INTRODUCTION
Currently, total stomach resection is typically performed in adults with stomach cancer[1-9]. Other causes of total stomach resection include chemical burns of the digestive tract caused by the consumption of toxic, most often caustic, substances, which occurs accidentally in children and in adults who have attempted suicide[10]. Most recent studies describe burns in the upper part of the digestive tract occurring after the consumption of concentrated acids, pesticides and bases used as detergents, bleachers or rust-removers[11-13]. Drug poisonings usually cause symptoms in the central nervous system and the circulatory and respiratory systems as well as bleeding because they most often involve the ingestion of soporific, psychotropic and cardiac medicines. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used in treatments globally. In some countries, e.g., in the United States, NSAIDs are used protractedly and in large doses, particularly in elderly patients. The administration of NSAIDs involves the risk of complications occurring in the digestive tract. It has been shown that these medicines may damage mucous membranes in the stomach and induce complications such as ulcerations, hemorrhages, or perforations[14-17]. The aim of the article is to present a female patient who consumed a very large amount of NSAIDs and Tramal at the same time in a suicide attempt.
CASE REPORT
A 54-year-old female was admitted to the General Surgery Department of the University Hospital in Olsztyn from the Internal Medicine Department to undergo surgical treatment of a pylorus narrowing that was induced by the consumption of drugs in a suicide attempt. Approximately five months before that, the woman took 60 NSAID pills (including Ibuprom, Ketonal, Diklofenak, Aspirin) and also ingested 300 mg of Tramal. After that episode, she was treated at the intensive care unit and then at the department of internal diseases. During that time, the patient was fed parenterally and, later, also enterally. Prior to that incident, the woman had not been treated for coexisting diseases such as rheumatoid arthritis or depression. At the time of admission to the surgery department, the patient reported epigastric pain with nausea and vomiting with mucous content as well as the inability to consume food orally. Despite parenteral and enteral feeding, the patient exhibited a 16-kg drop in body mass. Upon admission to the surgery department, her weight was 59 kg. The patient also suffered from pain in the epigastric and umbilical regions. However, the belly was soft with no pathological resistance, and the liver was not enlarged. Biochemical examinations showed minimal anemia (hemoglobin 10.4 g/dL) and increased fibrinogen values (up to 479 mg%) at international normalized ratio 1.10. During gastroscopy, a very small stomach was noticeably covered by scars and numerous fibrin-covered ulcerations. The stomach lacked a mucous membrane and hemorrhaged when touched with the device. The length of the stomach in the upper region was 2-3 cm. The distal part of the stomach was excessively narrowed and inaccessible. The pylorus channel allowed only for the insertion of the Flokar Ch10/130 cm catheter, which was placed properly behind the ligament of Treitz, with resistance. The histopathologic examination of a sample taken from the stomach revealed the existence of necrotic and inflammatory masses with granulation. The patient was qualified to undergo surgery operational treatment. A very small, infiltrated stomach with an initial section of duodenum was identified intraoperatively. Those organs exhibited excessive inflammatory infiltration. There were also numerous enlarged lymphatic glands, which were removed. After preparation and total resection of the stomach (Figure 1) with the initial part of the duodenum, a Roux-Y anastomosis was performed using a 25-mm circular stapler. The esophageal resection line was 10 mm and free from pathological changes; the esophagus was observed to have intact epithelium and stroma with dispersed inflammatory infiltration. The initial duodenum resection line was 12-mm long with a preserved margin of mucous membrane and chronic exacerbated inflammation in the mucous and submucosal membranes. Histopathologic examination of the stomach revealed a deep, chronic and exacerbated inflammatory condition with an extensive ulceration over the entire length, reaching up to the pylorus. Microscopic examination revealed numerous lymphatic glands with inflammatory changes (Figures 2 and 3). The post-operative period was complicated on the fifth day due to bile leakage from the part of the duodenum closed with a linear stapler. A relaparotomy revealed numerous adhesions, as well as an orifice, 2 mm in diameter, on the top of the closed, bloated duodenum stump, approximately 10 mm from the stitch line, out of which bile flowed heavily. Through the orifice, a drain of the same diameter was introduced into the duodenum as a duodenostomy. Four days after the surgery, the patient was treated with a respirator. On the following days, apart from some non-edemic and inflammatory changes in the lower segments of the lungs, the course of treatment was satisfactory. The patient was fed parenterally and enterally through a Flocare-type tube. When performing control examinations, the drain was removed from the duodenum stump (14th day). On the 16th day, the patient was administered an oral diet that was extended gradually. On the 21st day, she was discharged from the hospital, in good general condition, with body mass of 61.5 kg.
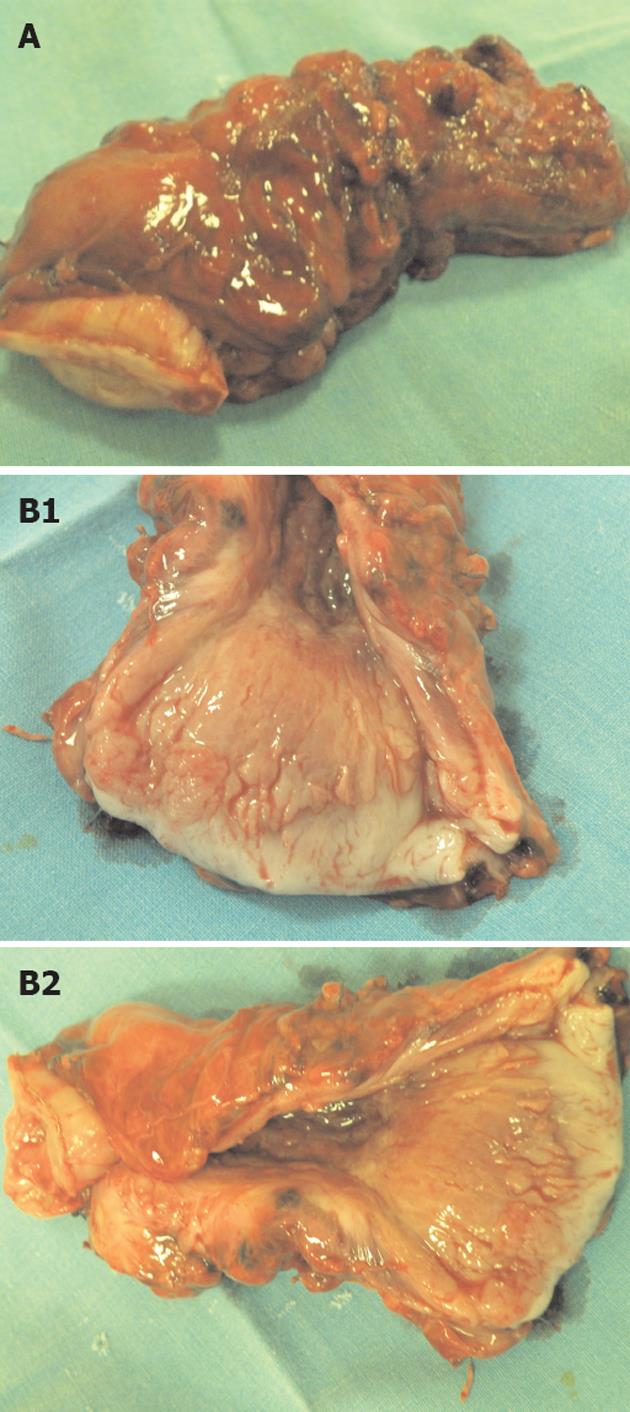
Figure 1 Pathological changes in atrophic gastritis after treatment.
A: Tubular resected stomach as a whole, 9 cm long; B1 and B2: Cross-section of stomach with its 2 cm thick wall and its atrophic mucose membrane.
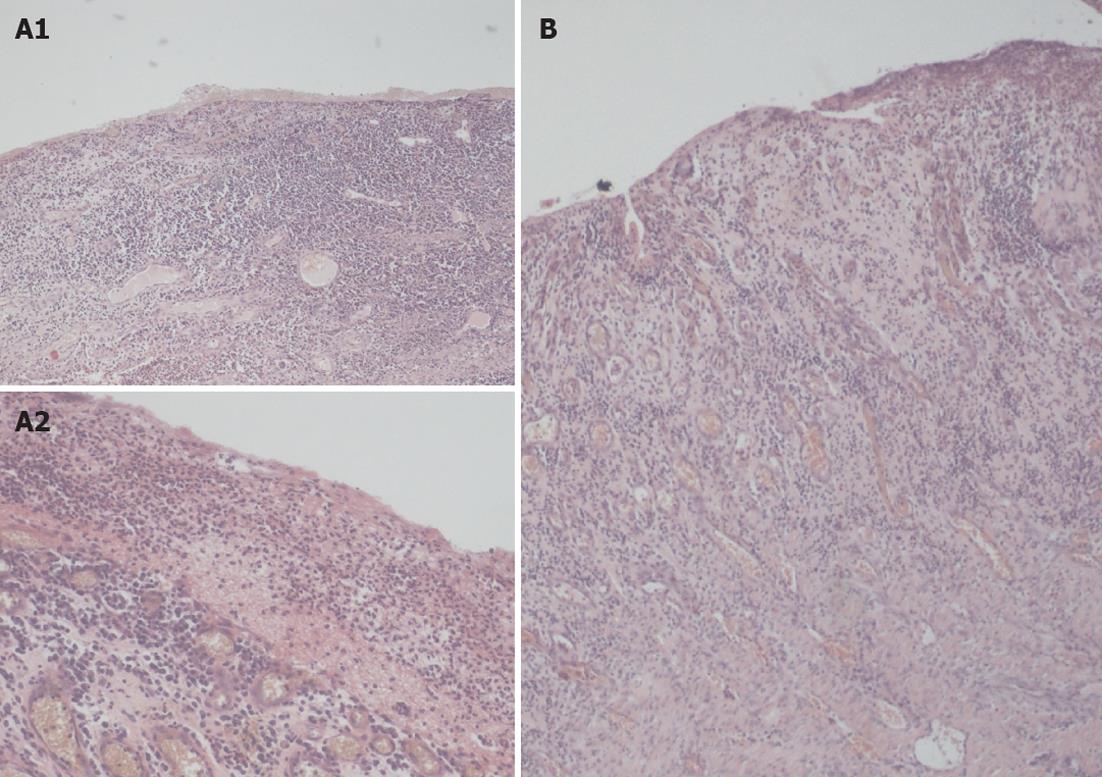
Figure 2 Representative photomicrographs of hematoxylin and eosin stained sections from the stomach’s necrosis of submucous membrane.
A: The inflammatory infiltration of the submucosal membrane of stomach (A1 magnitude 40× and A2 magnitude 100×); B: The ulceration-granulation in the stomach’s submucosal membrane, magnitude 40×.
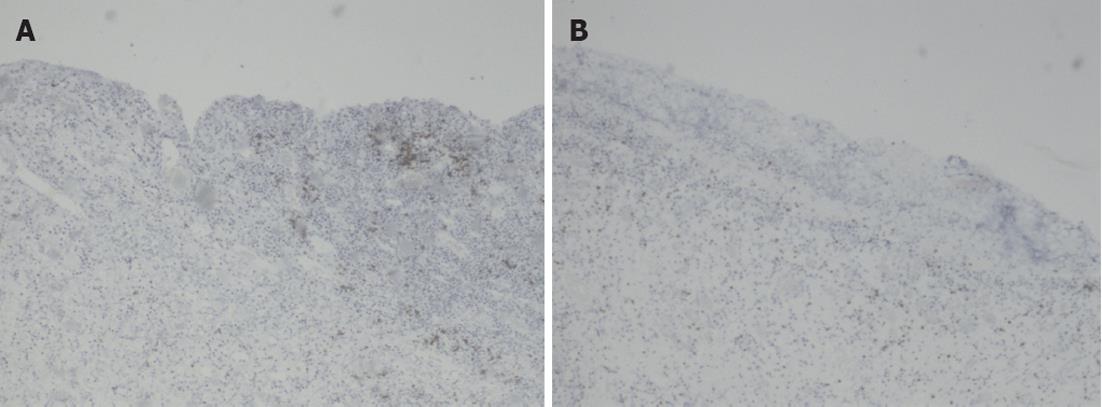
Figure 3 Representative photomicrographs sections from the stomach (magnitude 40×).
A: The large, transmural inflammatory cell infiltration of submucosal membrane CD3 (+); B: Mixed inflammatory cell infiltrations CD3 (+).
DISCUSSION
Benzodiazepines and other psychotropic drugs are the most common causes of suicide-related drug poisoning. Few studies have examined suicide attempts that involve NSAID overdoses. The long-term administration of NSAIDs, even in therapeutic doses, results in digestive tract complications in the form of inflammation, ulceration, mucous membrane bleeding and hemorrhage as well as perforations to the stomach and duodenum[14-17]. The consumption of NSAIDs in larger amounts causes damage to the stomach’s mucous membrane, even resulting in total necrosis, as observed in the current case. During the six-month-long feeding treatment of the patient and her endoscopic observation at the Department of Internal Medicine, preparations were made for surgery. The patient was in poor psychological condition and did not agree to undergo surgery. Within the borders of the stomach and duodenum, inflammatory infiltrate almost completely closed the pylorus with numerous adhesions to the surrounding tissues. The mucous membrane had slipped down completely, and its place was taken by necrotic and inflammatory tissues. It has already been proven that high doses of acetylsalicylic acid increase the risk of hemorrhage during the course of peptic ulcer disease[18]. In the current case, there was no information related to the adverse effects of NSAIDs administered to patients with osteoarthritis. When patients overdose for suicidal reasons, the duration of contact between the mucous membrane and the caustic substance is long, as in the case of our patient. The exposure time, type of drug (e.g., hydrophilic properties), concentration in the stomach, contents of the stomach before drug consumption, degree of pylorus contraction and operations performed on the digestive tract that impair its motor activity are of crucial importance with respect to the level of damage and the extent of changes to the stomach. The morphological changes to the stomach upon consumption of large amounts of NSAIDs may be accompanied by damage to the liver, kidneys and heart[17,19]. Nelson et al[20] described a case of liver failure requiring transplantation and simultaneous intestinal necrosis upon consumption of large amounts of acetaminophen and ibuprofen by their schizophrenic patient. The toxic activity of those drugs damages the mucous membrane and stops the production of prostaglandins in the intestines. A massive hemorrhage from a duodenum or stomach ulcer may often be observed among patients who have consumed NSAIDs even in therapeutic doses[21,22]. Morphological changes in the digestive tract are usually described in the literature as liquefactive or coagulative necrosis but refer to poisonings with concentrated bases or acids. Regardless of the type of poison consumed orally, chronic ulcerations of the stomach’s mucous membrane, excessive inflammation, clots in the micro-circulation, bacterial colonization and increased fibroblastic activity may develop. The toxic activity of any drug depends not only on the consumed dose but also on other circumstances. Having a meal, drinking alcohol, and the ingestion of other medicines influences the patient’s clinical condition. Most often, oral poisonings cause changes to the upper part of the digestive tract and lead to damage to the liver and kidneys. The current literature lacks reports on total resection of the stomach due to poisoning with NSAIDs and Tramal.