in the large bowel. Eleven patients (15.5%) had subacute bowel obstruction, of which eight occurred in the small bowel and three occurred in the large bowel. Twenty patients (28.2%) had no bowel obstruction. The diagnoses made for the non-obstructive conditions were ileus, pseudo-obstruction, gastritis, gastroenteritis, ileitis, colitis, constipation, cholecystitis, and bowel ischemia. Surgical intervention was performed in 25 patients (35.2%) during the same admission for the acute abdominal conditions.
Four hundred and twenty-six recordings were made from the 71 patients, of which 6 were of poor quality and were not used for analysis.
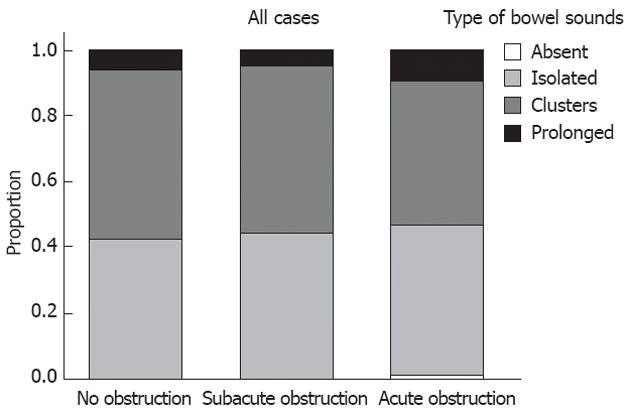
All types of bowel sounds were heard in all three groups of patients. Overall, isolated and clustered bowel sounds were heard most frequently in approximately equal proportions in all three groups of patients and prolonged sounds comprised 9.3% in the group with acute bowel obstruction (Figure 3).
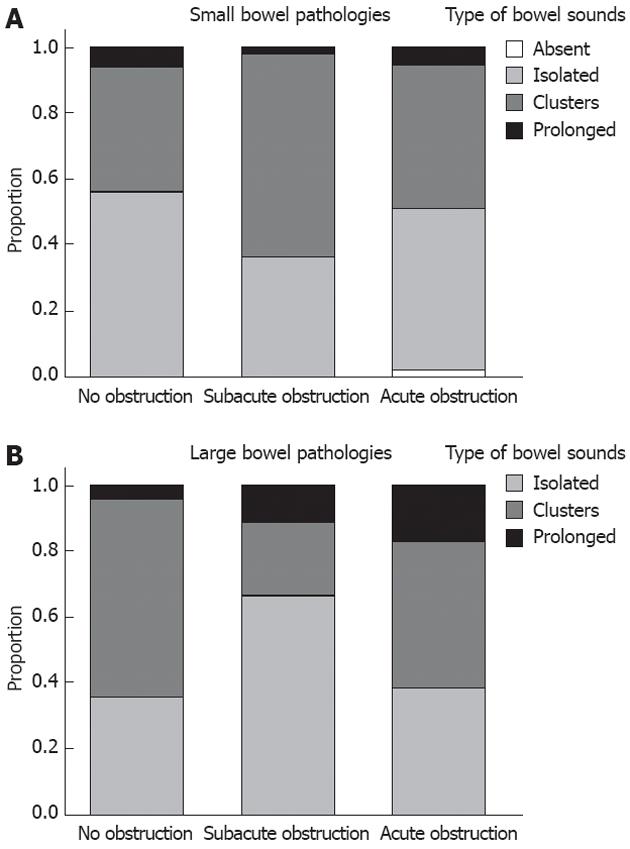
The cases were further analysed separately in subgroups of patients with small bowel pathologies and patients with large bowel pathologies. In the subgroup of patients with small bowel pathologies, the incidence of prolonged sounds were 6%, 2% and 6% with no obstruction, subacute obstruction and acute obstruction, respectively, and were not significantly different (P = 0.208) (Figure 4A). In the subgroup of patients with large bowel pathologies, the incidence of prolonged sounds increased significantly from 4% with no obstruction to 11% with subacute obstruction, and 17% with acute obstruction (P = 0.025) (Figure 4B).
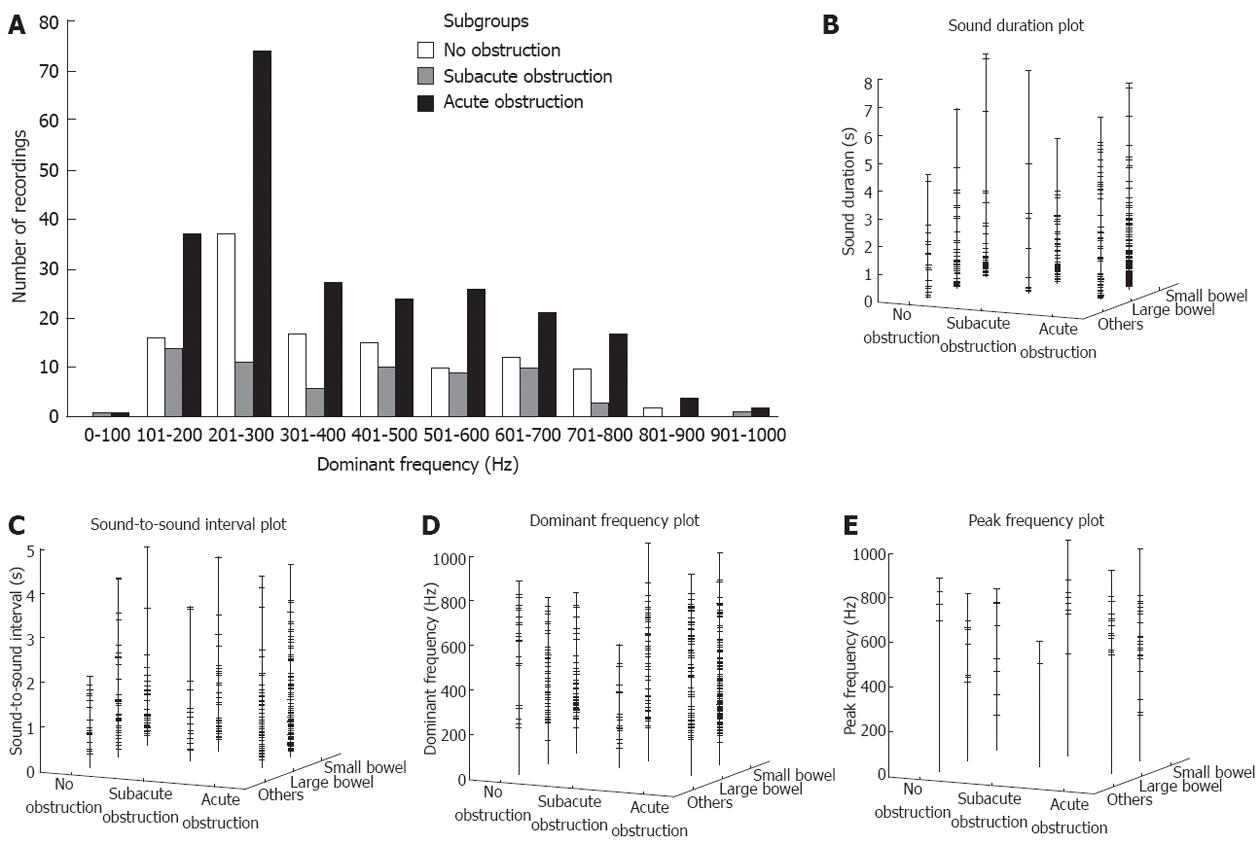
Among the groups of patients with no bowel obstruction, subacute obstruction, and acute obstruction, the distributions of dominant frequencies were similar, with the highest number of recordings with a dominant frequency in the 100 to 300 Hz range (Figure 5A). None of the recordings showed a dominant frequency of over 1000 Hz.
There was no significant difference between the sound characteristics in terms of sound duration (Figure 5B), sound-to-sound interval (Figure 5C), dominant frequency (Figure 5D), and peak frequency (Figure 5E) when comparisons were made among the groups of patients with acute bowel obstruction, subacute bowel obstruction, and no bowel obstruction. The results are summarised in Table 1.
| No obstruction (n = 20) | Subacute obstruction (n = 11) | Acute obstruction (n = 40) | P value | |
| Sound duration (s) | 0.64 (0.20-1.57) | 0.63 (0.23-1.67) | 0.69 (0.19-2.10) | > 0.05 |
| Sound-to-sound interval (s) | 0.72 (0.46-1.27) | 0.70 (0.47-1.67) | 0.75 (0.41-1.41) | > 0.05 |
| Dominant frequency (Hz) | 325 (225-530) | 405 (218-565) | 315 (225-545) | > 0.05 |
| Peak frequency (Hz) | 595 (378-713) | 655 (465-735) | 585 (530-706) | > 0.05 |
In the patient subset with acute bowel obstruction (n = 40), 27 patients had a small bowel obstruction and 13 had a large bowel obstruction. The sound characteristics in acute small and large bowel obstruction were compared (Table 2). The sound duration was significantly longer (P = 0.021) and the dominant frequency significantly higher (P = 0.003) in the large bowel obstruction group. The median peak frequency was about 100 Hz higher in the large bowel obstruction group, but the difference did not reach statistical significance (P = 0.060).
| Small bowel obstruction (n = 27) | Large bowel obstruction (n = 13) | P value | |
| Sound duration (s) | 0.55 (0.17-1.67) | 0.87 (0.27-3.60) | 0.021 |
| Sound-to-sound interval (s) | 0.72 (0.41-1.40) | 0.78 (0.44-1.42) | 0.621 |
| Dominant frequency (Hz) | 288 (220-479) | 440 (250-643) | 0.003 |
| Peak frequency (Hz) | 560 (480-695) | 660 (578-740) | 0.060 |
Comparison was made between patients with acute large bowel obstruction and the three patients with pseudo-obstruction of the large bowel (Table 3). There was no significant difference in the sound characteristics between the two groups. Comparison between patients with a small bowel obstruction and a pseudo-obstruction (Table 4) showed significantly longer sound duration, longer sound-to-sound interval, and higher dominant frequency in patients with a pseudo-obstruction.
| Large bowel obstruction (n = 13) | Large bowel pseudo-obstruction (n = 3) | P value | |
| Sound duration (s) | 0.87 (0.27-3.60) | 1.24 (0.53-2.64) | 0.686 |
| Sound-to-sound interval (s) | 0.78 (0.44-1.42) | 1.08 (0.68-2.23) | 0.061 |
| Dominant frequency (Hz) | 440 (250-643) | 488 (389-679) | 0.174 |
| Peak frequency (Hz) | 660 (578-740) | 630 (525-750) | 0.638 |
| Small bowel obstruction (n = 27) | Large bowel pseudo-obstruction (n = 3) | P value | |
| Sound duration (s) | 0.55 (0.17-1.67) | 1.24 (0.53-2.64) | 0.048 |
| Sound-to-sound interval (s) | 0.72 (0.41-1.40) | 1.08 (0.68-2.23) | 0.041 |
| Dominant frequency (Hz) | 288 (220-479) | 488 (389-679) | 0.001 |
| Peak frequency (Hz) | 560 (480-695) | 630 (525-750) | 0.446 |
Analysis was performed on the 35 patients with a small bowel obstruction (27 acute obstruction and eight subacute obstruction included). Twenty-six patients (74%) with a small bowel obstruction were caused by (or presumed to be caused by) adhesions when there was a previous history of abdominal operation(s), CT (performed on 30 patients) did not find any mass lesion causing the obstruction, or the diagnosis confirmed during surgical exploration. Other causes of obstruction were small bowel volvulus (n = 3), bowel non-rotation (n = 1), femoral hernia (n = 1), parastomal hernia (n = 1), omental mass invasion (n = 1), and unknown (n = 2). The bowel sounds characteristics were compared between those who were treated conservatively (n = 25) vs those who were operated on (n = 10) (Table 5). The dominant frequency and peak frequency between non-operated and operated groups were not significantly different. The sound duration in the operated group was longer than the non-operated group, but the difference did not reach statistical significance. The sound-to-sound interval was significantly longer in the operated group (P < 0.001).
| Small bowel obstruction, non operated (n = 25) | Small bowel obstruction, operated (n = 10) | P value | |
| Sound duration (s) | 0.55 (0.21-1.45) | 1.00 (0.25-2.26) | 0.100 |
| Sound-to-sound interval (s) | 0.63 (0.39-1.13) | 1.29 (0.61-1.82) | < 0.001 |
| Dominant frequency (Hz) | 360 (225-560) | 265 (210-455) | 0.084 |
| Peak frequency (Hz) | 625 (535-713) | 525 (400-738) | 0.432 |
Analysis of bowel sounds was made in relation to bowel dilatation in acutely obstructed bowel. There was no correlation between the small bowel calibre (4.8 ± 1.6 cm) and the sound duration (r = -0.046, P = 0.567), sound-to sound interval (r = -0.020, P = 0.817), dominant frequency (r = 0.025, P = 0.753), and peak frequency (r = -0.208, P = 0.298) for acute small bowel obstruction. Similarly, for acute large bowel obstruction, there was no correlation between the large bowel calibre (8.2 ± 1.7 cm) and sound duration (r = -0.103, P = 0.372), sound-to-sound interval (r = -0.077, P = 0.535), dominant frequency (r = -0.022, P = 0.847), and peak frequency (r = -0.028, P = 0.927).
Bowel sounds are generated by contractions of the alimentary tract, and mixing of gaseous and liquid contents[9]. The quality of bowel sounds varies according to the state of bowel activity[10,11]. Bowel sounds are complex, and each sound comprises a mixture of tones and is often a sequence of closely connected sounds. Common descriptions of bowel sounds include gurgling or rattling or rustling noise heard in a normal person, rumbling explosions heard with gastroenteritis, succussion splash heard in gastric outlet obstruction, diminished, i.e., infrequent, and soft sounds, and prolonged tinkling or high-pitched metallic sounds that may be heard in bowel obstruction. Very diminished or absent bowel sounds may be caused by bowel obstruction, intestinal ischemia, paralytic ileus, and peritonitis.
The published literature on auscultation of bowel sounds has been rather scarce over the past century. Since Cannon described the rhythmic sounds produced by the stomach and intestines more than 100 years ago, very few papers have been published on this subject[12].
Advances in technology have allowed various systems to be developed for the objective analysis of bowel sounds. Spectral analysis of bowel sounds was first described by Horn et al[13] in 1966. The spectrogram that their apparatus produced was a complex record, which was difficult to understand, and the frequency range of their apparatus was too small. Work by Watson et al[14] in 1967 found that bowel sounds have a frequency range of at least 150 Hz to 5000 Hz, with peaks detected at frequencies of up to 2000 Hz. These very high frequencies were not seen in our study, where the peak dominant frequency of bowel sounds recorded never reached above 1000 Hz in any of our recordings.
Yoshino et al[15] in 1990 attempted a computer analysis of bowel sounds in intestinal obstruction. The number of subjects studied was small (n = 21). The peak frequency of patients with intestinal obstruction in the subgroup of patients that required surgery (612 ± 86 Hz, n = 5) was significantly higher compared with the subgroup that did not require surgery (273 ± 64 Hz, n = 3). The authors concluded that computer analysis of bowel sounds of mechanical obstruction could provide a very objective assessment of severity, and could help determine the treatment regimen (conservative or operative) of each patient. However, our data on patients with small bowel obstruction showed that the subgroup that subsequently underwent surgery (n = 10) did not have any significant difference in the dominant or peak frequencies when compared with the subgroup that did not undergo surgery (n = 25). Instead, there was a significantly longer sound-to-sound interval in the subgroup that underwent surgery compared with the subgroup that was treated conservatively. The explanation for this is difficult, but it may be that in situations where the small bowel obstruction does not resolve and subsequently requires surgery, the affected bowel is more prone to ischemia and fatigue, becoming more distended and resulting in less frequent peristaltic activities and recordable sounds[10,16].
The study by Sugrue et al[17] in 1994 compared characteristics of bowel sounds in controls (n = 63) and patients with acute appendicitis (n = 25), acute cholecystitis (n = 15), and bowel obstruction (n = 21). This study compared sound number, duration, interval, and amplitude but not frequency of bowel sounds. It was found that in bowel obstruction, the sound duration, interval, and amplitude all significantly increased when compared to control subjects. However, in our current study, there was no significant difference in the sound duration and sound-to-sound interval between obstructed and non-obstructed bowel.
The current study is, so far, the largest series of patients with intestinal obstruction investigated for bowel sounds (n = 51). This study has shown objectively that bowel sound characteristics, in general, are not significantly different between patients with acute, subacute, or no intestinal obstruction using the commonly compared parameters, including sound duration, sound-to-sound interval, and dominant and peak frequencies. However, the obstructed large bowel has significantly longer sound duration (median 0.87 s vs 0.56 s) and higher dominant frequency (median 440 Hz vs 288 Hz) when compared to obstructed small bowel. The possible explanations for these differences are that movements within the colon usually involve less frequent peristalsis but larger volume shift with each peristalsis and, therefore, in the presence of an obstruction, a longer time elapses when fluid and gas are forced to pass through a tight stenosis. The higher sound frequency in large bowel obstruction can be explained by the fact that the majority of ileocecal valves are competent[18,19]. In the event of large bowel obstruction, the pressure rises within the “closed loop” segment of the colon proximal to the point of obstruction. Progressive distension of the colon increases the tension on the colonic wall, as well as thinning of the wall; hence, vibration is produced at a higher frequency. In small bowel obstruction, the pressure within the obstructed segment of bowel is usually limited by reflux of the small bowel contents back into the stomach (except in the presence of certain uncommon situations causing a closed loop obstruction), hence the common presentation of vomiting in small bowel obstruction.
In the small group of patients with large bowel pseudo-obstruction, the sound characteristics were similar to those with large bowel obstruction. This is not surprising, because in both conditions the large bowel can be grossly distended. The point of “obstruction” in patients with pseudo-obstruction is often caused by a high resting anal sphincter tone, which impedes the evacuation of flatus and faeces. This can be identified by digital rectal examination and the findings of a tight anus, which precludes easy entry of the examining finger. Upon entry of the finger, the rectum can be felt to be capacious and mainly gas and fluid filled.
The intrinsic difficulty with the study of bowel sounds is that it is never possible to hear or record exactly the same pattern of bowel sounds with exactly same amplitude, frequency, duration and interval repeatedly and consistently as compared to the consistent sounds produced from the heart, which has a set rhythm and sound characteristics over time. The bowel sounds heard from the same patient will also differ at different times when the patient is re-examined. Therefore intrasubject reproducibility of repeat recording was not evaluated in this study. The wide range of physiological variations means that the clinical significance of bowel sounds is limited. There is no clear evidence that high-pitched bowel sounds have clinical pertinence[20]. The recording of bowel sound yields only the sum of the motility of all areas of the alimentary track, so no statements are possible about the activity of any particular segment by comparison of sounds at different recording sites[21].
In this study, the recording of six 8-second tracts of bowel sounds performed over a few minutes may not be representative of the overall pattern over a longer period. The technical ability to perform continuous recording over a longer period is more likely to provide better representation of the whole picture, as well as improving intrasubject reproducibility. Recent biomedical engineering experimental studies have utilised bowel sounds to assess bowel motility and their techniques have shown good potential for monitoring and estimation of bowel motility[22-25]. Incorporation of these technologies into a portable electronic stethoscope might improve the recording, analysis, and interpretation of clinical data.
Auscultation of bowel sounds is a traditional technique for evaluating patients with abdominal symptoms. It is simple, but is generally empirical and too subjective. There is a distinct lack of clinical research to support the value of auscultation for bowel sounds.
Recording of bowel sounds with objective evaluation has become possible with commercially available electronic stethoscopes. In this study, the authors aimed to determine the value of objective assessment of bowel sounds provided by an electronic stethoscope in supporting a clinical diagnosis of intestinal obstruction. Correlation with radiological and operative findings, and clinical outcome was made to identify characteristic bowel sounds that will improve the diagnostic accuracy for bowel obstruction.
This is the largest study examining bowel sounds for intestinal obstruction using a commercially available electronic stethoscope. Bowel sounds recorded for different conditions, including acute and subacute obstruction of the small bowel and large bowel, pseudo-obstruction of large bowel, and patients with no bowel obstruction were compared using measurable parameters, such as sound duration, sound-to-sound interval, dominant frequency, and peak frequency. The most important breakthroughs from this study are that large bowel obstruction has a significantly longer sound duration and higher dominant frequency than small bowel obstruction. Furthermore, bowel sounds in pseudo-obstruction of the large bowel mimic acute large bowel obstruction; therefore, auscultation is of less value in differentiating between these two conditions. Small bowel obstruction that resolved with conservative management had shorter sound-to-sound interval than those that eventually needed surgery.
By understanding the differences in bowel sound qualities among various acute obstructive conditions of the bowel, practitioners can use their past experience and clinical judgement when auscultating and interpreting bowel sounds in an acute abdomen.
Bowel sound duration, sound-to-sound interval, dominant frequency, and peak frequency are the main parameters used to analyse bowel sounds. The reasons for the observed differences among conditions, including acute and subacute obstruction, small and large bowel obstruction, were discussed.
The authors assessed the value of objective analysis of bowel sounds in a unique group of patients who presented with a common, yet challenging, abdominal condition. The data presented in this study showed that auscultation of bowel sounds, seemingly so simple to perform, becomes very complex when subjected to a scientific study. Bowel sounds on their own may not be specific enough to provide a diagnosis of bowel obstruction. The combination of clinical and radiological assessments remains the standard for diagnosing bowel obstruction.
Peer reviewer: Fernando Azpiroz, MD, Digestive System Research Unit, University Hospital Vall d’Hebron, Paseo Vall d’Hebron, 119-129, 08035 Barcelona, Spain
S- Editor Lv S L- Editor Stewart GJ E- Editor Li JY
| 1. | Gade J, Kruse P, Andersen OT, Pedersen SB, Boesby S. Physicians' abdominal auscultation. A multi-rater agreement study. Scand J Gastroenterol. 1998;33:773-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Gu Y, Lim HJ, Moser MA. How useful are bowel sounds in assessing the abdomen? Dig Surg. 2010;27:422-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Hepburn MJ, Dooley DP, Fraser SL, Purcell BK, Ferguson TM, Horvath LL. An examination of the transmissibility and clinical utility of auscultation of bowel sounds in all four abdominal quadrants. J Clin Gastroenterol. 2004;38:298-299. [PubMed] |
| 5. | Georgoulis B. Bowel sounds. Proc R Soc Med. 1967;60:917-920. [PubMed] |
| 6. | Frager D, Medwid SW, Baer JW, Mollinelli B, Friedman M. CT of small-bowel obstruction: value in establishing the diagnosis and determining the degree and cause. AJR Am J Roentgenol. 1994;162:37-41. [PubMed] |
| 7. | Maglinte DD, Reyes BL, Harmon BH, Kelvin FM, Turner WW, Hage JE, Ng AC, Chua GT, Gage SN. Reliability and role of plain film radiography and CT in the diagnosis of small-bowel obstruction. AJR Am J Roentgenol. 1996;167:1451-1455. [PubMed] |
| 8. | Suri S, Gupta S, Sudhakar PJ, Venkataramu NK, Sood B, Wig JD. Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol. 1999;40:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 127] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Politzer JP, Devroede G, Vasseur C, Gerard J, Thibault R. The genesis of bowel sounds: influence of viscus and gastrointestinal content. Gastroenterology. 1976;71:282-285. [PubMed] |
| 10. | Woolsey JH. Auscultation of the Abdomen. Cal West Med. 1939;50:105-109. [PubMed] |
| 11. | Arnbjörnsson E. Normal and pathological bowel sound patterns. Ann Chir Gynaecol. 1986;75:314-318. [PubMed] |
| 12. | Cannon WB. Auscultation of the rhythmic sounds produced by the stomach and intestines. Am J Physiol. 1905;14:339-353. |
| 13. | Horn GE, Mynors JM. Recording the bowel sounds. Med Biol Eng. 1966;4:205-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Watson WC, Knox EC. Phonoenterography: the recording and analysis of bowel sounds. Gut. 1967;8:88-94. [PubMed] |
| 15. | Yoshino H, Abe Y, Yoshino T, Ohsato K. Clinical application of spectral analysis of bowel sounds in intestinal obstruction. Dis Colon Rectum. 1990;33:753-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 39] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Ruf W, Suehiro GT, Suehiro A, Pressler V, McNamara JJ. Intestinal blood flow at various intraluminal pressures in the piglet with closed abdomen. Ann Surg. 1980;191:157-163. [PubMed] |
| 17. | Sugrue M, Redfern M. Computerized phonoenterography: the clinical investigation of a new system. J Clin Gastroenterol. 1994;18:139-144. [PubMed] |
| 18. | Love L. The role of the ileocecal valve in large bowel obstruction. A preliminary report. Radiology. 1960;75:391-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Gazet JC. The surgical significance of the ileo-caecal junction. Ann R Coll Surg Engl. 1968;43:19-38. [PubMed] |
| 20. | Moll van Charante EP, de Jongh TO. [Auscultation of the abdomen]. Ned Tijdschr Geneeskd. 2011;155:A2657. [PubMed] |
| 21. | Connell AM. The assessment of intestinal motility. Proc R Soc Med. 1966;59 Suppl:6-9. [PubMed] |
| 22. | Yamaguchi K, Yamaguchi T, Odaka T, Saisho H. Evaluation of gastrointestinal motility by computerized analysis of abdominal auscultation findings. J Gastroenterol Hepatol. 2006;21:510-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Dimoulas C, Kalliris G, Papanikolaou G, Kalampakas A. Long-term signal detection, segmentation and summarization using wavelets and fractal dimension: a bioacoustics application in gastrointestinal-motility monitoring. Comput Biol Med. 2007;37:438-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Ranta R, Louis-Dorr V, Heinrich C, Wolf D, Guillemin F. Digestive activity evaluation by multichannel abdominal sounds analysis. IEEE Trans Biomed Eng. 2010;57:1507-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Kim KS, Seo JH, Song CG. Non-invasive algorithm for bowel motility estimation using a back-propagation neural network model of bowel sounds. Biomed Eng Online. 2011;10:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |