Published online May 14, 2012. doi: 10.3748/wjg.v18.i18.2219
Revised: December 22, 2011
Accepted: March 9, 2012
Published online: May 14, 2012
AIM: To compare the recurrent bleeding after endoscopic injection of different epinephrine volumes with hemoclips in patients with bleeding peptic ulcer.
METHODS: Between January 2005 and December 2009, 150 patients with gastric or duodenal bleeding ulcer with major stigmata of hemorrhage and nonbleeding visible vessel in an ulcer bed (Forrest IIa) were included in the study. Patients were randomized to receive a small-volume epinephrine group (15 to 25 mL injection group; Group 1, n = 50), a large-volume epinephrine group (30 to 40 mL injection group; Group 2, n = 50) and a hemoclip group (Group 3, n = 50). The rate of recurrent bleeding, as the primary outcome, was compared between the groups of patients included in the study. Secondary outcomes compared between the groups were primary hemostasis rate, permanent hemostasis, need for emergency surgery, 30 d mortality, bleeding-related deaths, length of hospital stay and transfusion requirements.
RESULTS: Initial hemostasis was obtained in all patients. The rate of early recurrent bleeding was 30% (15/50) in the small-volume epinephrine group (Group 1) and 16% (8/50) in the large-volume epinephrine group (Group 2) (P = 0.09). The rate of recurrent bleeding was 4% (2/50) in the hemoclip group (Group 3); the difference was statistically significant with regard to patients treated with either small-volume or large-volume epinephrine solution (P = 0.0005 and P = 0.045, respectively). Duration of hospital stay was significantly shorter among patients treated with hemoclips than among patients treated with epinephrine whereas there were no differences in transfusion requirement or even 30 d mortality between the groups.
CONCLUSION: Endoclip is superior to both small and large volume injection of epinephrine in the prevention of recurrent bleeding in patients with peptic ulcer.
-
Citation: Ljubicic N, Budimir I, Biscanin A, Nikolic M, Supanc V, Hrabar D, Pavic T. Endoclips
vs large or small-volume epinephrine in peptic ulcer recurrent bleeding. World J Gastroenterol 2012; 18(18): 2219-2224 - URL: https://www.wjgnet.com/1007-9327/full/v18/i18/2219.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i18.2219
Peptic ulcer disease accounts for 50% to 70% of cases of acute nonvariceal upper gastrointestinal bleeding (UGIB)[1,2]. Initial haemostatic rates of 80% to almost 100% can be achieved with various endoscopic techniques. However, after initial control, bleeding recurs in 10% to 30% of patients[3].
Among various endoscopic techniques a recent International consensus on nonvariceal UGIB recommends combination therapy with clear statement that epinephrine injection alone provides suboptimal efficacy and should be used in combination with another methods[4]. However, several recent studies found injection of a large volume of epinephrine to be superior to injection of a small epinephrine volume with respect to recurrent bleeding from peptic ulcer[5,6]. Since epinephrine injection is effective (initial hemostasis obtained with epinephrine injection range from 85% to 100%), safe, inexpensive and technically easy, the concept of a beneficial effect of large volumes of epinephrine in preventing recurrent ulcer bleeding seems to be very challenging. Therefore, the aim of this prospective study was to compare the rates of recurrent bleeding after endoscopic injection of two different volumes of an epinephrine solution (15-25 mL vs 30-40 mL) with endoscopic placement of hemoclips in patients with peptic ulcer bleeding. Since it has been suggested that the useful baseline factor for stratification in UGIB trials may be stigmata of hemorrhage in an ulcer, we decided to include in the study only patients presenting with acute UGIB and endoscopically proven gastric or duodenal ulcer with visible vessel in an ulcer bed (Forrest IIa)[7].
Between January 2005 and December 2009, consecutive patients presenting with acute UGIB were considered for this study. These patients were referred to the Emergency Unit of the Department of Internal Medicine at the “Sestre milosrdnice” University Hospital, Zagreb, Croatia and then if necessary hospitalized at the Interventional Gastroenterology Unit at the same hospital.
UGIB was suspected if hematemesis, melena or hematochezia were seen and/or bloody nasogastric aspirate was observed. In all those patients upper gastrointestinal endoscopy was performed within 6 h of hospital admission. Patients were included only if emergency endoscopy disclosed a gastric or duodenal bleeding ulcer with major stigmata of hemorrhage (“coffee ground” material or blood in the stomach and/or duodenum) and nonbleeding visible vessel in an ulcer bed (Forrest IIa)[8]. Exclusion criteria were as follows: major comorbid or terminal illness that made endoscopy hazardous; inability or unwillingness to consent to endoscopy and endoscopic therapy; gastric malignancy; minor stigmata of hemorrhage at endoscopy such as oozing from ulcer borders without a visible vessel, flat-pigmented spots, or clean ulcer base. Patients with gastric and duodenal ulcer with either an actively bleeding vessel (spurting or oozing; Forrest I), or adherent clot (Forrest IIb) were also excluded.
Endoscopy was performed with standard upper endoscopes (GIF Q140 and GIF Q160, Olympus Optical Co., Japan). Endotherapy was carried out by the well-trained endoscopists, each with at least five years experience in the treatment of patients with GI bleeding. Endoscopic characteristics, including ulcer localization, ulcer size, and type of stigmata, were recorded (Endobase, Olympus, Japan).
Possible complications of endoscopic treatment and complete study protocol were discussed with patients and their relatives, and written informed consent was obtained before endoscopy and entry into the trial. The ethics committee of our hospital approved the treatment protocol. Randomization of eligible patients was carried out at the time of endoscopy by an individual uninvolved with the procedure who opened sealed numbered envelopes containing treatment assignments generated with a computer randomization program. The treatment group allocation was then communicated to the endoscopist in the endoscopy suite. Patients were randomized to a small-volume epinephrine group (15 to 25 mL injection group; Group 1), a large-volume epinephrine group (30 to 40 mL injection group; Group 2) and a hemoclip group (Group 3). In the small-volume epinephrine group (Group 1) 15 to 25 mL of a 1:10 000 solution of epinephrine was injected around the visible vessel (2-4 mL/injection at 2-3 mm from the visible vessel). In the large-volume epinephrine group (Group 2), 30-40 mL of a 1:10 000 solution of epinephrine was injected around the visible vessel at the ulcer bed as in the small-volume epinephrine group. Mechanical hemostasis was performed with stainless steel hemoclips (Olympus, Japan) as has been previously described[9,10]. During endoscopy and endotherapy, electrocardiographic monitoring was used to detect arrhythmias.
Once hemostasis was achieved the bleeding site was observed for at least 10 min and it was assessed by water irrigation at maximal pressure. Failure of the initial hemostasis has been defined if any hemorrhage occurred immediately (within 10 min) after initial endoscopic hemostasis. In these patients crossing over to the other treatment group was not allowed. In all patients two biopsy specimens were taken from the gastric antrum and body, and the presence of Helicobacter pylori (H. pylori) infection was assessed by histopathological examination of the specimens. In patients with gastric ulcer in whom recurrent bleeding was not observed, control endoscopy was performed 4 d to 5 d after initial hemostasis and biopsy specimens were obtained from the margins and base of gastric ulcers to exclude malignancy.
After initial endoscopic hemostasis, patients were hospitalized and cared for by a physician who was blinded to the endoscopic treatment that had been delivered. Vital signs were monitored hourly whereas blood counts were observed every 6 h for the first 48 h and every 12 h to 24 h thereafter. All patients were given acid suppressive therapy: pantoprazole 80 mg iv, (bolus) and then 40 mg iv, every 8 h for at least 48 h, followed by 40 mg daily by mouth, or esomeprazole 80mg iv, (bolus) and then 40 mg iv, every 8 h for at least 48 h, followed by 20 mg once a day by mouth. Shock was defined as a systolic blood pressure of less than 90mmHg with symptoms or signs of organ hypoperfusion.
Recurrent bleeding was defined as one or more signs of ongoing bleeding, including fresh hematemesis or melena, hematochezia, aspiration of fresh blood via nasogastric tube, instability of vital signs, and a reduction of Hb by more than 2 g/dL over a 24 h period (early recurrence) or over a 7 d period (late recurrence) after initial stabilization of puls, blood pressure and Hb concentration. If recurrent bleeding was suspected, endoscopy was performed immediately. If “coffee ground” material or blood in the stomach and/or duodenum has been found together with active bleeding or a fresh blood clot in the ulcer base were found, recurrent bleeding was considered confirmed. For ethical reasons, additional endoscopic methods for treatment of recurrent bleeding were discussed with patients and their relatives and therapeutic option in all patients with recurrent bleeding was hemoclip application. Patients in whom endoscopic treatment or retreatment was unsuccessful underwent emergency surgery.
The rate of recurrent bleeding, as the primary outcome, was compared between the groups of patients included in the study. Secondary outcomes compared between the groups were primary hemostasis rate (defined as the absence of hemorrhage occurred immediately after initial endoscopic hemostasis), permanent hemostasis (defined as the absence of recurrent bleeding within the 30 d period after initial or secondary endoscopic hemostasis), need for emergency surgery, 30 d mortality and bleeding-related deaths, length of hospital stay, and transfusion requirements.
Base on assumption that injection of a large-volume epinephrine decreased the expected rate of recurrent bleeding from 17.1% after injection of small-volume epinephrine solution to zero, 39 patients would have been needed in each group for a power of 80% and a significance level of 0.05[6].
Continuous data were summarized as mean [95% confidence interval (CI)]. The Student t test was used to compare the mean values of continuous variables. The Pearson chi-square test and the Fisher exact test were used when appropriate for the comparison of categorical variables. All analyses were performed with a statistical package (SPSS for Windows, United States). A P values less than 0.05 were regarded as statistically significant.
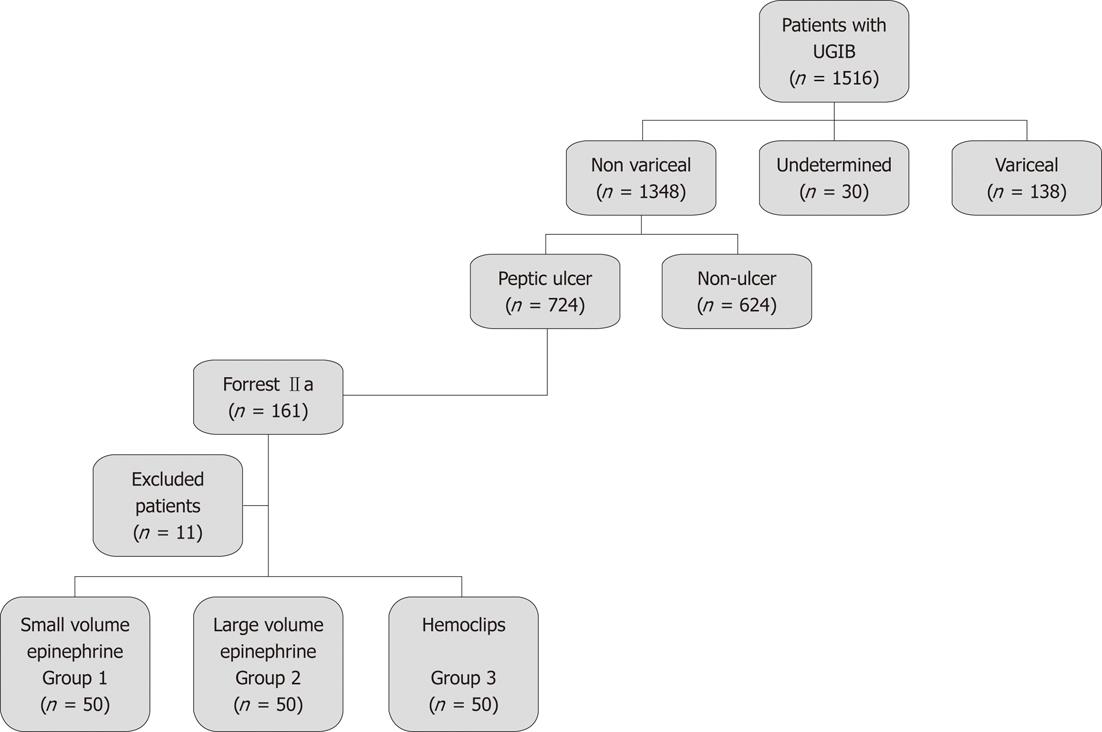
From January 2005 to December 2009, 150 patients were included in this study; they were randomly assigned to receive small-volume (15 to 25 mL) injection of epinephrine (Group 1, n = 50), large-volume (30 to 40 mL) injection of epinephrine (Group 2, n = 50), and hemoclip (Group 3, n = 50). During the same period a total of 1516 patients with UGIB were encountered; of these 47.8% had gastric or duodenal bleeding ulcer, 41.2% had non-ulcer lesions (acute erosive gastropathy, portal hypertensive gastropathy, malignancy, Mallory-Weiss tear, angiomata, Dieulafoy’s lesion), 9.1% had esophageal or gastric variceal bleeding, and 1.9% had no source of bleeding (Figure 1). Among the 161 patients with UGIB and endoscopically proven peptic ulcer with visible vessel (Forrest IIa), randomly assigned to receive small-volume or large-volume of epinephrine, or hemoclip, 11 patients were excluded because they refused to participate in the study.
Clinical and endoscopic data obtained for patients included in the study are outlined in Table 1. There were no significant differences between the groups with respect to age, gender, ulcer size and location, positive H. pylori status, NSAID or alcohol consumption, shock, bleeding stigmata, history of previous peptic ulcer or peptic ulcer bleeding, comorbid diseases or hemoglobin and hematocrit levels at admission.
| Group 1(n = 50) | Group 2 (n = 50) | Group 3 (n = 50) | |
| Age (yr) | 68 (40-96) | 61 (30-92) | 67 (40-94) |
| Gender (M/F) | 31/19 | 33/17 | 34/16 |
| Location of ulcer | |||
| Stomach | 26 (52) | 23 (46) | 28 (56) |
| Duodenum | 24 (48) | 27 (54) | 22 (44) |
| Ulcer size (cm) | |||
| < 2 | 36 (72) | 44 (88 ) | 37 (74) |
| ≥ 2 | 14 (28) | 6 (12) | 13 (26) |
| Gastric content | |||
| Blood | 19 (38) | 22 (44) | 21 (42) |
| Coffee ground | 31 (62) | 28 (56) | 29 (58) |
| Shock | 4 (8) | 2 (4) | 1 (2) |
| Hb level (g/dL) | 9.3 (3.9-14.7) | 9.0 (3.6-14.2) | 9.4 (5.6-14.3) |
| Comorbid disease | 36 (72) | 35 (70) | 33 (60) |
| NSAIDs | 15 (30) | 23 (46) | 29 (58) |
| Alcohol consumption | 20 (40) | 23 (46) | 30 (60) |
| Smoker’s | 12 (24) | 16 (32) | 10 (20) |
| Previous ulcer disease | 14 (28) | 10 (20) | 11 (22) |
| Previous ulcer bleeding | 12 (24) | 10 (20) | 8 (16) |
Clinical outcome data are summarized in Table 2. Initial hemostasis was obtained in all patients. In the small-volume epinephrine group (Group 1) the mean volume of epinephrine injected was 19.1 mL (range, 16 to 25 mL) whereas in the large-volume epinephrine group (Group 2) the mean volume of epinephrine injected was 37.9 mL (range, 30 to 40 mL). Among patients endoscopically treated with hemoclips (Group 3), multiple clips (up to three) were needed in majority of cases with a median of 1.6 clips per patient.
| Group 1 | Group 2 | Group 3 | |
| Primary outcome | |||
| Early recurrent bleeding | 15 (30) | 8 (16) | 2 (4)cb |
| Stigmata | |||
| Spurting | 4 (26.7) | 1 (12.5) | 1 (50) |
| Oozing | 5 (33.3) | 2 (25) | 1 (50) |
| Visible vessel | 6 (40) | 5 (62.5) | 0 |
| Secondary outcomes | |||
| Initial hemostasis | 50 (100) | 50 (100) | 50 (100) |
| Permanent hemostasis | 44 (88) | 46 (92) | 48 (96) |
| Emergency surgery | 6 (12) | 4 (8) | 2 (4) |
| 30-d mortality | 3 (6) | 0 (0) | 4 (8) |
| Blood transfusion (mL) | 1041 (120-1997) | 912 (0-2039) | 840 (0-1893) |
| Hospital stays (d) | 7.5 (1-14) | 7.6 (1-15) | 5.7(1-15)bd |
The rate of early recurrent bleeding was 30% (15/50) in the small-volume epinephrine group (Group 1) and 16% (8/50) in the large-volume epinephrine group (Group 2); the difference did not reach statistical significance (P = 0.09). The rate of recurrent bleeding was 4% (2/50) in the hemoclip group (Group 3); the difference was statistically significant with regard to patients treated with either small-volume or large-volume epinephrine solution (P = 0.0005 and P = 0.045, respectively). Late recurrent hemorrhage was not observed in our patients. With regard to ulcer location and ulcer size as well, there were no significant differences in the rate of early recurrent bleeding between the groups. Also, there were no differences in transfusion requirement or even 30 d mortality between the groups. However, duration of hospital stay was significantly shorter among patients treated with hemoclips than among patients treated with epinephrine (Table 2). There was no bleeding-related death or procedure-related death. Three patients from Group 1 (causes of death were colon malignancy in one patient, cardiac failure in one patient, and obstructive pulmonary disease with pneumonia in one patient) and four patients from Group 3 died (pulmonary embolism in two patients and myocardial infarction in one patient). Among patients from Group 2 no one died. One patient in whom large-volume injection of the epinephrine solution was administered (35 mL) required emergent surgery because of a perforation.
Of the 15 patients in the small-volume epinephrine group (Group 1), eight patients in the large-volume epinephrine group (Group 2), and two patients in the hemoclip group (Group 3) who had recurrent bleeding, all were treated with hemoclips. Emergency surgery was performed in all patients in whom re-treatment with hemoclips did not produce hemostasis: six patients from group 1, three patients from Group 2, and two patients from Group 3. Majority of patients in whom emergency surgery has been performed had duodenal ulcer located on the duodenal bulb posterior wall (Group 1, 5/6; Group 2, 2/3; Group 3, 3/3, respectively). Successful permanent hemostasis was not statistically different among groups of patients (Table 2).
Therapeutic efficacy of the small-volume epinephrine vs large-volume epinephrine and hemoclips is given in Table 3. Small-volume vs large-volume epinephrine was not significant in NNT benefit prediction, although small-volume epinephrine (NNT = 4) and large-volume epinephrine (NNT = 9) showed different significant benefits concerning hemoclip treatment.
| Recurrent bleeding rate (%) | RRR (%) | ARR (%) | NNT |
| Small-volume vs large-volume epinephrine | 46.6 (-11.2-75.0) | 14.0 (-2.6-30.3) | 8.0 (37.7-3.3) |
| Small-volume epinephrine vs hemoclips | 86.7 (51.7-96.5) | 26.0 (12.3-40.4) | 4.0 (2.5-8.1) |
| Large-volume epinephrine vs hemoclips | 75.0 (9.0-23.0) | 12.0 (0.2-25.0) | 9.0 (4.0-476.0) |
There were no procedure-related cardiovascular complications in the three groups. Electrocardiographic monitoring did not record any serious cardiac arrhythmia except of occasional sinus tachycardia and isolated supraventricular extrasystoles observed among all patients treated with large-volume epinephrine injection. The number of patients who complained of epigastric pain during and/or immediately after the procedure of endotherapy was significantly higher in the large-volume epinephrine group (34/50) than in the small-volume epinephrine (3/50) or hemoclips (2/50) groups (P < 0.001).
Emergency endoscopy is accepted as the method of choice in the early identification and treatment of a bleeding peptic ulcer[10]. A variety of endoscopic hemostatic methods have been developed and all were found to be similarly effective[3,11]. Epinephrine as the most commonly used agent for endoscopic injection therapy has been demonstrated to be effective for initial hemostasis but appears less effective in preventing further bleeding than other monotherapies, and definitely is less effective than epinephrine followed by a second modality such as sclerosant or a thermal contact device[4,12]. However, when the analysis was restricted to studies that used routine second-look endoscopy with re-treatment of high-risk stigmata, epinephrine injection was not found to be less effective than other monotherapies or epinephrine followed by second modality[12]. On the other hand, limited data indicate that injection of a large volume epinephrine seems to be superior to injection of a small epinephrine volume with respect to recurrent bleeding[5,6,13]. These studies suggested local tamponade is the major effect in sustained hemostasis and that injection of larger volumes of epinephrine may be beneficial in preventing recurrent bleeding by prolonging the hemostatic effect of mechanical compression. Lin et al[5] demonstrated that injection of a large volume (13-20 mL) of epinephrine can reduce the rate of recurrent bleeding in patients with high-risk peptic ulcer and is superior to injection of lesser volumes (5-10 mL) of epinephrine (15.4% vs 30.8%). Park et al[6] reported that injection of 35 to 45 mL of a epinephrine solution was more effective in preventing recurrent bleeding than an injection of 15 to 25 mL of the same solution (0% vs 17.1%). Similar results have been found by Liou et al[13,14] demonstrated that injection of a large volume (30 to 40 mL) of epinephrine significantly reducing the rebleeding rate in patients with active bleeding ulcer.
The current study clarifies the low value of endoscopic injection therapy with epinephrine alone in patients with peptic ulcer bleeding showing major stigmata of hemorrhage (patients with endoscopically proven peptic ulcer with a visible vessel in an ulcer bed; Forrest IIa). Disparities in inclusion criteria using Forrest classification, across the majority of studies that demonstrated higher effectiveness of large volume diluted epinephrine injection significantly limit the interpretation of those results. Unlike many mentioned studies, this trial was carried out on adequate patient’s sample with clearly predefined groups of patients.
Our results have clearly shown that endoscopic therapy with hemoclip represents safe and effective method, superior to both, small-volume (15 to 25 mL) and large-volume (30 to 40 mL) injection of diluted epinephrine in the prevention of early recurrent bleeding from peptic ulcer. Reduction in recurrent hemorrhage rates observed among our peptic ulcer patients treated with hemoclip method positively affected length of hospital stay, reflecting the possibility of significant cost savings.
It has been postulated that possible mechanisms that underlie hemostasis in response to endoscopic injection of diluted epinephrine are vasoconstriction, vessel compression, and platelet aggregation[15,16]. Among these, mechanical compression of the bleeding vessel is the most important factor with respect to initial hemostasis[6,16]. Therefore, it has been assumed that injection of larger volumes of diluted epinephrine may be beneficial in preventing recurrent peptic ulcer bleeding by prolonging the hemostatic effect of mechanical effect and compression[5,6,14]. Despite the fact that previously mentioned assumption has been indirectly confirmed by several studies demonstrating a significantly lower rate of recurrent peptic ulcer bleeding following large volume epinephrine injection, we strongly believe that even sustained mechanical compression achieved by a larger volumes of diluted epinephrine injection is not sufficiently sustained to produce vessel compression that will last enough to provoke platelet aggregation in a greater extent, that would finally result vessel thrombosis. The results observed in this study indicate that local tamponade observed even after larger volumes of diluted epinephrine injection was not effective as hemoclip for the preventing of recurrent bleeding. This observation strongly suggested that vessel compression, produced by a hemoclip has an important role in the mechanisms involved in vessel occlusion, thus preventing the recurrent bleeding.
To our knowledge, this is the first prospective randomized study comparing the rates of the recurrent bleeding after endoscopic injection of two different volumes of an epinephrine solution and mechanical endoscopic method in patients with UGIB and endoscopically proven peptic ulcer with nonbleeding visible vessel in an ulcer bed (Forrest IIa). Our results have confirmed that endoclip is safe and effective method, pointing out to its superiority to both, small volume and large volume injection of diluted epinephrine in the prevention of early recurrent bleeding from peptic ulcer.
Peptic ulcer disease accounts for 50% to 70% of cases of acute nonvariceal upper gastrointestinal bleeding (UGIB). Initial haemostatic rates of 80% to almost 100% can be achieved with various endoscopic techniques, but, after initial control, bleeding recurs in 10% to 30% of patients. Several recent studies found injection of a large volume of epinephrine to be superior to injection of a small epinephrine volume with respect to recurrent bleeding from peptic ulcer. Since epinephrine injection is effective (initial hemostasis obtained with epinephrine injection range from 85% to 100%), safe, inexpensive and technically easy, the concept of a beneficial effect of large volumes of epinephrine in preventing recurrent ulcer bleeding seems to be very challenging.
To compare the rates of recurrent bleeding after endoscopic injection of two different volumes of an epinephrine solution (15-25 mL vs 30-40 mL) with endoscopic placement of hemoclips in patients with acute peptic ulcer bleeding and endoscopically proven gastric or duodenal ulcers with visible vessel in an ulcer bed (Forrest IIa).
This is the first prospective randomized study comparing the rates of the recurrent bleeding after endoscopic injection of two different volumes of an epinephrine solution and mechanical endoscopic method in patients with UGIB and endoscopically proven peptic ulcer with nonbleeding visible vessel in an ulcer bed (Forrest IIa). Unlike many studies, this trial was carried out on adequate patient’s sample with clearly predefined groups of patients, in a unique center. A detailed description is provided to allow other investigators to reproduce or validate.
The results provide sufficient experimental evidence to draw firm scientific conclusions. The results have clearly shown that endoscopic therapy with hemoclip represents safe and effective method, superior to both, small-volume (15 to 25 mL) and large-volume (30 to 40 mL) injection of diluted epinephrine in the prevention of early recurrent bleeding from peptic ulcer. Reduction in recurrent hemorrhage rates observed among our peptic ulcer patients treated with hemoclip method positively affected length of hospital stay, reflecting the possibility of significant cost savings.
This is the paper in which authors compere two most commonly used hemostatic methods in patients with bleeding peptic ulcer. The sample size is adequate, in a unique center. A detailed description is provided to allow other investigators to reproduce or validate. The statistical methods used are appropriate. The results provide sufficient experimental evidence or data to draw firm scientific conclusions. The discussion is well organized and provide systematic theoretical analyses and valuable conclusions.
Peer reviewer: Javier San Martin, MD, Gastroenterology and Endoscopy, Sanatorio Cantegril, Av. Roosevelt y P 13, Punta del Este 20100, Uruguay
S- Editor Gou SX L- Editor A E- Editor Zheng XM
| 1. | Di Fiore F, Lecleire S, Merle V, Hervé S, Duhamel C, Dupas JL, Vandewalle A, Bental A, Gouerou H, Le Page M. Changes in characteristics and outcome of acute upper gastrointestinal haemorrhage: a comparison of epidemiology and practices between 1996 and 2000 in a multicentre French study. Eur J Gastroenterol Hepatol. 2005;17:641-647. [PubMed] |
| 2. | Enestvedt BK, Gralnek IM, Mattek N, Lieberman DA, Eisen G. An evaluation of endoscopic indications and findings related to nonvariceal upper-GI hemorrhage in a large multicenter consortium. Gastrointest Endosc. 2008;67:422-429. [PubMed] |
| 3. | Barkun AN, Martel M, Toubouti Y, Rahme E, Bardou M. Endoscopic hemostasis in peptic ulcer bleeding for patients with high-risk lesions: a series of meta-analyses. Gastrointest Endosc. 2009;69:786-799. [PubMed] |
| 4. | Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair P. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101-113. [PubMed] |
| 5. | Lin HJ, Hsieh YH, Tseng GY, Perng CL, Chang FY, Lee SD. A prospective, randomized trial of large- versus small-volume endoscopic injection of epinephrine for peptic ulcer bleeding. Gastrointest Endosc. 2002;55:615-619. [PubMed] |
| 6. | Park CH, Lee SJ, Park JH, Park JH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. Optimal injection volume of epinephrine for endoscopic prevention of recurrent peptic ulcer bleeding. Gastrointest Endosc. 2004;60:875-880. [PubMed] |
| 7. | Laine L, Spiegel B, Rostom A, Moayyedi P, Kuipers EJ, Bardou M, Sung J, Barkun AN. Methodology for randomized trials of patients with nonvariceal upper gastrointestinal bleeding: recommendations from an international consensus conference. Am J Gastroenterol. 2010;105:540-550. [PubMed] |
| 8. | Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet. 1974;2:394-397. [PubMed] |
| 9. | LJubicic N, Supanc V, Vrsalovic M. Efficacy of endoscopic clipping for actively bleeding peptic ulcer: comparison with polidocanol injection therapy. Hepatogastroenterology. 2004;51:408-412. [PubMed] |
| 10. | Ljubicic N. Efficacy of endoscopic clipping and long-term follow-up of bleeding Dieulafoy's lesions in the upper gastrointestinal tract. Hepatogastroenterology. 2006;53:224-227. [PubMed] |
| 11. | Gralnek IM, Barkun AN, Bardou M. Management of acute bleeding from a peptic ulcer. N Engl J Med. 2008;359:928-937. [PubMed] |
| 12. | Laine L, McQuaid KR. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol. 2009;7:33-47; quiz 1-2. [PubMed] |
| 13. | Liou TC, Lin SC, Wang HY, Chang WH. Optimal injection volume of epinephrine for endoscopic treatment of peptic ulcer bleeding. World J Gastroenterol. 2006;12:3108-3113. [PubMed] |
| 14. | Liou TC, Chang WH, Wang HY, Lin SC, Shih SC. Large-volume endoscopic injection of epinephrine plus normal saline for peptic ulcer bleeding. J Gastroenterol Hepatol. 2007;22:996-1002. [PubMed] |
| 15. | O'brien JR. Some effects of adrenaline and anti-adrenaline compounds on platelets in vitro and in vivo. Nature. 1963;200:763-764. [PubMed] |
| 16. | Randall GM, Jensen DM, Hirabayashi K, Machicado GA. Controlled study of different sclerosing agents for coagulation of canine gut arteries. Gastroenterology. 1989;96:1274-1281. [PubMed] |