Published online Aug 7, 2012. doi: 10.3748/wjg.v18.i29.3869
Revised: April 16, 2012
Accepted: May 12, 2012
Published online: August 7, 2012
AIM: To study the short-term outcome of patients treated with laparoscopic right colectomy and how intracorporeal anastomosis has improved the outcome.
METHODS: We retrospectively examined all patients affected by colorectal cancer who underwent a laparoscopic right colectomy between January 2006 and December 2010 in our department. Our evaluation criteria were: diagnosis of colorectal carcinoma at presurgical biopsy, elective surgery, and the same surgeon. We excluded: emergency surgery, conversions from laparotomic colectomy, and other surgeons. The endpoints we examined were: surgical time, number of lymph nodes removed, length of stay (removal of nasogastric tube, bowel movements, gas evacuation, solid and liquid feeding, hospitalization), and major complications. Seventy-two patients were divided into two groups: intracorporeal anastomosis (39 patients) and extracorporeal anastomosis (33 patients).
RESULTS: Significant differences were observed between intracorporeal vs extracorporeal anastomosis, respectively, for surgical times (186.8 min vs 184.1 min, P < 0.001), time to resumption of gas evacuation (3 d vs 3.5 d, P < 0.001), days until resumption of bowel movements (3.8 d vs 4.9 d, P < 0.001), days until resumption of liquid diet (3.5 d vs 4.5 d, P < 0.001), days until resuming a solid diet (4.6 d vs 5.7 d, P < 0.001), and total hospitalization duration (7.4 d vs 8.5 d, P < 0.001). In the intracorporeal group, on average, 19 positive lymph nodes were removed; in the extracorporeal group, on average, 14 were removed P < 0.001). Thus, intracorporeal anastomosis for right laparoscopic colectomy improved patient outcome by providing faster recovery of nutrition, faster recovery of intestinal function, and shorter hospitalization than extracorporeal anastomosis.
CONCLUSION: Short-term outcomes favor intracorporeal anastomosis, confirming that a less traumatic surgical approach improves patient outcome.
- Citation: Anania G, Santini M, Scagliarini L, Marzetti A, Vedana L, Marino S, Gregorio C, Resta G, Cavallesco G. A totally mini-invasive approach for colorectal laparoscopic surgery. World J Gastroenterol 2012; 18(29): 3869-3874
- URL: https://www.wjgnet.com/1007-9327/full/v18/i29/3869.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i29.3869
Over the last decades, colorectal laparoscopic surgery has outachieved traditional surgery for safety and oncological radicality. Some studies such as COST[1], CLASICC[2], Barcelona[3], and COLOR[4] have shown short-term postoperative advantages without compromising long-term oncological results. For right colectomy, laparoscopic surgery was established later because of technical difficulties related to anatomic and vascular variability[5]. The re-establishment of intestinal transit with ileocolic anastomosis can be performed with two techniques: extracorporeal anastomosis and intracorporeal anastomosis. In extracorporeal anastomosis, also called “laparoscopic-assisted colectomy”, stitching (manual or mechanical) and vascular resection are done extracorporeally by externalizing the bowel through a cutaneous mini-incision. On the other hand, the other type of anastomosis is totally intracorporeal, and the stitching is often performed mechanically. A case-control study showed that laparoscopic right colectomy performed with intracorporeal anastomosis is considered one of the most difficult surgeries after transverse resection, rectum resection, and recanalization after Hartmann’s resection. However, the ligation of ileocolic vessels and the medial-to-lateral dissection of the right mesocolon intracorporeally are more oncologically safe in terms of the number of lymph nodes removed and cancer management. Nevertheless, extracorporeal anastomosis is the most popular as the literature shows, although it has some limitations in terms of the number of accesses and complications after bowel externalization[6-11].
We evaluated the short-term outcome of patients with colorectal cancer who underwent a laparoscopic right colectomy, and we showed that intracorporeal anastomosis improved patient outcome (shorter hospitalization, fewer postoperative complications, and better oncological radicality). Finally, we considered the influence of the “learning curve” on these surgical techniques.
We retrospectively examined all patients with colorectal cancer who underwent a laparoscopic right colectomy between January 2006 and December 2010 in our department. Our evaluation criteria were elective surgery and the same surgeon as the first operator. We excluded patients undergoing emergency surgery, conversions from laparotomic colectomy, and other surgeons as the first operator. Patients were divided into two groups: the first included those who underwent a right colectomy with intracorporeal anastomosis, and the second included those who underwent a right colectomy with extracorporeal anastomosis. Patient data included age, gender, body mass index (BMI), American Society of Anesthesiology (ASA) class, and surgical history. We also obtained other data concerning the operation including the surgical time, preoperative diagnosis, and number of lymph nodes removed. We noted parameters of post-surgery hospitalization including removal of nasogastric tube, resumption of bowel movements, resumption of gas evacuation, time to consumption of solid and liquid feeding. We also considered major complications in terms of post-surgery time and hospitalization.
We obtained data from medical records, surgical cards, and databases. We used JMP software 7a Version [SAS Institute Inc. (1989-2007), Cary, NC, United States] for electronic data processing. Descriptive variables were expressed as mean, standard deviation, mode, median, number of events, patients, and percentage. According to the different features of these variables, we used the χ2 test, F test, and Student’s t test as appropriate, and considered P < 0.05 to indicate statistical significance.
In this study, 72 patients were divided into two groups: intracorporeal anastomosis (n = 39) and extracorporeal anastomosis (n = 33). There were no significant differences in age, gender, BMI (Table 1), or ASA class between the two groups (P = 0.8645 for ASA).
| Patients | Intracorporeal | Extracorporeal | ||
| n = 39 | n = 33 | |||
| Age (yr) | Median | 74.5 | 74 | NS |
| Min-max | 53-89 | 45-96 | ||
| Gender | Male | 24 | 20 | NS |
| Female | 15 | 13 | ||
| Ratio M/F | 1.6 | 1.5 | ||
| Weight (kg) | Median | 71 | 77 | NS |
| Min-max | 50-90 | 51-120 | ||
| Height (cm) | Median | 165 | 167 | NS |
| Min-max | 148-182 | 146-183 | ||
| BMI (kg/m2) | Median | 26.3 | 28.1 | NS |
| Min-max | 20-37 | 19.9-37 | ||
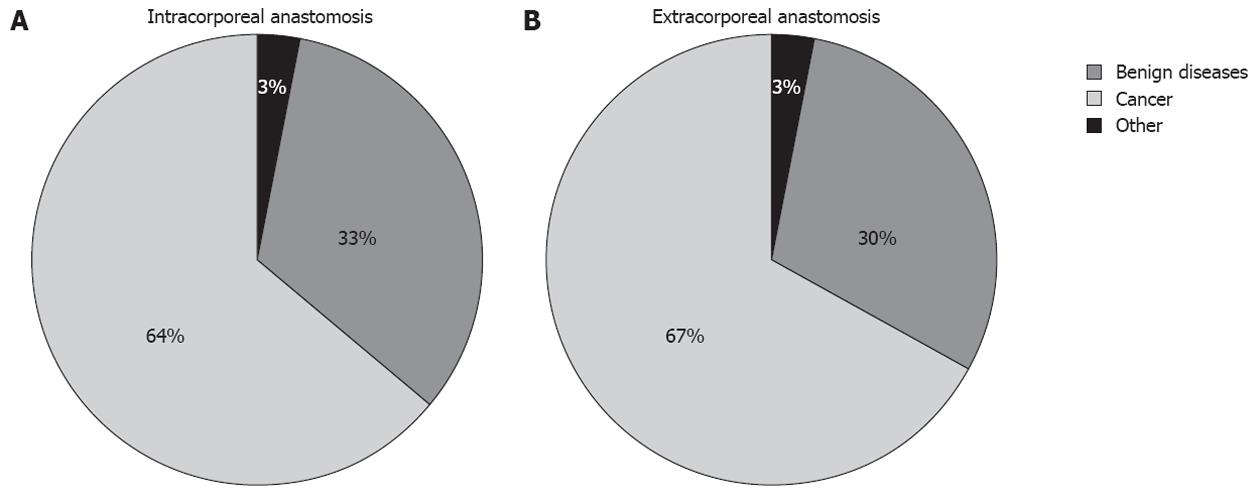
Twenty patients in the intracorporeal group had a positive abdominal surgical history (51.3%), whereas 21 patients in the extracorporeal group had such a history (63.6%; P = 0.8433, Table 2). There were also no significant differences in the diagnosis from the pre-surgery biopsy (Figure 1).
| Intracorporeal anastomosis | Extracorporeal anastomosis | ||
| 20/39 (51.3%) | 21/33 (63.6%) | ||
| One operation | 11 | One operation | 14 |
| Two operations | 7 | Two operations | 7 |
| > Two operations | 2 | > Two operations | 7 |
| Appendectomy | 9 | Appendectomy | 15 |
| Colic resection | 2 | Colic resection | 1 |
| Isteroannessectomy | 4 | Isteroannessectomy | 2 |
| Cholecystectomy | 5 | Cholecystectomy | 1 |
| Urologic surgery | 4 | Urologic surgery | 1 |
| Hernioplasty | 2 | Hernioplasty | 9 |
In the intracorporeal group, we performed additional surgical procedures in seven patients during surgery, i.e., one nefrectomy, five colecistectomies, and one intraoperative coloscopy, whereas in the extracorporeal group, we performed two colecistectomies, one intraoperative coloscopy, and one polipectomy.
In the intracorporeal group, we removed an average of 19 lymph nodes (range: 7-36), whereas in the extracorporeal group we removed an average of 14 lymph nodes (range: 2-29, P < 0.0001).
The average surgical time was 186.8 min (range: 105-280 min) in the intracorporeal group and 184.1 min in the extracorporeal group (range: 115-285 min, P = 0.6549).
Gas evacuation was shorter in the intracorporeal group than in the extracorporeal group (3 ± 1.05 d vs 3.5 ± 1.1 d, range: 1-6 d, P < 0.0001). Bowel movements occurred earlier in the intracorporeal group (3.8 ± 1.4 d, range: 1-7 d vs 4.9 ± 1.5 d, range: 2-8 d, P < 0.0001). In addition, the NGT was removed sooner in the intracorporeal group than in the extracorporeal group (1.8 d and 3 d, respectively, P < 0.0001).
Resumption of a liquid diet occurred an average of (3.5 ± 2.2 d, range: 2-12 d, P < 0.0001) after intracorporeal anastomosis and (4.5 ± 1.7 d, range: 2-10 d, P < 0.0001) after extracorporeal anastomosis. Resumption of a solid diet occurred (4.6 ± 2.1 d, range 2-12 d) and after intracorporeal and extracorporeal anastomosis, respectively (5.7 ± 1.7 d, range: 3-11 d, P < 0.0001).
Total hospitalization time was significantly less after intracorporeal anastomosis (average of 7.4 ± 3.2 d, range: 4-19 d) than after extracorporeal anastomosis (average of 8.5 ± 3.9 d, range: 5-25 d, P < 0.0001; Table 3).
| Intracorporeal anastomosis | Extracorporeal anastomosis | P value | ||
| Time until resumption of gas evacuation (d) | Median | 3 | 3.5 | < 0.0001 |
| Min-max | 1-6 | 1-6 | ||
| Time until resumption of bowel movements (d) | Median | 3.8 | 4.9 | < 0.0001 |
| Min-max | 1-7 | 2-7 | ||
| Time until removal of nasogastric tube (d) | Median | 1.8 | 3 | < 0.0001 |
| Min-max | 0-11 | 0-6 | ||
| Time until resumption of liquid diet (d) | Median | 3.5 | 4.5 | < 0.0001 |
| Min-max | 2-12 | 2-10 | ||
| Time to resumption of solid diet (d) | Median | 4.6 | 5.7 | < 0.0001 |
| Min-max | 2-12 | 3-11 | ||
| Discharge (d) | Median | 7.4 | 8.5 | NS |
| Min-max | 4-19 | 5-25 | 0.5424 |
Major complications occurred in 10.2% of patients undergoing intracorporeal anastomosis, i.e., three patients: one with severe anemia, one with anastomotic dehiscence, and one with enterocutaneous fistula. In the extracorporeal group, 12.1% of patients had major complications, i.e., five patients: two with severe anemia, one with occlusion, one with anastomotic dehiscence, and one with enterocutaneous fistula.
Our study shows that intracorporeal anastomosis for right laparoscopic colectomy improved patient outcome compared with patients who underwent extracorporeal anastomosis. With intracorporeal anastomosis, we found faster recovery of nutrition, faster recovery of intestinal function, and shorter hospitalization. However, there was no difference in average surgery time between the two groups.
According to the inclusion and exclusion criteria, we obtained two homogeneous and comparable groups without significant differences in age, gender, BMI (Tables 1 and 4), ASA class, or abdominal surgical history (Table 2). In laparoscopic right colectomy with extracorporeal anastomosis (laparoscopic-assisted colectomy), the bowel is externalized through a lateral mini-incision. With this approach, bowel mobilization and ligation of vessels is usually laparoscopic, whereas resection of the specimen and creation of the anastomosis is extracorporeal. On the other hand, in laparoscopic right colectomy with intracorporeal anastomosis (totally laparoscopic colectomy), bowel mobilization, ligation of vessels, resection of the specimen, and creation of the anastomosis are totally intracorporeal.
| Intracorporeal | Extracorporeal | |
| Age (yr) | ||
| < 65 | 13.6 | 12.1 |
| 65-80 | 43.2 | 48.5 |
| > 80 | 43.2 | 33.4 |
| BMI (kg/m2) | ||
| < 25 | 44.4 | 26.9 |
| 25-30 | 40.7 | 53.1 |
| > 30 | 14.9 | 23.0 |
| Number of lymph nodes removed | ||
| < 12 | 7 (21.2) | 14 (46.7) |
| 12-15 | 6 (18.2) | 6.6 (2) |
| > 15 | 20 (60.6) | 14 (46.7) |
| Discharge from hospital (d) | ||
| < 6 | 15 (42.8) | 8 (24.4) |
| 7 | 10 (28.6) | 10 (30.3) |
| 8-9 | 5 (14.3) | 8 (24.2) |
| > 10 | 5 (14.3) | 7 (21.1) |
In our experience, right colectomy with intracorporeal anastomosis has been standardized step by step: first, ileocolic vessels are isolated, secured between clips, and divided near their origin. Then, the right mesocolon is dissected medial-to-lateral, and the small bowel mesentery is divided to reach the edge of the terminal ileum. Then, the specimen is resected with an Endo-GIA stapler. The end the Endo-GIA stapler is deployed through the bowel openings to form a side-to-side anastomosis. The last step is specimen extraction and wound closure. We did not standardize the right colectomy with extracorporeal anastomosis; in 36.4% of cases, the ligation of vessels was performed after partial bowel mobilization, whereas in 63.6% of cases, it was the first step of the surgical procedure. Finally, the anastomosis was realized manually, lateral-to-lateral, in a double layer.
Both techniques are oncologically safe; according to the latest Union for International Cancer Control Tumor Node Metastasis classification, removal of at least 12 lymph nodes is fundamental to guarantee sufficient oncological radicality[12].To achieve this goal, the arterial vessels must be ligated at the origin from the superior mesenteric artery. When vascular ligation is extracorporeal, it is very difficult to obtain an adequate number of lymph nodes[13]. Bergamaschi et al[14] showed that extracorporeal vascular oncologic ligation is very difficult through a small cutaneous incision, and the bowel undergoes a hard traction with this technique. Hellan et al[15] emphasized that the limitations of extracorporeal vascular ligation include poor exposure of the ileocolic pedicle through the small incision. Difficult exposure of the base of the mesentery could compromise the oncological result. That is why some surgeons propose the technique of intracorporeal high-vessel ligation combined with extracorporeal anastomosis[16-19].
Regarding oncological radicality, we found significant differences in the number of lymph nodes removed. We removed an average of 19 lymph nodes from the intracorporeal group and 14 lymph nodes from the extracorporeal group. In particular, in the first group we removed more than 15 lymph nodes in 60% of patients, 12 to 15 lymph nodes in 18.2% of patients, and fewer than 12 lymph nodes in 21% of patients. In the extracorporeal group, we removed more than 15 lymph nodes in 46.7% of patients, 12 to 15 lymph nodes in 6.6% of patients, and fewer than 12 lymph nodes in 46.7% of patients (Table 4). Thus, our experience shows that there is an important difference in the number of positive lymph nodes removed in the intracorporeal group, and also on the percentage of patients in which more than 12 lymph nodes were removed (P < 0.0001). The explanation for this difference is the missed ligation of vessels before the mobilization of the right colon. We believe that is very difficult to obtain an adequate number of lymph nodes when vessel division is not the first step in laparoscopic right colectomy.
In the literature, some authors have reported no differences in safety, whereas others noted that the only advantage was a smaller incision[20,21]. On the other hand, other studies affirmed the safety of intracorporeal anastomosis, with the same complication rate as for extracorporeal anastomosis[22,23].
Because intracorporeal anastomosis is considered more difficult, only a few surgeons have used this kind of technique; however less mobilization is required, and less tension is applied to the bowel and mesentery because the bowel does not need to reach the anterior abdominal wall for externalization. Furthermore, the excessive tension on the mesentery during the mobilization is associated with an increased risk of mesenteric or portal vein thrombosis[24].
Concerning surgical times, we did not find a significant difference in surgical time between the two groups.
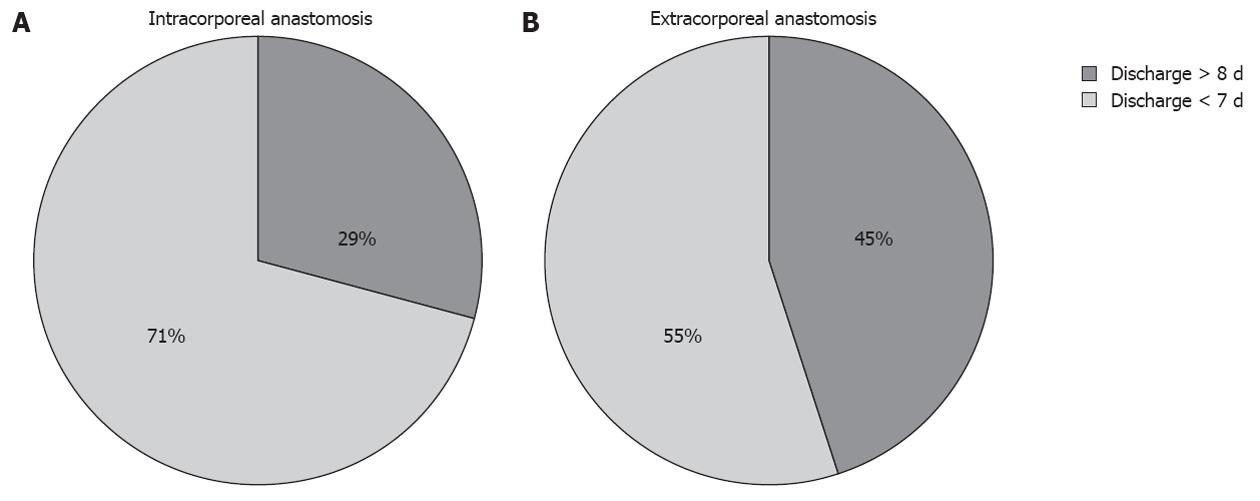
Patients in the intracorporeal group had a shorter hospitalization duration. In some cases, the hospitalization duration was longer possibly because of age (43.2% of patients in the intracorporeal group and 33.4% in the extracorporeal group were over 80 years old). Our results showed a significantly shorter average hospitalization stay in the intracorporeal group (Table 4). These data agree with a recent Spanish study[25], although this difference was not significant (P = 0.5424) because hospitalization duration is influenced by many patient factors. On the other hand, we found that 71.4% of patients in the intracorporeal group went home within 7 d, and 54.7% of patients in the extracorporeal group went home within this period (P = 0.0001, Figure 2).
Concerning the recovery of intestinal function, our results found significantly shorter average times for resumption of gas evacuation after 3 d in the intracorporeal group compared to after 3.8 d in the extracorporeal group. Bowel movements occurred after an average of 4.9 d in the intracorporeal group. In the intracorporeal group, the nasogastric tube was removed after 1.8 d, whereas it was removed after 3 d in the extracorporeal group. This difference can be explained by an increased percentage of paralytic ileum in the second group, which is due to the traction of the right colon and terminal ileum through the mini-incision on the pancreas and duodenum[26]. This approach allowed a more rapid recovery of liquid and solid nutrition consumption.
We analyzed major complications, which included severe anemia, occlusion, anastomotic dehisces, and enterocutaneous fistulae. There were no significant differences between the two groups.
In conclusion, our study clearly shows that laparoscopic right colectomy with intracorporeal anastomosis improves patient outcome. We found that intracorporeal anastomosis resulted in faster recovery of nutrition consumption, faster recovery of intestinal function, and shorter hospitalization duration. The higher number of lymph nodes removed seems to be related to vascular division as the first surgical step as a rule. This confirms that a mini invasive approach improves patient outcome.
A lot of studies have demonstrated the benefits of laparoscopic right colectomy, proving the short-term outcome of patients. The aim of this study is to show how intracorporeal anastomosis in laparoscopic right colectomy has further improved patient outcome.
In the area of mini-invasive surgery, intracorporeal anastomosis, confirm that a less traumatic surgical approach improves patient outcome.
Based on a large series, this study describes the outcome of patients treated with laparoscopic right colectomy and is a reference for comparison in future studies.
The study results show how laparoscopic right colectomy with intracorporeal anastomosis improves patients outcome. This study suggest that all patients treated with intracorporeal anastomosis have faster recovery of nutrition consumption, faster recovery of intestinal function, and shorter hospitalization duration.
This paper demonstrated the outcomes of patients treated with laparoscopic right colectomy with intracorporeal anastomosis.
Peer reviewer: Dr. Ashok Kumar, Surgical Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow 226014, India
S- Editor Gou SX L- Editor A E- Editor Li JY
| 1. | Tinmouth J, Tomlinson G. Laparoscopically assisted versus open colectomy for colon cancer. N Engl J Med. 2004;351:933-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jaine DG, Smith AMH, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre randomized controlled trail. Lancet. 2005;365:1718-1726. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2298] [Article Influence: 114.9] [Reference Citation Analysis (0)] |
| 3. | Lacy AM, Garcia-Valdecasas JC, Pique JM, Delgado S, Campo E, Bordas JM, Taurá P, Grande L, Fuster J, Pacheco JL. Short-term outcome analysis of a randomized study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc. 1995;9:1101-1105. [RCA] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 165] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | COLOR Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Dig Surg. 2000;17:617-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 115] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Fabozzi M, Allieta R, Contul RB, Grivon M, Millo P, Lale-Murix E, Nardi M. Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc. 2010;24:2085-2091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Senagore AJ, Delaney CP. A critical analysis of laparoscopic colectomy at a single institution: lessons learned after 1000 cases. Am J Surg. 2006;191:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Baća I, Perko Z, Bokan I, Mimica Z, Petricević A, Druzijanić N, Situm M. Technique and survival after laparoscopically assisted right hemicolectomy. Surg Endosc. 2005;19:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Kaiser AM, Kang JC, Chan LS, Vukasin P, Beart RW. Laparoscopic-assisted vs. open colectomy for colon cancer: a prospective randomized trial. J Laparoendosc Adv Surg Tech A. 2004;14:329-334. [PubMed] |
| 9. | Leung KL, Meng WC, Lee JF, Thung KH, Lai PB, Lau WY. Laparoscopic-assisted resection of right-sided colonic carcinoma: a case-control study. J Surg Oncol. 1999;71:97-100. [PubMed] |
| 10. | Lezoche E, Feliciotti F, Paganini AM, Guerrieri M, De Sanctis A, Minervini S, Campagnacci R. Laparoscopic vs open hemicolectomy for colon cancer. Surg Endosc. 2002;16:596-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 81] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Senagore AJ, Delaney CP, Brady KM, Fazio VW. Standardized approach to laparoscopic right colectomy: outcomes in 70 consecutive cases. J Am Coll Surg. 2004;199:675-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Edge SB, Byrd DR, Compton CC, Fritz AG. AJCC Cancer Staging Manual. 7th ed. Greene FL, Trotti A, editors. New York, NY: Springer 2010; 347-376. |
| 13. | Monson JRT, Young-Fadok TM, Nelson H. Invited editorial. Dis Colon Rectum. 2000;43:271-273. [DOI] [Full Text] |
| 14. | Bergamaschi R, Schochet E, Haughn C, Burke M, Reed JF 3rd, Arnaud JP. Standardized laparoscopic intracorporeal right colectomy for cancer: short-term outcome in 111 unselected patients. Dis Colon Rectum. 2008;51:1350-1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Hellan M, Anderson C, Pigazzi A. Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS. 2009;13:312-317. [PubMed] |
| 16. | Naitoh T, Tsuchiya T, Honda H, Oikawa M, Saito Y, Hasegawa Y. Clinical outcome of the laparoscopic surgery for stage II and III colorectal cancer. Surg Endosc. 2008;22:950-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Senagore AJ, Luchtefeld MA, Mackeigan JM. What is the learning curve for laparoscopic colectomy? Am Surg. 1995;61:681-685. [PubMed] |
| 18. | Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005;242:83-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 601] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 19. | Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, Köhler L, Bärlehner E, Köckerling F. Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc. 2001;15:116-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Bernstein MA, Dawson JW, Reissman P, Weiss EG, Nogueras JJ, Wexner SD. Is complete laparoscopic colectomy superior to laparoscopic assisted colectomy? Am Surg. 1996;62:507-511. [PubMed] |
| 21. | Franklin ME, Gonzalez JJ, Miter DB, Mansur JH, Trevino JM, Glass JL, Mancilla G, Abrego-Medina D. Laparoscopic right hemicolectomy for cancer: 11-year experience. Rev Gastroenterol Mex. 2004;69 Suppl 1:65-72. [PubMed] |
| 22. | Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2518] [Article Influence: 119.9] [Reference Citation Analysis (0)] |
| 23. | Baixauli J, Delaney CP, Senagore AJ, Remzi FH, Fazio VW. Portal vein thrombosis after laparoscopic sigmoid colectomy for diverticulitis: report of case. Dis Colon Rectum. 2003;46:550-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Chaves JA, Idoate CP, Fons JB, Oliver MB, Rodríguez NP, Delgado AB, Lizoain JL. [A case-control study of extracorporeal versus intracorporeal anastomosis in patients subjected to right laparoscopic hemicolectomy]. Cir Esp. 2011;89:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Scatizzi M, Kröning KC, Borrelli A, Andan G, Lenzi E, Feroci F. Extracorporeal versus intracorporeal anastomosis after right colectomy for cancer: A case-control study. World J Surg. 2010;268:743-746. [PubMed] |
| 26. | Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY. Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc. 2009;23:622-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |