Published online Jul 21, 2012. doi: 10.3748/wjg.v18.i27.3558
Revised: August 25, 2011
Accepted: August 31, 2011
Published online: July 21, 2012
AIM: To compare natural orifice transluminal endoscopic surgery (NOTES) vs standard laparoscopic ovariectomy in mini pigs with respect to technical aspects, complications and parameters of systemic inflammatory response.
METHODS: This was a randomized, experimental, survival study. Ten female mini pigs underwent NOTES transgastric ovariectomy (NOTES group) and ten female mini pigs underwent laparoscopic ovariectomy (LAP group). A “percutaneous endoscopic gastrostomy” approach with guidewire and sphincterotome was used for gastrotomy creation. The ovary was resected using standard biopsy forceps and a snare. The access site was closed using a “KING” closure with a single endoloop and several clips. In the laparoscopic group, a three-port laparoscopy and an ovariectomy were performed with the use of standard laparoscopic devices. C-reactive protein (CRP), white blood count and interleukin (IL)-6 plasma levels were used as indicators of systemic inflammatory response. All animals were euthanized 28 d after surgery.
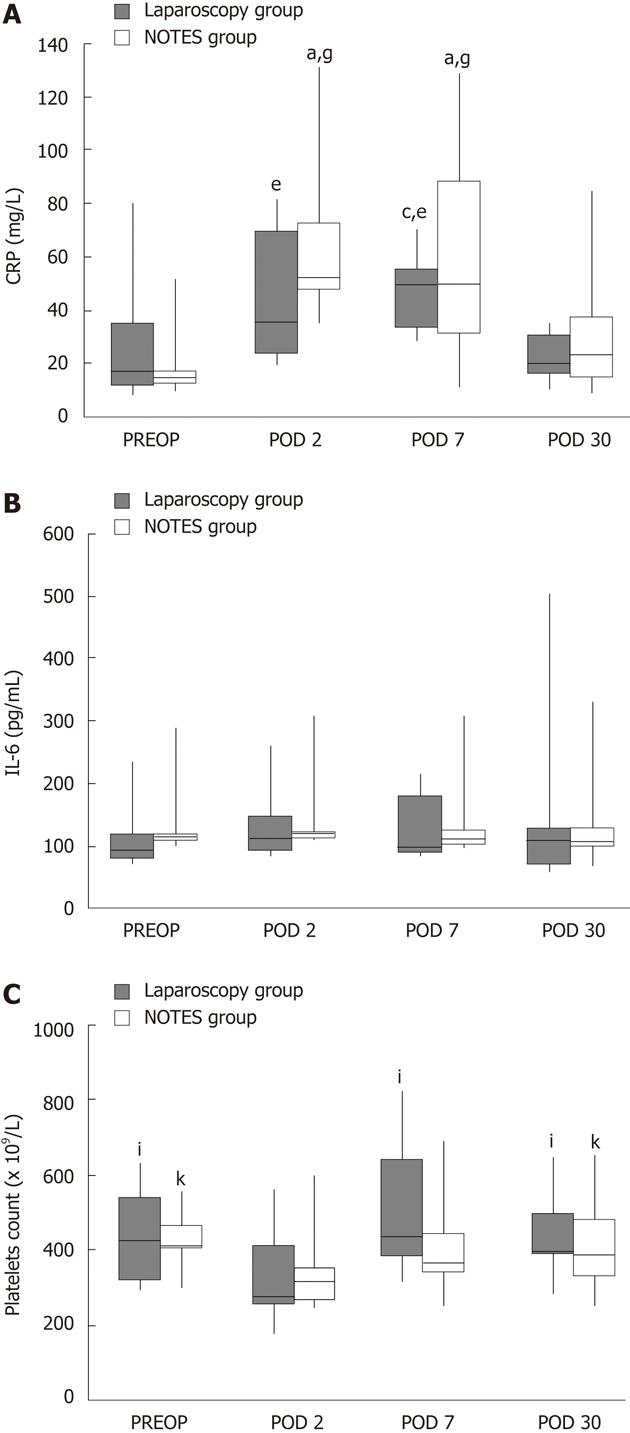
RESULTS: All animals survived without complications. The mean procedure time was 41.3 min ± 17.6 min (NOTES group) and 25.7 min ± 5.25 min (LAP group, P < 0.02). Postmortem examinations demonstrated that 50% and 70% of animals were free of any complications in the NOTES and LAP groups, respectively. The remaining animals developed minor complications (adhesions) in a comparable frequency between the two groups. In the NOTES group, one animal developed a small intramural gastric abscess close to the gastrotomy site. A minor serous exudate that was present in 50% and 40% of the animals in the NOTES and laparoscopy groups, respectively, was not considered a complication. In both groups CRP levels increased significantly on the 2nd and 7th postoperative days (POD) and returned to normal after 28 d. On POD 2, an increase of CRP level was significantly higher in the NOTES group compared to the LAP group. Values of IL-6 did not differ from baseline values in either of the groups postoperatively. Interestingly, the platelet count decreased significantly on POD 2, but returned close to baseline values on POD 7 and PODs 28-30.
CONCLUSION: Both NOTES and laparoscopic ovariectomies had a similar frequency of minor complications. However, the NOTES technique produced an increased systemic inflammatory response on POD 2.
- Citation: Martínek J, Ryska O, Filípková T, Doležel R, Juhas S, Motlík J, Holubová M, Nosek V, Rotnáglová B, Zavoral M, Ryska M. Natural orifice transluminal endoscopic surgery vs laparoscopic ovariectomy: Complications and inflammatory response. World J Gastroenterol 2012; 18(27): 3558-3564
- URL: https://www.wjgnet.com/1007-9327/full/v18/i27/3558.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i27.3558
Natural orifice transluminal endoscopic surgery (NOTES) is a surgical procedure that enables intraperitoneal surgical interventions with the elimination of abdominal wall incisions. The potential benefits of NOTES include no remnant scars and obviating the possibility of abdominal wall infection and hernia formation. Although several NOTES procedures have already been performed in humans[1], NOTES still remains an experimental surgical technique. Since laparoscopy serves as a golden standard for mini- invasive surgery, NOTES should be compared to laparoscopy in all imaginable aspects. If NOTES is to be used in the future, it must at least reach standards comparable to the existing procedures.
Several small experimental studies have compared NOTES with laparoscopic procedures. These included peritoneoscopy, transvaginal cholecystectomy, colon injury repair and distal pancreatectomy[2-6]. NOTES procedures were feasible but they usually lasted longer. Most studies found a comparable frequency of abdominal complications. Only a few studies tested the differences in systemic inflammatory response, however, no finding has ever suggested a clear difference between NOTES and laparoscopy[3,4,7]. Only one study found a potentially significant relative thrombocytopenia in NOTES as compared to laparoscopy during a simple peritoneoscopy[8].
The aim of our randomized experimental survival study was to compare both the outcome criteria (mortality, morbidity and complications such as peritonitis or adhesion formations) and indicators of postoperative systemic inflammatory response and platelet count in NOTES and laparoscopic ovariectomy in mini pigs. There is currently no data available comparing laparoscopic and NOTES experimental ovariectomy. In addition, ovariectomy can serve as a model for appendectomy from a technical point of view since pigs do not have an appendix. The main working hypothesis was the non-inferiority of NOTES to standard laparoscopic procedures.
Twenty female domestic mini pigs weighing between 10-31 kg were used for this study. Ten animals underwent a NOTES procedure and 10 animals underwent a laparoscopic procedure. The animals were randomly assigned to one of the two groups using a block randomization allowing an equal number of animals in each group.
Before the procedure, the animals were fed with a liquid diet for 2 d and consequently left fasting overnight. Premedication with Ketamine 10 mg/kg (Narkamon 1%, SPOFA, Czech Republic) and Atropine 0.2 mg (Atropine Biotica 0.5 mg, BB Pharma, Czech Republic) was given IM 30 min before the procedure. Oral intubation of the mini pigs was performed, a marginal ear vein cannula was placed and anesthesia was maintained using 1.5% isoflurane and fentanyl (3-5 mL/h). Antibiotics were administered neither before nor after the procedure.
The protocol was approved by The Committee for the Protection of Animals of The Czech Academy of Sciences and the experiment was performed in accordance with Act No. 246/1992.
All procedures were performed with a double-channel endoscope (GIF 2T160; Olympus Medical Co., Tokyo, Japan). The percutaneous endoscopic gastrostomy was used to gain access into the peritoneal cavity[9]. After transillumination, the stomach was punctured with a needle and the guidewire (Jagwire; Boston Scientific, Natick, Mass) was introduced through the needle into the stomach. The guidewire was then locked-in with a snare and pulled out through the endoscope. Consequently, the sphincterotome (KD-V411M-0330 Papillotome, Olympus Medical Co.) was introduced with the guidewire to the gastric wall. A gastric wall incision measuring approximately 15-20 mm was then performed with a tightened sphincterotome, and the endoscope was advanced into the peritoneal cavity. Afterwards, a brief exploration of the peritoneal cavity was performed with the endoscope.
Air was used for moderate insufflation, but intraperitoneal pressure was not measured during the procedure.
The ovary was then exposed and resected using both standard biopsy forceps and a snare with a coagulation current.
The endoscope with a resected ovary using a tightened snare was then pulled back to the stomach and the peritoneal cavity was completely desufflated. The desufflation was possible without reintroducing the scope into the abdominal cavity since a double-channel endoscope was used. After the ovary was withdrawn from the mouth, the endoscope was reintroduced for the gastric wall closure.
The gastric wall closure was performed with one endoloop (HX-400U-30 Aset PolyLoop Colo5; Olympus Medical Co.) and 4-5 clips. This technique provides a reliable full-thickness closure[10]. An open endoloop with a diameter of 30 mm (MAJ-340, Olympus Medical Co.) was fixed around the gastrotomy site with 4-5 clips (HX-610-90L, Olympus Medical Co.). A big endoscopic grasper (Olympus FG-48L, 026235, Olympus Medical Co.) was then advanced through an open endoloop. Both edges of the incision were grasped and pulled through the endoloop toward the endoscope. Subsequently, the endoloop was closed and released.
The laparoscopic group consisted of ten animals undergoing a standard three-trocar laparoscopic ovariectomy. After the induction of anesthesia, a pneumoperitoneum was established with CO2 using a standard laparoscopic insufflator. The insufflation pressure was set to 10 mmHg and gas flow was initiated. After pneumoperitoneum was established, the intra-abdominal pressure was monitored throughout the procedure. After the exposure of the fallopian tube, the ovary was resected using scissors with a monopolar coagulation current, and the ovary was grasped and withdrawn using grasping forceps. The pneumoperitoneum was evacuated and all skin incisions were closed with a single absorbable suture.
All pigs recovered well after extubation and were placed in an animal facility unit where they were monitored twice a day for any signs of complications, whether in feeding or in general well-being. All pigs resumed pig chow on the first postoperative day. Their survival was assessed on the 28-30th postoperative day, at which point the animals were euthanized and a necropsy was performed. The adhesions were assessed using the Adhesion Scoring Group system (none; minor = avascular, flimsy; major = dense and/or vascular or cohesive)[11].
Blood samples for the blood count, C-reactive protein (CRP)-levels, and interleukin 6 (IL-6) levels were taken before the procedure (15-60 min) and on days 2, 7 and 28-30 after the procedure. The blood count was analyzed immediately using a fully automatic hematology analyzer (Scil ABC Vet 16p, ABX Diagnostics, France). Blood samples for CRP and IL-6 analyses were centrifuged and plasma kept frozen (-80 °C) until the final analysis.
Both CRP and IL-6 were analyzed in duplicate with one control. A commercially available enzyme-linked immunosorbent assay kit Quantikine Porcine IL-6 Immunoassay (R and D Systems, Inc.) was used to measure IL-6 levels. The dynamic range of the assay was 39.1-2500 ng/L. An Immunoperoxidase Assay for Determination of C-Reactive Protein in Pig Samples (Gen Way Biotech, Inc.) was used for CRP level assessment. Its dynamic range was 6.25-200 μg/L. An analysis was performed according to the manufacturer’s instructions by a researcher blinded to the operative procedure.
For descriptive statistics, the data is presented as median values with appropriate percentiles. As all variables confirmed the normality and equal variance assumption, a Student t-test was performed for testing the differences between and within the groups. Binary variables (e.g., presence or absence of complications) were assessed with the Fisher exact test. Statistical significance was defined as a P-value of less than 0.05 and all P-values were two-sided. For multiple comparisons, a Bonferroni correction was used.
Access into the peritoneal cavity was gained within 3-7 min in all animals in the NOTES group. A peritoneoscopy did not show any injuries to adjacent organs. Seven right-sided and three left-sided ovariectomies were performed without major technical problems. All gastrotomies were successfully closed using the technique described above.
All laparoscopies were performed without major technical problems. Nine right-sided and one left-sided ovariectomies were performed.
The NOTES procedure took significantly longer than the laparoscopy procedure - medians were 42.5 min [interquartile (IQ) range: 30-45 min] vs 25 min (IQ range: 25-29 min), P = 0.02.
All animals had lived and had been fed normally without any clinical signs suggesting complications until they were euthanized. They gained the desirable weight after the procedure. At necropsy no signs of organ damage or peritonitis were discovered in either group. The gastrotomy site healed completely in all pigs. Only minor complications were found (minor adhesions and one small abscess) in similar frequencies in both groups (Table 1). A minor serous exudate that was present in 50% and 40% of the animals in the NOTES and laparoscopy groups, respectively, was not considered a complication.
White blood count and platelets: White blood count (WBC) had a tendency to increase after the procedure (on days 2 and 7 after the procedure) and to return to baseline values (on days 28-30) in both groups (Table 2). No significant differences were detected between the groups (Table 3).
| NOTES (n = 10) | Laparoscopy (n = 10) | |||||||
| Before | POD 2 | POD 7 | PODs 28-30 | Before | POD 2 | POD 7 | PODs 28-30 | |
| CRP (mg/L) | 14.5 (12-17) | 52.6 (47-73)ac | 51.8 (31-88)ac | 22.1 (14-38) | 16.1 (11-35) | 37.1 (23-70)c | 51.4 (33-55)c | 20 (16-31) |
| WBC (× 109/L) | 14.9 (14-17) | 19.6 (15-21) | 19.7 (17-23)a | 15.3 (15-20) | 18.3 (14-23) | 23.5 (19-24)c | 20 (18-26)c | 15.4 (14-18) |
| IL-6 (ng/L) | 108 (105-118) | 115 (110-121) | 110 (100-123) | 104 (97-129) | 92 (79-117) | 103.5 (90-146) | 98.6 (85-178) | 111 (67-130) |
| Platelets (× 109/L) | 414 (400-465) | 314 (261-351)ac | 366 (336-442) | 381 (325-479) | 424 (313-540) | 273 (253-412)ae | 433 (381-641) | 389 (382-498) |
| POD 2 | POD 7 | POD 28 | ||||
| NOTES | Laparoscopy | NOTES | Laparoscopy | NOTES | Laparoscopy | |
| CRP (%) | 288 (207-357) | 64 (4-172)a | 154 (70-436) | 172 (60-273) | 31.6 (3-193) | 25 [(-57)-76] |
| WBC (%) | 16 (0.3-43) | 21 [(-6)-66] | 34 (13-42) | 33 [(-8)-60] | 8 [(-0.3)-26] | -15 [(-23)-10] |
| IL-6 (%) | 3.7 (1.6-9) | 6 (3-15) | -1.6 [(-8)-0.9] | 6.6 (0.9-19) | -9.8 [(-21)-(-1.6)] | -6.7 [(-21)-44] |
| Platelets (%) | -23.5 [(-24)-(-13)] | -17.6 [(-35)-(-10)] | 1.5 [(-13)-19)] | 21 (9-30) | 2 [(-11)-7] | 3 [(-2)-12] |
CRP: CRP levels increased on days 2 and 7 after the procedure and returned close to the baseline values on day 28-30 (Table 2, Figure 1A). Changes in CRP levels were similar among the two groups on PODs 7 and 28. However, on POD 2, according to the diversion rate analysis, an increase of CRP level was significantly higher in the NOTES group compared to the LAP group (Table 3).
IL-6: No significant changes with respect to IL-6 within the groups or between the groups were discovered (Tables 2 and 3, Figure 1B).
Platelets: The platelet count decreased significantly on POD 2, but it returned close to baseline values on POD 7 and PODs 28-30. The values of platelet count on POD 2 were, however, not dangerously low from a clinical point of view (Tables 2 and 3, Figure 1C).
Currently NOTES still represents an experimental surgical technique. If NOTES is to be introduced into clinical practice, it must show advantages in comparison with commonly available procedures. One of the potential advantages of NOTES is a “scar-less” surgery, whilst other real advantages are more or less speculative. Since laparoscopy is a golden standard for several surgical procedures, NOTES should be compared to laparoscopy in different experimental settings.
Given the potential advantages of the NOTES method in comparison with the classical laparoscopic techniques, our survival experimental study compared a standard laparoscopic ovariectomy with a NOTES ovariectomy in a sample of mini pigs. At the moment, there are no studies comparing NOTES and laparoscopic techniques involving ovariectomy.
All procedures were performed without any significant technical problems. The NOTES procedure lasted longer than the laparoscopy. However, the duration of the fastest NOTES procedure was 18 min, which was very close to the time of the fastest laparoscopic ovariectomy (14 min). Most studies comparing NOTES with laparoscopy also showed a better technical feasibility of laparoscopy[5,6]. This can be explained by the absence of appropriate equipment currently available for NOTES. We believe that an improvement of technical performance would reflect the implementation of new “NOTES” equipment.
Apart from the procedure duration, no significant differences between the two techniques regarding any other outcome criteria were found. All animals survived without any clinical signs of complications. At necropsy only minor adhesions were found in a small number of pigs in both groups. One pig in the NOTES group developed a small intramural abscess next to the gastrotomy site. This complication was most likely related to our otherwise safe gastric-closure technique rather than the NOTES procedure itself. Importantly, there were no signs of peritonitis in either group. Based on this finding, NOTES is not an inferior procedure to laparoscopy with respect to main outcome criteria despite lower aseptic conditions (an endoscope cannot be sterile as opposed to laparoscopic equipment), the absence of antibiotics administration and the absence of disinfection of the gastric lumen. Similar outcome criteria were used in several other studies comparing NOTES with laparoscopy[2,4-8,12]. A majority of these studies did not show significant differences between the two techniques regarding the frequency of major complications. This involved procedures such as peritoneoscopy[2,3,7,8], transvaginal cholecystectomy[4], colon injury repair[5], salpingectomy[12] and distal pancreatectomy[6].
However, in some cases the occurrence of adhesions or histological peritonitis was higher in NOTES as opposed to laparoscopy[2,13]. The slightly higher frequency of adhesions or intraperitoneal infections is possibly related to the quality of the access site closure. Safe closure is thus considered a prerequisite for any study comparing NOTES with laparoscopy. For example, von Renteln et al[14] showed a higher frequency of infectious complications, including one fatal case of peritonitis with an incomplete gastrotomy closure using endoclips. In our study a single-loop and clips technique providing full-thickness closure was used.
In order to assess the physiological impact of NOTES compared to laparoscopic surgery, changes in interleukin-6 levels, white-blood cells, platelet count and CRP levels were analyzed. IL-6 has been extensively studied as an indicator demonstrating a lower invasiveness of laparoscopy in comparison to open surgery[15-17]. IL-6 alterations have been directly correlated to the operation duration[15]. IL-6 levels culminate 24 h after surgery and its serum level increases later than the serum level of other cytokines (tumor necrosis factor-α and IL-1β). It also remains longer in circulation. This cytokine was hence chosen for the purpose of our study.
No significant changes with respect to IL-6 values were detected in either group. Furthermore, no increase in IL-6 levels after either procedure was observed. It can be argued that measuring IL-6 levels on POD 2 is too late to detect such an increase. Freeman et al[18] showed a peak serum concentration of IL-6 levels 2 h after NOTES ovariectomy in dogs. IL-6 levels returned to baseline values within 18 h. The possible explanation for this increase is that the procedures lasted an average of 157 min, which is considerably more than in our study. Other studies investigating IL-6 levels showed elevated levels even on POD 5 in a group of patients undergoing laparoscopic colorectal resection or laparoscopic cholecystectomy[19,20]. On the other hand, Fan et al[4] did not show any significant changes with regard to IL-6 levels after transvaginal cholecystectomy on PODs 1 and 2. Their study, though, was rather small with only 2 pigs in the laparoscopic control group.
We did not assess the peritoneal inflammatory response as measured by IL-6 levels in the peritoneal fluid. It has been demonstrated that the degree of such a response correlated with the extent of adhesions[2,13]. Since we detected similar occurrence of adhesions in both groups we did not expect to find a differing local inflammatory response.
Several studies have investigated the way in which laparoscopic surgery affects the acute-phase response by assessing CRP. CRP-levels have been found to be elevated in a majority of laparoscopic procedures as late as on POD 14[21,22]. In agreement with these findings, we observed an increase in CRP-levels on POD 2 and 7 in our laparoscopic group. CRP-levels returned to the baseline values on PODs 28-30. In the NOTES group a quite similar behavior in CRP response was found. We detected a significantly higher increase of CRP levels in the NOTES group compared to the LAP group on POD 2; however, on POD 7 this difference was no longer present. This suggests that an inflammatory response in the NOTES procedure is not lower than that in the LAP group.
An increase of WBC after both laparoscopic and NOTES peritoneoscopy on PODs 2 and 7 has been reported[8], however, no significant changes in WBC were found after the same procedure in another study[7]. In our study, only an insignificant trend in WBC increase on PODs 2 and 7 was observed in both groups.
Bingener et al[8] showed relative thrombocytopenia after NOTES peritoneoscopy but not after standard laparoscopy. In contrast, we found a decrease in platelet count in both groups on POD 2. However, the decrease was not clinically significant. The explanation for this phenomenon is unclear. Bingener thought that the possible reason for his finding was heparin-induced thrombocytopenia. In our study no heparin was used (for the flushing of invasive monitoring lines) as in the study conducted by Bingener. It cannot be excluded that thrombocytopenia in the porcine environment occurred due to a bacterial infection[23]. A possible explanation could also be the Stage II of Systemic Inflammatory Response when small quantities of local cytokines are released into circulation to improve the local response. This leads to a stimulation of the growth factor and the recruitment of macrophages and platelets. We believe that the phenomenon of a decreasing platelet count in the NOTES procedure should be addressed in further studies.
There are several limitations to our study. Primarily, it is a study conducted on animals. The clinical implications and applicability of these findings in human medicine are unclear.
Secondly, the use of an infant animal model in a limited number is also a significant limitation when translating results into practice. The limited number of animals cannot exclude a type II error when interpreting our results. Thirdly, intraperitoneal pressure was not measured systematically and also microbiological contamination was not assessed. Also, for the NOTES procedures we used room air for insufflations, while for laparoscopic procedures we used a standard carbon dioxide insufflation. This could, theoretically, have influenced the results regarding the higher CRP levels in the NOTES group. Finally, IL-6 levels were not measured on the first day after the procedure.
In conclusion, both NOTES ovariectomy and laparoscopic ovariectomy were performed without any major technical problems and both were accompanied by a similar frequency of minor complications. However, the NOTES technique produced an increased systemic inflammatory response on POD 2 in comparison to the laparoscopic technique.
The methods of laparoscopic and standard open surgery are currently the commonly used procedures. Natural orifice transluminal endoscopic surgery (NOTES) is an experimental surgical technique whereby “scar-less” abdominal operations can be performed with an endoscope passing through a natural orifice (mouth, anus, etc.) and then through an internal incision in the stomach or rectum. Although some NOTES procedures have already been performed on humans (e.g., transvaginal cholecystectomy), NOTES remains an experimental method.
Several NOTES procedures have been examined and studied in experimental studies-NOTES peritoneoscopy, cholecystectomy, colon injury repair, etc.Should NOTES be implemented into clinical practice, it must be compared to the current surgical standards (laparoscopy and open surgery). The authors compared the technical feasibility, complications, and indicators of postoperative systemic inflammatory response in an experimental study.
The authors found that NOTES ovariectomy is not an inferior procedure to the standard laparoscopic ovariectomy in terms of technical feasibility and frequency of complications, although the NOTES procedure lasted significantly longer. The postoperative systemic inflammatory response was mild, almost identical to laparoscopy. However, C-reactive protein increase on postoperative day 2 was significantly higher in the NOTES group as compared to the laparoscopy group.
The study shows the feasibility of the NOTES procedures in the experimental setting. This is the first research study that compares laparoscopic and NOTES ovariectomy procedures and that provides evidence to the similarity between both of them. In other words, the study shows no inferiority of the NOTES ovariectomy as compared to laparoscopy with regard to the majority of variables.
This is a rarity of published works in the literature concerning natural orifice transluminal endoscopic surgery versus laparoscopy. The manuscript is well structured. NOTES is a challenging topic for recent minimal invasive surgery. This experimental study claimed that NOTES had similar effects with laparoscopy for ovariectomy.
Peer reviewers: George Sgourakis, MD, PhD, FACS, 2nd Surgical Department and Surgical Oncology Unit, Red Cross Hospital, 11 Mantzarou Str., Neo Psychiko, 15451 Athens, Greece; Cuneyt Kayaalp, MD, Professor, Department of General Surgery, Staff Surgeon of Gastrointestinal Surgery, Turgut Ozal Medical Center, Inonu University, Malatya 44315, Turkey
S- Editor Lv S L- Editor Rutherford A E- Editor Xiong L
| 1. | Santos BF, Hungness ES. Natural orifice translumenal endoscopic surgery: progress in humans since white paper. World J Gastroenterol. 2011;17:1655-1665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Trunzo JA, McGee MF, Cavazzola LT, Schomisch S, Nikfarjam M, Bailey J, Mishra T, Poulose BK, Lee YJ, Ponsky JL. Peritoneal inflammatory response of natural orifice translumenal endoscopic surgery (NOTES) versus laparoscopy with carbon dioxide and air pneumoperitoneum. Surg Endosc. 2010;24:1727-1736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | McGee MF, Schomisch SJ, Marks JM, Delaney CP, Jin J, Williams C, Chak A, Matteson DT, Andrews J, Ponsky JL. Late phase TNF-alpha depression in natural orifice translumenal endoscopic surgery (NOTES) peritoneoscopy. Surgery. 2008;143:318-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Fan JK, Tong DK, Ho DW, Luk J, Law WL, Law S. Systemic inflammatory response after natural orifice translumenal surgery: transvaginal cholecystectomy in a porcine model. JSLS. 2009;13:9-13. [PubMed] |
| 5. | Romagnuolo J, Morris J, Palesch S, Hawes R, Lewin D, Morgan K. Natural orifice transluminal endoscopic surgery versus laparoscopic surgery for inadvertent colon injury repair: feasibility, risk of abdominal adhesions, and peritoneal contamination in a porcine survival model. Gastrointest Endosc. 2010;71:817-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Willingham FF, Gee DW, Sylla P, Kambadakone A, Singh AH, Sahani D, Mino-Kenudson M, Rattner DW, Brugge WR. Natural orifice versus conventional laparoscopic distal pancreatectomy in a porcine model: a randomized, controlled trial. Gastrointest Endosc. 2009;70:740-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Bingener J, Krishnegowda NK, Michalek JE. Immunologic parameters during NOTES compared with laparoscopy in a randomized blinded porcine trial. Surg Endosc. 2009;23:178-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Bingener J, Michalek J, Van Sickle K, Schwesinger W. Randomized blinded trial shows relative thrombocytopenia in natural orifice translumenal endoscopic surgery compared with standard laparoscopy in a porcine survival model. Surg Endosc. 2008;22:2067-2071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Kantsevoy SV, Jagannath SB, Niiyama H, Isakovich NV, Chung SS, Cotton PB, Gostout CJ, Hawes RH, Pasricha PJ, Kalloo AN. A novel safe approach to the peritoneal cavity for per-oral transgastric endoscopic procedures. Gastrointest Endosc. 2007;65:497-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Ryska O, Martinek J, Dolezel R, Filipkova T, Juhas S, Juhasova J, Zavoral M, Tuckova I, Ryska M. Feasibility of a novel single loop-and-clip gastrotomy closure (‘King’s closure’) after NOTES procedures in an experimental study. Gastroenterology and Hepatology. 2011;65:207-210. |
| 11. | Corson SL, Batzer FR, Gocial B, Kelly M, Gutmann JN, Maislin G. Intraobserver and Interobserver Variability in Scoring Laparoscopic Diagnosis of Pelvic Adhesions. J Am Assoc Gynecol Laparosc. 1994;1:S8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Hucl T, Benes M, Kocik M, Krak M, Maluskova J, Kieslichova E, Oliverius M, Spicak J. A novel double-endoloop technique for natural orifice transluminal endoscopic surgery gastric access site closure. Gastrointest Endosc. 2010;71:806-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Ramamoorthy SL, Lee JK, Luo L, Mintz Y, Cullen J, Easter DW, Savu MK, Chock A, Carethers J, Horgan S. The inflammatory response in transgastric surgery: gastric content leak leads to localized inflammatory response and higher adhesive disease. Surg Endosc. 2010;24:531-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | von Renteln D, Vassiliou MC, Rothstein RI. Randomized controlled trial comparing endoscopic clips and over-the-scope clips for closure of natural orifice transluminal endoscopic surgery gastrotomies. Endoscopy. 2009;41:1056-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 15. | Vittimberga FJ, Foley DP, Meyers WC, Callery MP. Laparoscopic surgery and the systemic immune response. Ann Surg. 1998;227:326-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 205] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Joris J, Cigarini I, Legrand M, Jacquet N, De Groote D, Franchimont P, Lamy M. Metabolic and respiratory changes after cholecystectomy performed via laparotomy or laparoscopy. Br J Anaesth. 1992;69:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 207] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Cho JM, LaPorta AJ, Clark JR, Schofield MJ, Hammond SL, Mallory PL. Response of serum cytokines in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 1994;8:1380-1383; discussion 1380-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Freeman LJ, Rahmani EY, Sherman S, Chiorean MV, Selzer DJ, Constable PD, Snyder PW. Oophorectomy by natural orifice transluminal endoscopic surgery: feasibility study in dogs. Gastrointest Endosc. 2009;69:1321-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Wichmann MW, Hüttl TP, Winter H, Spelsberg F, Angele MK, Heiss MM, Jauch KW. Immunological effects of laparoscopic vs open colorectal surgery: a prospective clinical study. Arch Surg. 2005;140:692-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 132] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 20. | Glaser F, Sannwald GA, Buhr HJ, Kuntz C, Mayer H, Klee F, Herfarth C. General stress response to conventional and laparoscopic cholecystectomy. Ann Surg. 1995;221:372-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 130] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Ohzato H, Yoshizaki K, Nishimoto N, Ogata A, Tagoh H, Monden M, Gotoh M, Kishimoto T, Mori T. Interleukin-6 as a new indicator of inflammatory status: detection of serum levels of interleukin-6 and C-reactive protein after surgery. Surgery. 1992;111:201-209. [PubMed] |
| 22. | Bolufer JM, Delgado F, Blanes F, Martínez-Abad M, Canos JI, Martín J, Oliver MJ. Injury in laparoscopic surgery. Surg Laparosc Endosc. 1995;5:318-323. [PubMed] |
| 23. | Bautista MJ, Ruiz-Villamor E, Salguero FJ, Sánchez-Cordón PJ, Carrasco L, Gómez-Villamandos JC. Early platelet aggregation as a cause of thrombocytopenia in classical swine fever. Vet Pathol. 2002;39:84-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |